ED Wait Times in Greenville: Get The Facts
When care is most needed, ECU Health is always here. Our focus on our mission – improving the health and well-being of eastern North Carolina – is at the heart of all we do, and our doors are always open.
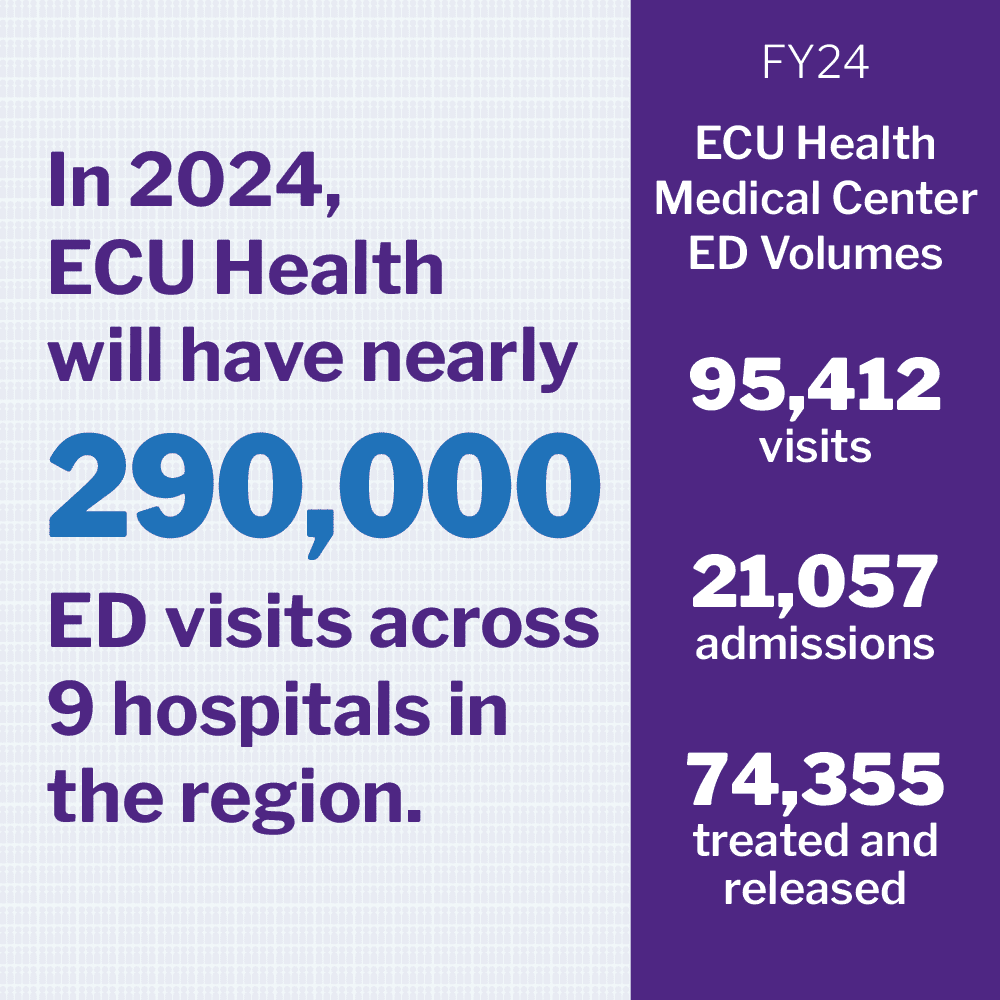
ECU Health’s mission and the complex realities we face in our underserved rural region is most evident in the nine emergency departments across the region, which collectively treat more than 290,000 community members annually. Our teams are actively implementing innovative solutions to help ensure we deliver life-saving care daily. Still, not every patient we treat in the emergency department faces a life-threatening illness. In fact, patients come to us with a wide spectrum of health concerns – from heart attacks to headaches, to behavioral health challenges and everything in between.
Our obligation and responsibility is to care for every patient, though depending on your condition, there may be a wait. Patients with most serious conditions such as heart attacks, strokes and traumatic injuries, must be treated first. While long wait times for patients who are less sick can be frustrating, we are working every day to improve our processes and treat as many patient as possible.

To better understand the unique challenges of emergency care in our region, there are a few things to know about eastern North Carolina, emergency departments, and how we are working on solutions with our communities on solutions.
What is an Emergency Department?
An Emergency Department (ED) is a hospital facility that provides immediate care for patients with conditions that require medical attention. EDs are staffed 24/7.
EDs are required to assess all patients upon entry. This is part of a federal requirement, known as the Emergency Medical Treatment & Labor Act (EMTALA). Patients cannot be turned away even if their symptoms/conditions do not constitute a medical emergency.
When a patient arrives at the ED, they are triaged to determine the severity of their condition. Triage is based on the patient’s vital signs, symptoms and complaints, and patients are categorized into five levels:
- Level 1: Immediate, life-threatening
- Ex. cardiac arrest, major trauma and severe respiratory distress.
- Level 2: Emergency, could be life-threatening
- Ex. cardiac-related chest pain, asthma attack and altered mental status.
- Level 3: Urgent
- Ex. abdominal pain, high fever with cough and persistent headache.
- Level 4: Semi-urgent
- Ex. simple laceration, rabies vaccination and sore throat.
- Level 5: Non-urgent
- Ex. low appetite, ear and skin problems and general minor discomfort.
Patients with life-threatening or severe conditions are treated immediately, while those with less urgent conditions may have to wait in a designated area. Typically, around 30% of ED patients have a condition that requires them to be admitted to a hospital. The rest are treated and released.
ECU Health Medical Center: One of the busiest hospitals in the nation
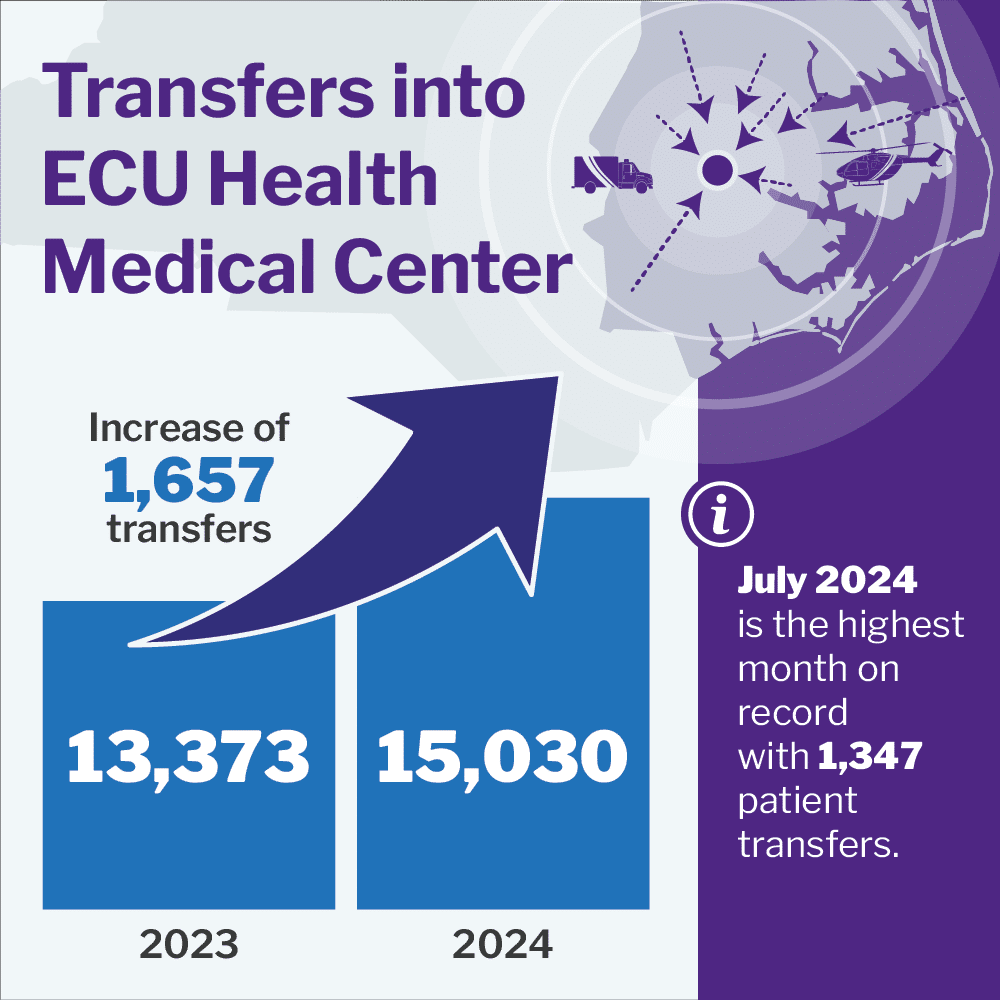
ECU Health Medical Center is one of the busiest hospitals in the nation serving more than 95,000 patients in 2024 with more than 21,000 of those patients admitted for care. Across the region, ECU Health’s Transfer Center fields 27,000 calls per month to find hospital placement for patients needing care. Simply put, the increasing need for services across eastern North Carolina puts immense pressure on emergency departments.
This high volume of ED patients further strains space and licensed bed limitations. Consider that ECU Health Medical Center has 974 beds while at the same time operating full capacity for 174 days in the last fiscal year. That means community demand is more than our licensed beds nearly half of the year. In the ED, this results in longer wait times for patients who need placement.
Why can ED wait times be so long?
It is no secret that overcrowding in emergency departments is a challenge facing hospitals across the country. ECU Health Medical Center, the only Level I Trauma Center in ECU Health’s 29 county service area, is no exception. The Medical Center cares for a largely underserved rural region where access to care is difficult for many. This includes primary care, behavioral health care and other services provided in outpatient settings. Combined with a disproportionate number of uninsured community members, this lack of access to care means more and more patients are using – or being told to use – the emergency department for primary care and routine care needs. Some patients believe it is faster or more convenient for them. Others simply lack access to primary care resources.
EDs are federally required by EMTALA to assess all patients upon entry. Patients cannot be turned away even if their symptoms/conditions do not constitute a medical emergency. Patients with life-threatening or severe conditions are treated immediately, while those with less urgent conditions may have to wait in a designated area.
Unnecessary use of the ED delays care for everyone. Patients with life threatening needs are seen first, but as new patients come into the ED for non-emergent care, the wait gets longer. Patient understanding of what constitutes an emergency can be different from clinically defined emergencies which can cause frustrations.
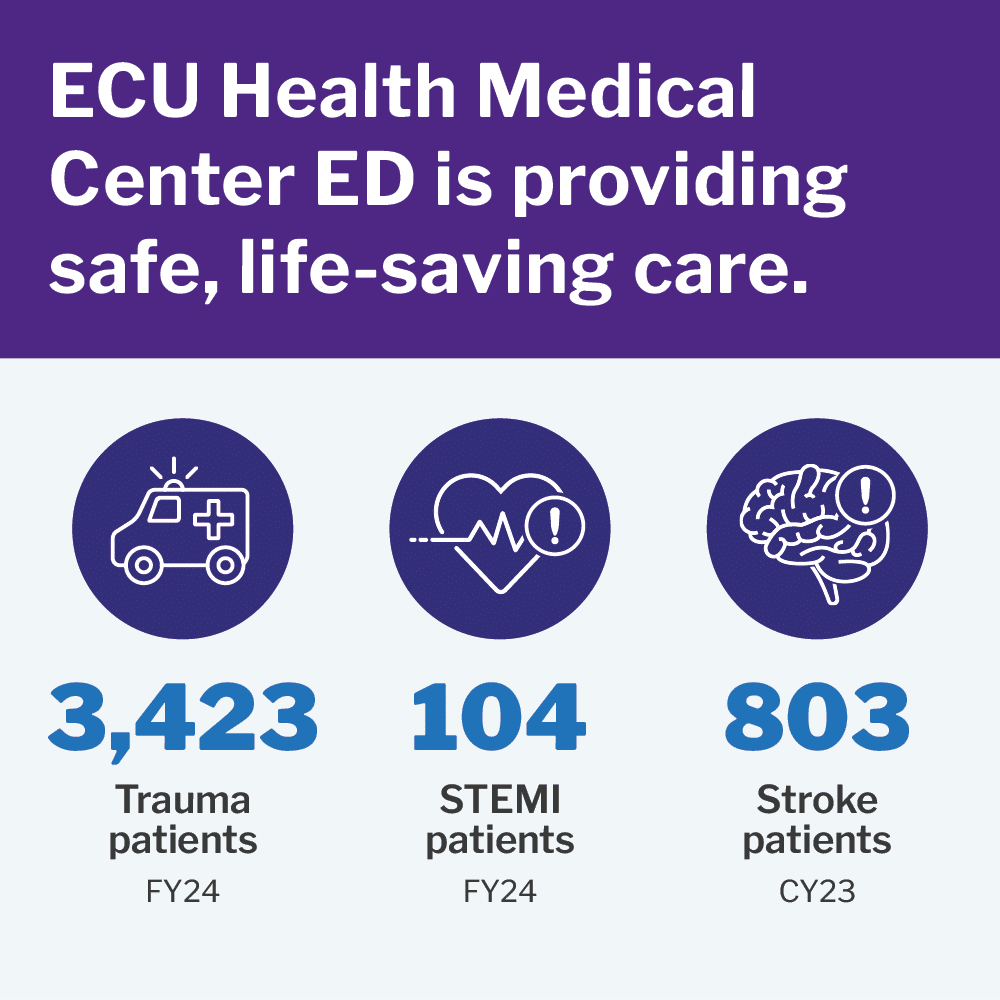
Despite these challenges, ECU Health still delivers high-quality, life-saving care.
ECU Health Medical Center is a teaching hospital and Level I Trauma Center which means it provides both community care and care to critically ill, highly complex patients from across the region.
While those visiting our ED for non-emergent care are likely to wait for an extended time before being seen, there is no delay for those who need life-saving care. Take, for example, patients who suffer from a stroke. Time is the most critical factor for stroke care.
Across ECU Health, code strokes in the ED have grown steadily from 195 in 2016 to 803 in 2023. Despite this increase, clot-busting tissue plasminogen activator (tPA) response times outperform the national benchmarks:
- 100% patients received tPA within 60 minutes (vs goal 85%)
- 89% patients received tPA within 45 minutes (vs goal 75%)
- 61% patients received tPA within 30 minutes (vs goal 50%)
ECU Health Medical Center’s emergency department is also unique in that it has a truly multidisciplinary team of physicians, providers and nurses who help bring unique expertise to a unique population of patients. This includes a large pediatric emergency medicine faculty provider group of eight academic providers, three certified toxicologists and more.
What is ECU Health doing to reduce wait times and serve more patients at the Medical Center?
ECU Health has launched several efforts to help reduce wait times in the Medical Center ED. These have resulted in a 12.5% reduction in time it takes for a patient to see a provider from FY22 to FY24. Additionally, ECU Health Medical Center, despite historic volumes, decreased the length of stay and improved our discharge time.
More about specific initiatives helping us in our journey to improve the ED experience:
More options for routine care and non-emergency acute care
Our virtual care platform – ECU Health Now – is always available to provide fast, convenient care from any location. Visit ECUHealthNow.org to learn more.
ECU Health estimates that eastern North Carolina has a shortage of 150 primary care providers in order to meet the needs of the region. While we cannot solve this shortage on our own, we’re working hard to expand access to primary care and have expanded appointments by 17%. This equates to seeing nearly 2,700 more patients per month in the primary care setting.
New separate ECU Health urgent care facilities for adults and minors will open within a year. While this will not solve wait times in the ED, it will help connect patients to urgent care resources in a location outside the ED.
Physician in Triage
During the busiest times in the ED, ECU Health Medical Center has a physician working in triage. The speeds up the medical evaluation, which includes asking the patient about their story, performing a limited physical exam and ordering laboratory tests and imaging studies, sometimes before a patient is placed in a room.
Dedicated case managers for behavioral health patients in the ED
When behavioral health patients can’t access the care they need in the community, they often end up in the ED. ECU Health has set up a dedicated behavioral health case management team which is designed to help patients get connected to the resources they need outside the ED.
More technology to render care more efficiently
At ECU Health, we are using technology to share information faster, get labs/radiology results more efficiently and begin treatments as quickly and safely as possible.
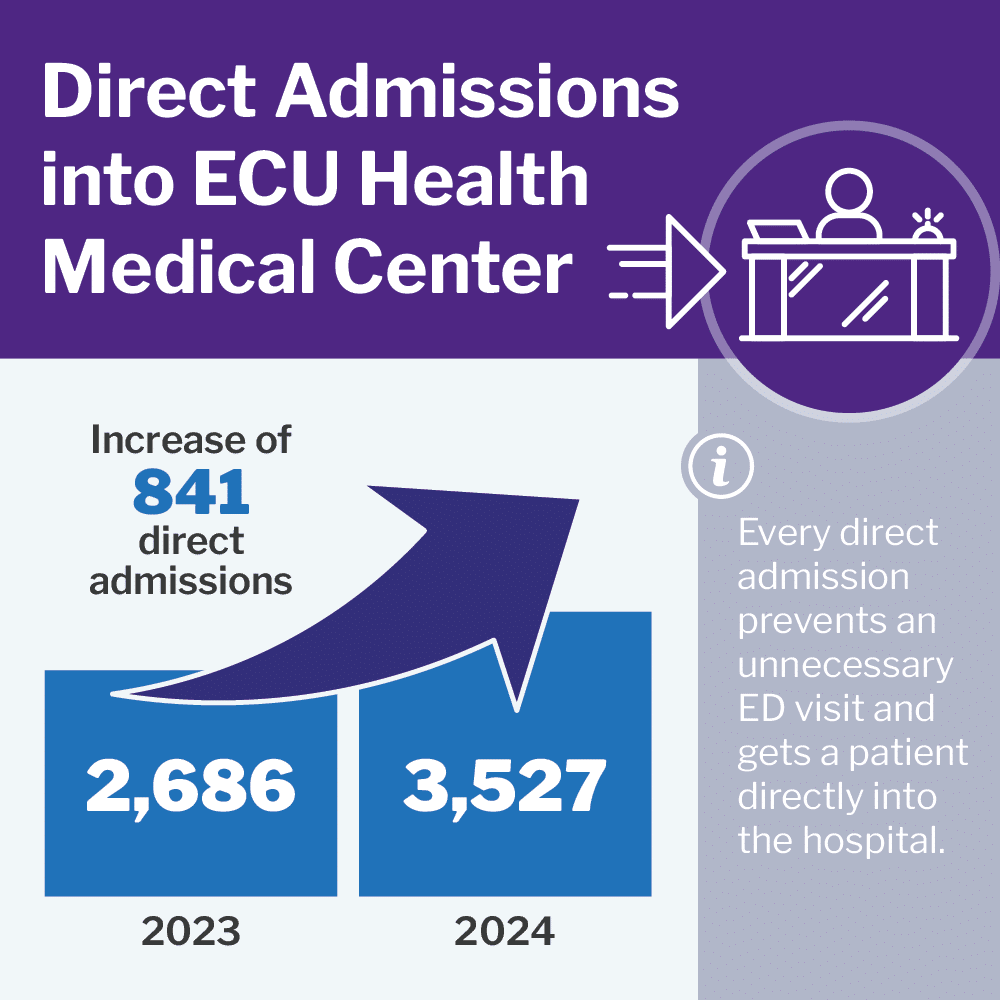
We have also invested heavily in our Operations Center, which manages transfers and placements from across region, especially for ED patients admitted to hospitals. These team members help route patients to the right care facility based on a number of factors.
Connecting patients to transportation
An unfortunate reality facing many of our patients is a lack of transportation. While all patients find a way to the emergency department, not all of them can find a way out, particularly when it comes to needing outpatient services following the emergency department visit. With this need in-mind, ECU Health has partnered with an outside company to begin providing dedicated transportation services from the emergency department for those that need support.
Collaborating with community partners to fill care gaps
There are a number of community-based organizations providing care resources to people with a range of health needs. Collaboration is key, and it is important that we’re all working together to ensure patients receive care in an appropriate setting.
We’re partnering with Pitt County Department of Social Services and other local/regional health care partners to decrease unnecessary ED visits. These partnerships include law enforcement, behavioral health providers, social services, public health departments, medical transportation providers and more.
We’re committed to improving your health and wellness. Eastern North Carolina experiences higher rates of chronic illness and disease. By improving wellness, we can stay healthy and stay out of the ED.
It will take an entire community working together to solve this challenge.

ECU Health engaged with community leaders from eastern North Carolina, all committed to solving the complex challenges of ED utilization.
ECU Health is committed to providing high-quality care, reducing waiting times and optimizing its emergency departments. While we have implemented a number of efforts designed to help meet these goals, there are outside forces contributing to the challenge.
Ultimately, the emergency department is a reflection of the gaps in care and resources that exist across our region. It will take all of us as a community working together to help solve the challenge. ECU Health is committed to constantly improving its processes to ensure high-quality emergency care is provided as quickly as possible. At the same time, we’re committed to working with our fellow health agencies in and around the region to ensure every organization understands the important role it plays in connecting people to care in the most appropriate setting. By working together, we can reduce volume within the ED to ensure those needing emergent care are treated quickly and efficiently.

Read more about a community collaboration event to address challenges in emergency medicine.