Support, action and investment are needed in the East to solve what community members and experts alike are calling a mental health crisis across the region and state. That was the common theme at the Mental Health Town Hall in Greenville hosted by North Carolina Department of Health and Human Services (NCDHHS) Secretary Kody H. Kinsley and local legislators Feb. 9.
The bipartisan panel for the town hall featured Rep. Gloristine Brown, Sen. Jim Burgin, House Majority Leader John Bell, Rep. Dr. Tim Reeder and Sen. Kandie Smith, all of whom represent districts that fall within ECU Health’s 29-county service area. With more than 150 people in attendance, community members and representatives for local organizations shared their perspectives on mental health with the panel.
Kinsley said town halls are crucial to help him and other state officials understand the unique challenges in each area of the state.

“We are having mental health challenges all across the state, but every community is different because every community’s resources are different and their needs are different,” Kinsley said. “It’s really important to me as we set statewide policy that we’re doing it in a way that is informed by boots on the ground, and we heard a lot of that tonight, and we know we have a lot of work to do, and I’ve appreciated this conversation.”
Dr. Michael Lang, chair of the Department of Psychiatry & Behavioral Health at ECU Health and the Brody School of Medicine said the town hall was a positive step to help share with leaders what he and others are seeing locally. He said it was symbolic to bring the event to Greenville where he and his team see a disproportionate number of patients daily needing mental health resources at the ECU Health Medical Center Emergency Department.
“This was a great event for us overall,” Dr. Lang said. “We had a chance to meet our leadership from Raleigh and let them know about the issues and challenges we’re facing, not only here in eastern North Carolina but across the state. I can tell you firsthand we feel the impact of the mental health crisis here in the region and here in Greenville at the medical center. The challenges we’re talking about, such as a lack of access to resources and a dependence on emergency department visits for those suffering from mental health crises, are felt every day at hospitals across the region. That’s why it is important to focus on improving outpatient behavioral health resources to crate stable environments and prevent hospitalization.”
Officials noted there are at least 350 mental health patients in emergency departments across the state waiting for bed placement on any given day. The lack of access to care and resources are more magnified in rural areas such as eastern North Carolina where there is a disproportionate number of under or uninsured individuals. The bipartisan panel all agreed Medicaid expansion in North Carolina would help provide necessary resources towards solving the crisis and Sen. Burgin noted that Medicaid expansion would allow the state to spend more than $1 billion on improving access to behavioral health resources.
 “ECU Health is grateful for our local legislators who are committed to having these difficult but necessary conversations while at the same time pursuing common-sense solutions like Medicaid expansion,” said Brian Floyd, chief operating officer, ECU Health. “Medicaid expansion would help provide needed health coverage to 100,000 people in our region and improve the way we as a state deliver behavioral health resources.”
“ECU Health is grateful for our local legislators who are committed to having these difficult but necessary conversations while at the same time pursuing common-sense solutions like Medicaid expansion,” said Brian Floyd, chief operating officer, ECU Health. “Medicaid expansion would help provide needed health coverage to 100,000 people in our region and improve the way we as a state deliver behavioral health resources.”
At ECU Health, the system announced a partnership with Acadia Healthcare to build a state-of-the-art, 144-bed behavioral health hospital in the medical district of Greenville, less than a mile from ECU Health Medical Center.
The hospital, slated to open in 2025, will provide important access to behavioral health services for adults and pediatric patients, with 24 inpatient beds specifically for children and adolescents with mental health needs.
“I’m incredibly grateful for health systems that have been investing in building more behavioral health beds,” Kinsley said. “This is important but I have a job to do on this, too. We have got to increase [reimbursement] rates to help make those beds sustainable and used.”
Resources
East Carolina University’s postgraduate program in cardiac psychology creates professionals who are ready to help patients cope as they adapt to life-saving heart devices.
On the heels of marking its 15th year, ECU’s nationally unique program in clinical health psychology continues to gain momentum through positive patient outcomes — and national recognition.
The program is a collaboration between ECU’s departments of psychology and cardiovascular sciences that has yielded a nationally unique blend of academics and research. The model integrates training psychology doctoral students and cardiology fellows in cardiac clinics, a strategy that the program’s founder calls the best of both worlds.

“This is a success story from eastern North Carolina,” said Samuel Sears, program director and professor in the departments of psychology and cardiovascular sciences. “From a national landscape, this is an extremely unique program. Only at East Carolina do you have this kind of synergized, integrated, one-for-one engagement in the training of cardiologists and the training of psychologists. Our program is intending to lead the country in this.”
Sears established the training program in 2007 and collaborates with Rajasekhar Nekkanti, associate professor and director of the cardiology fellowship program at ECU and ECU Health, to offer ECU students an integrated program experience that spans clinical care, research and training.
“Dr. Sears and his colleagues have been able to accomplish what others have only talked about,” said Alan Christensen, professor and chair of the ECU Department of Psychology. “Their seamless integration of clinical psychology into a cardiovascular medicine setting is really a pioneering effort in implementing what I believe will prove to be a more effective approach to training, research, and caring for patients.”
The growing field of cardiac psychology focuses on providing psychological care that is an interdisciplinary, comprehensive care approach to cardiac arrhythmia patients and their families.
Depression and anxiety are common occurrences after cardiac events and can occur in as many as one-third of all patients. These conditions interfere with all aspects of recovery from daily rehabilitative planning, medication adherence, and the pursuit of quality of life.
“Cardiac psychologists help by validating the emotional experience of having a heart problem, and helping patients take the next steps in their recovery emotionally and behaviorally,” Sears said. “ECU Cardiology and Cardiovascular Surgery continue to innovate, and that allows our patients to survive. Here at East Carolina, we have the vision and program to address the patient experience and recovery process fully from a psychological and behavioral perspective. We integrate all the aspects of recovery and prepare trainees for the future of cardiac care.”
The program was highlighted in a 2022 edition of Health Psychology, a journal of the American Psychological Association. The article, “Cardiac Psychology Training in a Rural Health Care Setting: East Carolina Heart Institute,” was led by author Kayla Sall, a 2023 graduate of ECU’s clinical health psychology program. Doctoral students Ashley Griffith, Emily Midgette, Andrea Winters and Connor Tripp also co-authored the article with Sears and Nekkanti.
“We are very proud to publish in our field’s top journal,” said Sall, who begins a psychology internship at Brown University this fall. “The publication goes to show how unique our training experience is. It’s very rare to find cardiac psychologists that are located in cardiology.”
The Health Psychology article covers not only the program’s unique nature of intertwining science with practice, but also its ability to adapt to the COVID-19 pandemic by transitioning to using telehealth to serve patients in rural North Carolina. It also explores the health disparities in eastern North Carolina that impact cardiac patient care and progress.
“Cardiovascular health is one of the leading causes of death in the U.S.,” Sall said, “so being able to take that lens and apply it to the social determinants of health has been amazing, and it’s how we’ve been able to do what we do.”
Greenville native and ECU graduate Scarlett Anthony didn’t have to go far to find a program that offers world-class education and preparation that will help her make a difference in her home region and beyond.
“I chose ECU’s program because of the focus on health psychology and the intersection between psychology and medicine. We train alongside psychologists who are embedded in medicine, and our program provides us with exceptional training among various health care settings,” said Anthony, a doctoral student in clinical health psychology. “I chose ECU’s program because of the dedication to serving diverse populations of eastern North Carolina, and I am passionate about providing care to those who may not have access to health psychology services otherwise.”
Standards of practice

Sall led the writing team in detailing the ECU training program and its strong collaborations in cardiology. The article presents ECU’s program as a national model for ideal collaboration between cardiology and psychology training that enhances the clinical and research expertise of both groups.
The ECU cardiac psychology program is part of the APA accredited clinical health psychology program. This program has achieved national rankings over its 15-year existence and annually has an approximately 5% acceptance. Rob Carels serves as the director of clinical training for the clinical health program.
“The article confirmed that the ECU program is not only one of a kind, but it remains the model as programs and universities try to create this similar-type experience,” Sears said. “The reason it’s so hard to create the ECU experience is that it requires both physicians and psychologists accommodating very different mindsets and contributions with the shared goal of patient success first. Physicians can quickly implant a cardiac device. Psychologists can quickly assess and treat psychological concerns. But when these two sets of problems merge, we need shared expertise.”
The article also highlights the setting of ECU’s health psychology program, a rural area where the social determinants of health — including environment, economic stability, community context, education and health access — impact health and wellness on a greater scale.
“Being in eastern North Carolina, we have a very unique setting with our patient population in a rural area,” Sall said.
That context allows psychologists to better understand the behavioral and mental health of cardiac patients. Many patients seen by cardiac psychologists at the East Carolina Heart Institute include those who suffer depression after a heart attack or other cardiac event, those with atrial fibrillation (a-fib) and those who have recently been fitted with implantable cardioverter defibrillators (ICD) — devices similar to pacemakers that correct heart arrhythmias with a high energy shock that can feel like being kicked by a horse.
“I think that is what is so scary for patients; they agree to have this device implanted, they know it’s life-saving, but you don’t know when the shock is going to go off,” Sall said. “You may go the whole rest of your life without receiving a shock, so that’s where part of the anxiety and fearfulness comes in.”
In the program’s scientist-practitioner approach, providers on each side have a thorough understanding of the opposite discipline.
“I think that’s what’s cool about cardiac psychology — here we are with people presenting with medical conditions or health issues and we’re evaluating, diagnosing, treating emotional behavioral disorders within the context of health and medicine,” Sall said. “We’re not doing just one or the other, we’re doing these together.”
World expert in action
Sears is a highly productive researcher examining quality of life and psychological adjustment in patients with heart rhythm disorders and ICDs. He has published more than 200 articles in the medicine and psychology research literatures and has well over 11,000 citations. In 2021, Expertscape.com named Sears one of the top 50 experts and most prolific authors in the world on ICDs over the last 10 years, amongst the 27,847 authors on the topic.
“I’m involved in both the training of psychologists as well as the training of cardiologists, so we’re trying to make cardiologists better at patient psychology and psychologists better at understanding the cardiology, so it’s synergistic,” Sears said.
Sears travels the world presenting his research and lending his expertise to patient, family and physician groups.
In 2013, the UNC Board of Governors presented Sears with the O. Max Gardner Award, the highest honor bestowed to a faculty member in the UNC system for contributions to mankind.
“The O. Max Gardner Award changed me because I stopped looking for external validation about our achievements. I desperately wanted to make an impact on our patients, our students, our university, our state and beyond,” he said. “The award confirmed some of these marks, so I used my energies more efficiently on the work at hand. I am proud of the health psychology program and the cardiac psychology program that my colleagues and students have created. In terms of work, I am so pleased that many of our ideas about helping cardiac patients are broadly employed across many sectors in cardiology, not just where we started.”
The article in Health Psychology signals consistent success and upward momentum for the program, said Sears, adding that Yale University’s health psychology program is the only other such program mentioned in that edition of the journal.
“This is a 15-year-old program. We’ve established success,” he said. “This is not a great idea that’s going away. Great ideas happen all the time, but they’re not sustainable. This is a sustainable solution that has true outcomes.”
When it comes to patient outcomes, Sears is optimistic that the growing field of cardiac psychology will continue to yield hope and healing.
“We can’t fix all the health inequalities, but what we can do is help our patients make small steps to have better awareness of where there are a lot of possibilities and decision points, and connect them to other resources,” Sears said. “Yes, this is a hard mountain to climb. Let’s do this together.”
Doctoral student Zachary Force said students begin the program learning what clinical health psychology can offer the world — and how ECU is leading the way.
“ECU has always done things differently, and other institutions are starting to take notice. ECU’s cardiac psychology service has received national recognition as the only place in the country to receive specialized training in an area with increasing need,” he said. “ECU’s fighting spirit imbues its doctoral students with the resiliency needed to advocate for psychology within the medical field.”
Read more from ECU News Services

Dr. Sy Atezaz Saeed
Contrary to popular belief, psychiatric disorders such as depression and post-traumatic stress disorder are just as common as other chronic conditions. About 11 percent of the U.S. population has been diagnosed with Diabetes, while in comparison 26 percent of the population has a diagnosable mental disorder per year.
Unlike other chronic conditions, there are few resources to treat mental illnesses in North Carolina, which is exemplified by the lack of behavioral health providers. Alarmingly, 42 out of 100 counties in the state have no psychiatrist or active behavioral health provider, leaving more than half of adults with mental illness without treatment options.
How did we get here?
In 2001, the state of North Carolina began to privatize mental health services by transitioning them from public area authorities to private provider groups. This transition meant private agencies would become solely responsible for caring for people with behavioral and mental health disorders as well as substance use disorders. For those without access to a local behavioral health professional or without the ability to pay for care, their only option is often the hospital emergency department (ED). In fact, one out of every eight ED visits is related to mental illness or substance use disorders. This puts more strain on EDs, which were not designed for this type of specialized care.
Working together
As a community, we need to work together to change the way behavioral health care is delivered in North Carolina. Solving the mental health crisis requires collaboration and partnership across a broad spectrum of services. One way ECU Health is doing this is through a joint venture partnership with Acadia Healthcare, a national leader in providing behavioral health services. Recently, we announced plans to build a state-of-the-art behavioral health hospital that is slated to open in spring 2025, pending regulatory approval.
In addition to serving adult patients, the new hospital will provide much-needed access to the behavioral health needs of children and adolescents, providing the only child and adolescent psychiatric beds within 75 miles of Greenville. Together, both ECU Health and Acadia will invest more than $60 million in expanding behavioral health resources.
Working in tandem with other partner organizations as a network providing a wide variety of treatment options can create a much greater impact than we’re able to on our own.
Everyone deserves access to high-quality health care, and ECU Health is committed to doing its part to offer vital behavioral health treatment to eastern North Carolina. While this partnership provides promise for those who are seeking behavioral health care, my hope is that we continue to find ways to partner in our communities and across the state to ensure our residents have access to the care they need to live healthy, fulfilling lives.
Sy Atezaz Saeed, MD, MS, FACPsych is Executive Director of the Behavioral Health Service Line for ECU Health, and Professor and Chair Emeritus of the Department of Psychiatry and Behavioral Medicine in the Brody School of Medicine at East Carolina University. He also serves as the Founding Director of the Center for Telepsychiatry at ECU and as the Founding Director of North Carolina Statewide Telepsychiatry Program (NC-STeP). Dr. Saeed has published more than 100 peer reviewed publications. In 2019, he was awarded the prestigious Gov. Oliver Max Gardner Award, the highest UNC award and selected by the UNC Board of Governors, which recognizes UNC system faculty who have “made the greatest contribution to the welfare of the human race.” To learn more, visit ENCBehavioralHealth.org.
Health care workers are well-versed in serving their community, even if that community happens to be an ocean away.
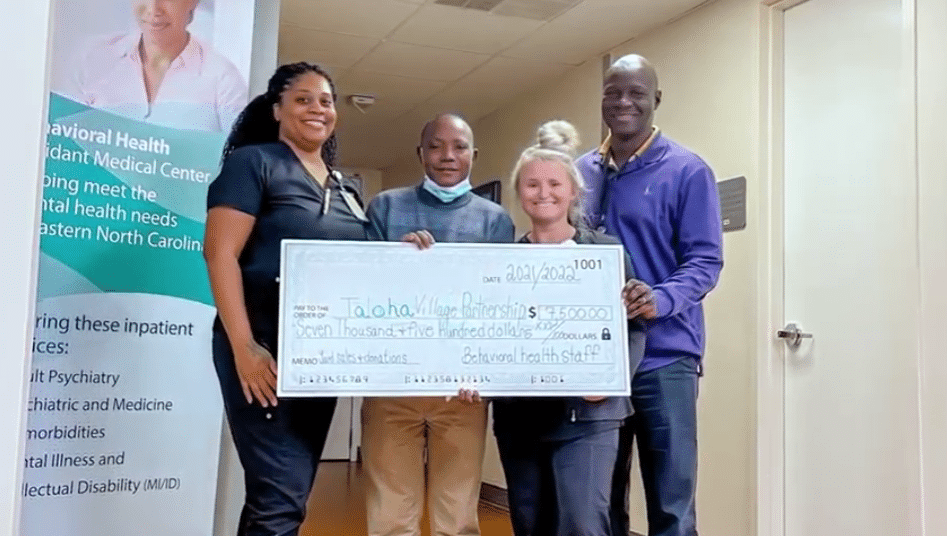
“I’m from Tanzania, east Africa. In a rural village called Taloha,” said Daniel Makoko, behavioral health team member at ECU Health.
After settling in eastern North Carolina, Makoko continued to help improve living conditions in his home village.
“The village has one primary school,” Makoko said. “So these kids use like four classrooms but there are like 270 kids. They share the classroom because it’s not enough. But also the main problem was that the room was leaking when it’s raining.”
So Makoko set about raising money through donations and events like yard sales to put a new roof on the primary school.
“They asked me, ‘What can we do?’ So I told them that if we can get a roof for them, It will be much transformation for the school,” said Makoko.
A transformation in more ways than one, made possible with the help of friends, family and colleagues.
“He’s a great inspiration to me just to see all the things that he has accomplished”, said Tony Dixon, a behavioral health team member at ECU Health. “Between four yard sales and donations from behavioral health services, we were able to raise the four-thousand dollars to get the roof done.”
“I was able to go there and implement the project and we finished the roof and the kids were so happy,” said Makoko.
It’s joy no roof can contain and an example of ECU Health values making a difference half a world away.
“This shows the greatness of the people here and how they are able to respond to the needs of other people across the world,” said Makoko. “I really appreciate it so much.”
Resources
Watch more ECU Health News videos
GREENVILLE, N.C. – ECU Health and Acadia Healthcare announced today plans to build a state-of-the-art, 144-bed behavioral health hospital in the medical district of Greenville, N.C., less than a mile from ECU Health Medical Center. This new facility will be a center of excellence, providing North Carolinians with important access to behavioral health services and treatment from specialized clinical teams in a carefully designed environment.
Slated to open in spring 2025, the hospital will be operated through a joint venture between ECU Health and Acadia, the largest standalone provider of behavioral healthcare services across the United States. Together, the organizations will invest approximately $65 million in expanding behavioral health resources in eastern North Carolina.
![Perspective View 2 - NIGHT [no-logo] Conceptual rendering of new behavioral health hospital](https://www.ecuhealth.org/wp-content/uploads/2022/07/Perspective-View-2-NIGHT-no-logo.jpg)
The hospital will include 24 inpatient beds specifically for children and adolescents with mental health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
“This hospital will be a tremendous resource for our patients and our state, and we’re thrilled to bring a partner and a national leader like Acadia to eastern North Carolina,” said Dr. Michael Waldrum, chief executive officer of ECU Health and dean of the Brody School of Medicine at East Carolina University. “Acadia has an established track record of providing high-quality, compassionate care in communities across the country. Together, we will strengthen our level of expertise, implement proven best practices and enhance the quality and number of behavioral health services available to patients throughout the region.”
Prior to the pandemic, nearly one in five North Carolinians were experiencing a mental, behavioral or emotional disorder, according to a report from the North Carolina Institute of Medicine’s Task Force on Mental Health and Substance Use. In the last two years, national data indicates a growing trend of depression and anxiety symptoms. This partnership demonstrates a commitment to talking about mental health disorders, normalizing and treating them with the latest science and medicine in appropriate care settings.
“As a clinician, seeing this type of investment and understanding the significant impact it will have on patients is exciting,” said Dr. Syed A. Saeed, an ECU Health board-certified psychiatrist with more than 40 years of experience. “The needs of behavioral health patients differ from other patients and vary widely even within the same diagnosis. This state-of-the-art hospital will allow us to fully meet our patients’ unique needs in a safe, patient-centered environment and ensure clinicians have the resources and training needed to deliver excellent care.”
The new hospital will also serve as a teaching hospital, training students and residents from the Brody School of Medicine, many of whom will go on to practice in eastern North Carolina and carry forth ECU Health’s mission to improve the health and well-being of the region.
“We are always seeking like-minded partners who share our commitment to expanding access to high-quality behavioral health services and transforming the way mental health patients are seen and cared for,” said Chris Hunter, chief executive officer of Acadia Healthcare. “Establishing a center of excellence in partnership with ECU Health presents a unique opportunity for us to support the development of the next generation of behavioral health care workers and clinicians. We’re excited to begin this important work with such a committed, patient-focused partner.”
Construction is expected to begin in 2023, pending standard state and regulatory approvals and gaining a Certificate of Need. To facilitate the development of the new 144-bed behavioral health hospital, ECU Health will transfer 80 of its current behavioral health beds.
To learn more about the potential partnership between ECU Health and Acadia Healthcare, visit
ENCBehavioralHealth.org.
Find more information in our Press Kit.
The promise of fresh starts, prioritizing and setting goals have become synonymous with the New Year. As you reflect on the physical, professional and financial goals you hope to accomplish in 2022, do not forget to take your emotional well-being into consideration.
“It is important to take time and make mental health a priority in your life, just as you would seek proactive lifestyle activities such as physical exercise and healthy eating,” said Dr. Ashley Britton, clinical assistant professor and psychologist at ECU’s Brody School of Medicine and ECU Health Medical Center. “To keep mentally fit, you should focus on enjoyable and meaningful activities as well as practice activities to keep your brain stimulated.”
With the start of 2022, the ongoing pandemic continues to disrupt lives and profoundly impact mental health. People continue to struggle with depression and anxiety as we experience expanded time in isolation. There are some key tips for helping us cope with the toll the pandemic is taking on us both mentally and physically. Maintaining structure and routines will greatly help with fortifying your mental well-being.

Chronic stress demands elevated levels of energy and cognitive hypervigilance but is not sustainable over time. In fact, chronic stress is extremely harmful to our health in the long term. Our bodies address stress through a process called General Adaptation Syndrome (GAS) that aims to manage stress and return us to normal, healthy levels of functioning, according to Dr. Britton. General adaptation syndrome affects the body in three stages.
The first stage is the alarm reaction stage also known as “fight or flight,” where your body sends a distress signal to the brain, causing it to release hormones including adrenaline. The second stage is the resistance stage, when your body is trying to recover from the alarm reaction. If there is persistent stress, you could experience lack of concentration and short term memory issues. The third stage is known as the exhaustion stage or the “burned out” feeling, which is what the extended pandemic has caused many of us to experience.
“In 2021, there was the sense that people were just trying to push through the pandemic,” said Dr. Britton. “However, for 2022, it is the time to practice resiliency and move forward by renewing or creating new connections to friends and resources.”
Connecting to others is a key factor in building resiliency, whether it be through phone conversations, virtual conversations or safe socially distanced or masked physical interactions such as talking in person. Communicating with others not only helps you feel better connected, it also helps you focus on what others around you are going through and takes you out of your own problems, keeping you engaged by helping others.
Focusing on what is positive in your life and what is going well is another important factor in becoming more resilient.
“Having work teams participate in a ‘weekly wins’ session, where you either recognize a positive experience from the week or something in the week ahead is an excellent activity to promote focus on positivity,” Dr. Britton said.
Another tip for better mental health is having a particular physical item in your possession that can help ground you in times of stress.
“A photo, ring, bracelet or other personal item can help you focus on your positive connections to them and help keep you present in the moment,” Dr. Britton said. “Keeping your mind stimulated helps direct your thoughts and activities away from negativity and on something that can add to your life, a new hobby or skill. Painting or journaling are some examples of activities to engage the brain in creative pursuits that help with purpose and positivity.”
As you set goals and plans for 2022, remember to give yourself a break when encountering life’s inevitable bumps. Self-compassion is about being inwardly understanding, encouraging and kind in the face of setbacks – a reaction we commonly extend to friends and family members but can forget when it comes to ourselves.
If you or someone you love are experiencing depression or anxiety, reach out for help. The National Suicide Prevention Lifeline can be reached at any time at 800-273-TALK (8255). Integrated Family Services provides Mobile Crises services in many eastern North Carolina counties. Call 866-437-1821 or visit integratedfamilyservices.net.
These topics included psychiatric disorders, stress management, resiliency and substance use. This series came at a crucial time, as COVID-19 kept many people indoors and away from their typical routines. That isolation and facing many unknowns in our world brought out mental health challenges.
Data trends show a steady increase in adults suffering from anxiety, stress, and depression over the past year.
Glenn Simpson, system service line administrator for Behavioral Health at Vidant, joined WITN to discuss the series.
“Some studies are indicating that four out of 10 of us in the last year have experienced depression or anxiety in a clinical range,” Simpson said. “If you went back two years, that would have been one out of 10, so we are very concerned about people’s mental health. Often times we will take care of our physical health before our mental health. We’re hoping by this series to help folks reach out for the help they need.”
Simpson said the series was exciting and brought forward experts in the field to talk to the general public about mental health and well-being.
Video recordings from the series can be found in the Behavioral Health section of VidantHealth.com.
Anxiety in adults exasperated over the pandemic
A new study from GlobalWebIndex has shown that many adults are worried about the lasting effects the pandemic will have on mental health.
According to the study, 28% of Millennials, and 29% of Gen X adults believe the pandemic will have long-term impacts on their mental health. Additionally, the study found that anxiety, stress and insomnia had all risen across all age groups in the study.
Dr. Nathan Harper, medical director for inpatient psychiatry at ECU Health Medical Center and ECU, said he there has been an increase in patients for mental health needs and services, not only in adults but for children as well. Dr. Harper said he believes isolation from quarantine made some of these issues more prevalent.
Dr. Harper discussed the study and his experience during a recent interview with WNCT.
Vidant has resources and information available on the Programs & Support page.