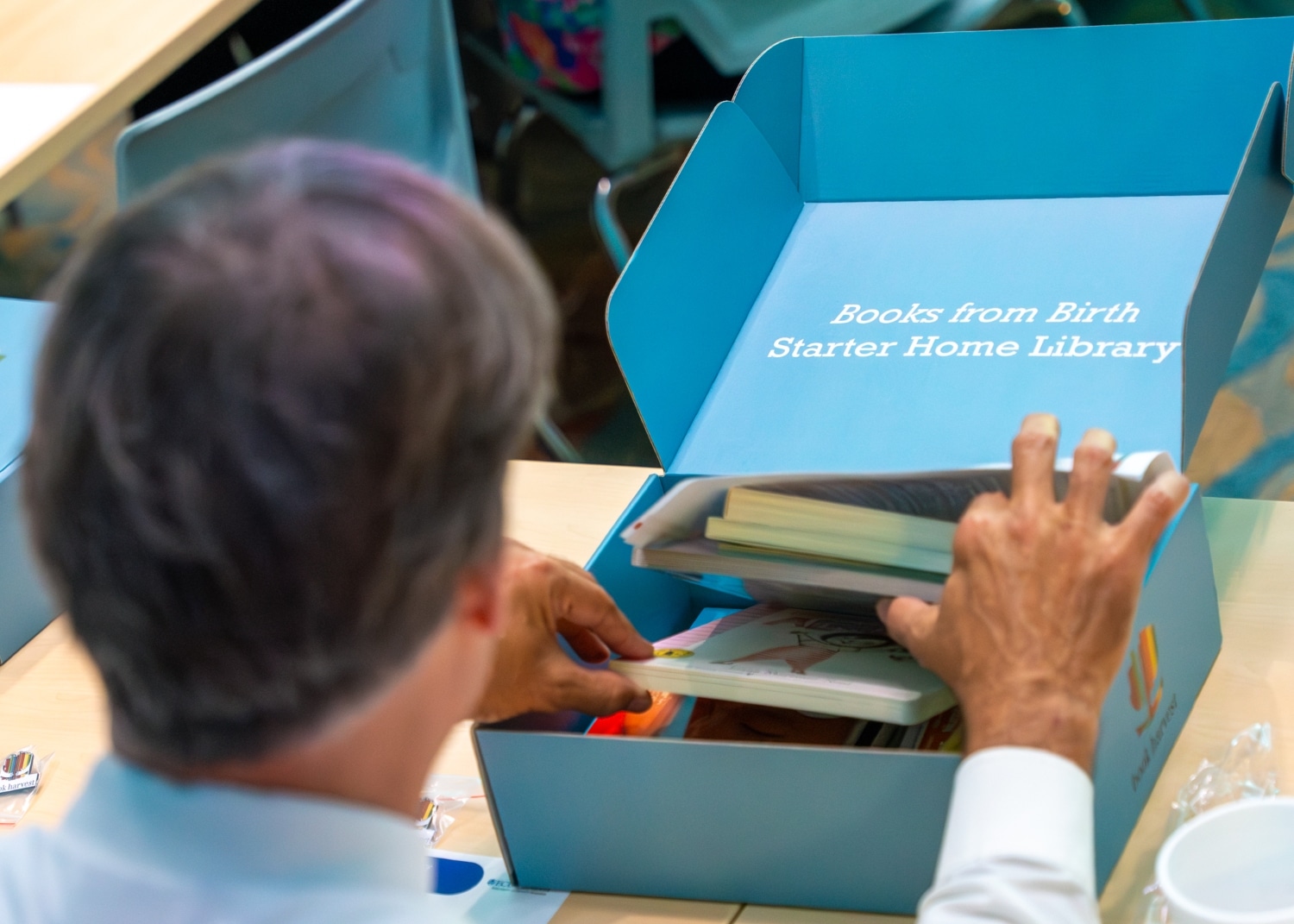
Books from Birth, a Book Harvest program, will begin providing children’s books to families of babies born in Maynard Children’s Hospital at ECU Health Medical Center starting in summer 2024. The books will help families foster early language and reading routines from a baby’s first days.
In preparation for the upcoming go-live, ECU Health hosted an event to educate team members at Maynard Children’s Hospital on Friday, June 14. Team members learned about Books from Birth, how these books can help families bond and improve early childhood education.
Book Harvest is an organization based in Durham that provides ongoing literacy support and an abundance of children’s books to families.
By partnering with Maynard Children’s Hospital, this collaboration will provide families and children in the East with the support and books they need to foster early language and reading routines at home from a baby’s very first days.
“The Books from Birth program is really designed to bridge early education and health,” said Book Harvest Chief Operating Officer Jeff Quinn. “Early literacy lays a foundation for life-long learning and healthy development. This program is meant to give children the opportunity to be what they want to be in life. We could not be more proud to help serve Pitt County and eastern North Carolina through this collaboration.”
N.C. House Rep. Tim Reeder, MD, District 9, secured funding of $500,000 for the project in the North Carolina State Budget. Rep. Reeder thanked Book Harvest and ECU Health for their willingness to partner on this important initiative. With his medical background in-mind, Rep. Reeder detailed the importance that early literacy has on the development of children as they grow, as well as the importance of improving access to education in eastern North Carolina.
“As a practicing physician, I see first-hand the benefits of early childhood literacy in terms of creating success in the classroom and in children’s behavior,” Rep. Reeder said. “Per data released from the state, about 50% of the children in Pitt County are not reading at grade-level. Early intervention and early reading is critically important to setting our children up for success. These books will help set families on a path to literacy that we know is really important to long-term development. I was proud to advocate for this funding and I am excited to see the impact this partnership will have.”
The Books from Birth program will provide a box of 10 board books, helpful reading education materials and a onesie for families who deliver babies in the Maynard Children’s Hospital.
“The benefit of giving these books at birth is that they help form loving and bonding relationships between babies and their caregivers,” said Dr. Matthew Ledoux, pediatrician in chief, ECU Health, chair of pediatrics, Brody School of Medicine at East Carolina University. “As a rural academic medical center serving a third of the state, it is incredibly valuable to get these books in the hands of families throughout eastern North Carolina. For that, we are very grateful.”
According to Tara Stroud, vice president, Women’s and Children’s Services, Maynard Children’s Hospital, the program will provide around 4,300 boxes of books to patients and families.
“This is our chance as a health system to change what it looks like for literacy in eastern North Carolina starting from the beginning,” said Stroud. “Our goal is that we demonstrate for our families the importance of books as a way to connect and bond with their child and improve their development.”

For Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center and Safe Kids Pitt County, the message she wants to get out is simple: “Never leave a child, senior or pet alone in a car, even for a minute.”
Walston’s message was amplified at a Hot Car Safety event in June hosted by ECU Health in partnership with the Pitt County Sheriff’s Office, Pitt County Health Department and the Martin-Pitt Partnership for Children, to demonstrate how quickly cars heat up.
The event included a demonstration with temperature gauges and s’mores roasting in a vehicle on hot, summer day. During an overcast, 88-degree day, the interior of the van rose to 113 degrees within 15 minutes.
The s’mores demonstration showed how quickly things can, quite literally, cook inside of a car when left alone. Volunteers handed out the s’mores to shoppers to explain the demonstration in a fun, interactive away.

“We host these types of events to raise awareness so parents are realizing how hot cars can become,” said Walston. “A car can heat 20 degrees in as quickly in 10 minutes. In our display today, it is already 113 degrees, and it’s only 86 degrees outside.”
According to Walston, about 17 percent of hot car fatalities occur in children intentionally left in the car. During this time, parents or caregivers are often running into the store or running an errand for a few minutes, thinking that will be fine.
“A lot of times, people think ‘I’m just going into the store for a few minutes,’ but anything could happen inside, from losing track of time to becoming distracted and forget the child,” Walston said. “There is a misnomer that if you crack a window and that will offer some less heat, but that really is a myth. It doesn’t affect the temperature of the car or cool the temperature down.”
Walston said it’s dangerous for anyone to be left alone in a vehicle because of how quickly they can heat up, but especially for children.
“Children’s bodies heat three to five times more quickly than adults,” Walston said. “They all have a smaller amount of body surface so they can’t cool themselves very quickly. A small child, like the families we’re serving today, they can’t verbalize when they’re thirsty if they’re under a certain age.”
More than 50 percent of child deaths from hot cars are children forgotten in vehicles, according to Walston. She said children can be forgotten when routines are broken, and leaving something like keys, a cellphone or a briefcase in the backseat next to the child or setting an alarm on your phone are extra safety measures one can take to ensure the child is not left in the car.
Walston encouraged attendees to call 911 if they ever see a child, senior or pet alone in a call.
“This is something parents really need to take seriously,” said North Carolina Insurance Commissioner Mike Causey. “It’s year-round, not necessarily just during the hottest months of the summer. We have had children die in November and other months outside of June, July and August.”

Greenville, N.C. – ECU Health is partnering with Food Lion Feeds, Sodexo and the ECU Health Foundation to provide free meals for kids, teens and people with disabilities as part of the Summer Meal Program. Meals will be available in Greenville, Bethel and Ahoskie. The selected sites this year were chosen based on the need in each county, existing partnerships and the social vulnerability index at each location.
During the school year, many kids and teens receive free or reduced-price meals. When schools close for the summer, those meals disappear, leaving families to choose between putting the next meal on the table or paying for other necessities like utilities or medical care. While over 57% of students in North Carolina receive free or reduced lunch, 66% of Pitt County students and over 90% of Hertford County students receive free or reduced lunch.
Meals will be available until food runs out each day at the following locations:

- Greenville: English Chapel Free Will Baptist Church – 11:30 a.m. to 1 p.m., Monday-Friday from June 10 to Aug. 23. The location will be closed July 22-26.
- Ahoskie: Calvary Missionary Baptist Church – 11:30 a.m. to 1 p.m., Monday-Friday from June 10 to Aug. 23. The location will be closed June 19 and July 4-5.
- Bethel: Bethel Youth Activity Center – 11:30 a.m. to 1 p.m., Monday-Thursday from June 17-July 17. The location will be closed July 3-7.
ECU Health has offered the Summer Meal Program since 2021, providing nearly 12,000 free meals to kids and teens during the summer months. In 2023, 51 ECU Health team members served more than 2,800 meals to kids in need.
No registration is required. For more information about the ECU Health Summer Meal Program, please email [email protected].
GREENVILLE, N.C. – The Children’s Miracle Network (CMN) 39th Annual Celebration Broadcast, which celebrates the thousands of children in eastern North Carolina who have received treatment at James and Connie Maynard Children’s Hospital at ECU Health Medical Center this past year, raised $1,258,511 Children’s Miracle Network Hospitals’ longtime television partner, WITN, which produces the fundraiser, shared the stories of complex illnesses, traumatic injuries and the quality medical care Miracle Children received from Maynard Children’s Hospital.
“Caring individuals, community groups, businesses and others show how much they care about children by providing generous contributions to Children’s Miracle Network Hospitals,” said Elise Ironmonger, director of programs, ECU Health Foundation. “In eastern North Carolina, this generosity enables the Maynard Children’s Hospital to see beyond obvious treatment and save more lives. The care and high-quality treatment received here will continue into the future through this year’s amazing donors.”
This year, an anonymous donor offered to match every donation up to $100,000. The family has a passion for children in eastern North Carolina and wants to ensure every child has the best chance possible to get better. They are grateful for all of the hard work, dedication and compassion that the team provides at Maynard Children’s Hospital and hopes their contribution provided an extra incentive for people to open their hearts and donate.
The theme of this year’s Children’s Miracle Network Hospitals campaign was “Change Kids’ Health, Change the Future,” which shows how important donations are in helping shape a healthier tomorrow for patients served at Maynard Children’s Hospital. Major contributors to the yearly event, held June 1-2 to raise money for Children’s Miracle Network Hospitals, featured contributions from long-time supporters from across eastern North Carolina including Speedway, part of 7-Eleven, Inc., Jersey Mike’s Subs, Log a Load for Kids and Walmart/Sam’s Clubs.
The Celebration Broadcast featured guests and sponsors who have contributed during the past year, as well as callers who pledged their support.
Earlier this year, the Music for Miracles Radiothon on Inner Banks Media Stations raised $109,703 during the 27th year of their special event, bringing their total raised to more than $3.9 million. The Inner Banks Media radio stations include: 107.9 WNCT; Talk 96.3 and 103.7; Oldies 94.1 and 102.7; and 94.3 The Game.
The largest donor to this year’s campaign came from a long-time corporate partner of CMN Hospitals, Speedway, part of 7-Eleven, Inc., which raised $260,310 in their ninth year of partnership with Maynard Children’s Hospital. The largest fundraising event for our local Children’s Miracle Network program was held by Jersey Mike’s Subs during their annual Month and Day of Giving. Collectively, the 17 participating stores in eastern North Carolina raised $148,196.
Long time CMN supporter, Log a Load for Kids, held their 27th annual sporting clays shoot on May 3-4 and raised $80,000. These funds came from sponsorships, including title sponsors, Colony Tire and Pinnacle Trailer Sales, and had over 600 participants.
Other major donors and their gifts included Walmart/Sam’s Clubs with $155,392; Panda Express with $41,567; Ace Hardware with $33,350; Extra Life with $29,334; Dance Arts Theater with $19,965 and Publix with $15,666.
Other campaign contributors were Dairy Queen with $14,273; Barbour Hendrick Honda Greenville and The Electric Cooperatives of Eastern NC both with $10,000; REMAX with $6,375; Ollie’s with $6,283; American Builders; Pepsi/Minges Bottling Group; Eastern Radiologists, Inc.; and Central Heating and Air Conditioning each contributed $5,000.
Additional gifts were from: Phi Mu Chapter of ECU with $4,791; Baynor with $4,000; Miller and Friends Lemonade Stand with $3,157; Grady White Boats with $3,000; Care-O-World Enrichment Learning Center with $2,231; Oasis Shrine Temple and brothers, Arun and Ajay Ajmera each with $1,500; Action Advertising, Equipment Plus, Ricci Law Firm; Builder’s Discount Center, Harris, Creech, Ward and Blackerby, PA, Stallings Plumbing, Heating and AC and Coldwell Banker’s Sea Coast each gave $1,000.
The local CMN Hospitals fundraising program is staffed and supported by the ECU Health Foundation, the non-profit charitable corporation that serves as the custodian for all financial gifts and bequests to ECU Health. The ECU Health Foundation oversees allocation of all donated funds.
GREENVILLE, N.C. – The Children’s Miracle Network (CMN) Celebration Broadcast honors past telethon traditions by celebrating selected miracle stories of children who represent the thousands of children in eastern North Carolina who have received treatment at James and Connie Maynard Children’s Hospital at ECU Health Medical Center this past year. This year, the CMN Celebration Broadcast will be held on Saturday, June 1, from 7-8 p.m. and Sunday, June 2, from 6-9 a.m. and 7-11 p.m. airing on longtime partner, WITN. Examples of how CMN donations are used will be featured throughout the event as well to show the impact philanthropic gifts truly make.
“We are so grateful to all those who support our Children’s Miracle Network Hospitals program all throughout the year,” said Elise Ironmonger, director of programs, ECU Health Foundation. “The generosity of our donors enables Maynard Children’s Hospital, located in Greenville and serving 29 counties, to provide life-saving care to the thousands of children who are treated each year. We look forward to being able to showcase the amazing care provided every day at Maynard Children’s Hospital during this weekend’s telethon and to have an opportunity to thank our amazing donors.”

This year’s Miracle Children and Teen include:
- Jadon Green, 1 year old, Greene County
- Leonardo Velasquez-Bartolon, 2 years old, Wayne County
- Layah Collins, 6 years old, Jones County
- Wiley Sloan, 14 years old, Wake County
The 2024 broadcast will highlight examples of the amazing care offered every day at Maynard Children’s Hospital while celebrating the miracles made possible by the life-saving care generous donations help provide. Thanks to the generosity of eastern North Carolina, thousands of children receive the specialized medical care they need, bringing them and their families the gift of hope and healing. Because of this support, the team at Maynard Children’s Hospital can ensure patients receive the best care possible.
The local Children’s Miracle Network Hospitals fundraising program is staffed and supported by the ECU Health Foundation, the non-profit charitable corporation that serves as the custodian for all financial gifts and bequests to ECU Health. The ECU Health Foundation oversees allocation of all donated funds. To donate, please call 1-800-673-5437 or visit givetocmn.com.
When Dr. Shannon Longshore, the medical director of the pediatric trauma program at ECU Health Medical Center, first joined the hospital, the James and Connie Maynard Children’s Hospital at ECU Health Medical Center wasn’t a verified pediatric trauma center. Now, Maynard Children’s Hospital is one of only four Level I Pediatric Trauma Centers in North Carolina and the only one serving the East.
“It is incredibly fulfilling to reflect on the growth we have experienced over the years, to now achieving verification as Level I Pediatric Trauma Center,” Dr. Longshore said. “Our teams across ECU Health have dedicated their work to constantly improving our care over the course of many years. From prevention, to treatment, and being entrusted to provide critical care at the highest level, this verification is a testament to the mission-driven work that defines our hospital and health system.”

The American College of Surgeons’ (ACS) Verification, Review and Consultation (VRC) Program is designed to assist hospitals in the evaluation and improvement of trauma care and provide objective, external review of institutional capability and performance, accomplished by an on-site review of the hospital by a peer review team experienced in the field of trauma care. There are three levels of ACS trauma center verification, with Level I being the highest verification a trauma center can achieve.
Level I Trauma Centers must be capable of providing system leadership and comprehensive trauma care for all injuries and have adequate depth of resources and personnel. These centers play an important role in local trauma system development, regional disaster planning, increasing capacity and advancing trauma care through research.
Recognizing excellence in pediatric trauma care and community outreach
Dr. Longshore herself has been instrumental in Maynard Children’s Hospital’s continued growth as a trauma center through her research and presentations at national conferences and her work with the Eastern Carolina Injury Prevention Program (ECIPP).
The ACS surveyors noted the value of ECIPP, which aims to create a safer environment, change behavior and change policy to improve the quality of life in eastern North Carolina. Sue Anne Pilgreen currently serves as the executive director of the Safe Communities Coalition and the manager of ECIPP, which has been around since 1995. Between 2020 and 2023, ECIPP was awarded more than $1 million in grant funding, which has supported work in areas such as teen driver safety, suicide prevention, firearm safety, and child passenger and bike safety.
“The surveyors were especially impressed with our work around firearm safety and suicide prevention,” said Pilgreen. “We utilize the pediatric trauma registry data, and that is what drives our work.”
Pilgreen was quick to commend ECIPP team’s work in all areas to prevent injuries, and she highlighted that while most trauma programs have one injury prevention person, ECU Health has an entire team. That enables the program to reach out to rural communities and establish new injury prevention processes.
“Even with our incredible injury prevention team, we recognize that injuries will happen,” said Pilgreen. “To have this Level I Trauma Center with the best of the best gives the opportunities for the best outcomes.”
Other specific strengths noted during the pediatric program’s survey included the addition of two pediatric orthopedic surgeons and a pediatric neurosurgeon; outreach clinical simulations in the region; the collaboration among the pediatric orthopedic surgeon, the neurosurgeon and the Pediatric ICU (PICU); and the recent renovation of the PICU to establish a family-friendly place to care for patients. Of note, a large strength also lauded was the academic research and a collaboration with the Brody School of Medicine at East Carolina University’s Department of Pediatrics.
This expansion of the pediatric trauma research footprint was accomplished through more than 10 publications in nationally recognized journals. Both Erika Greene, manager of the pediatric trauma program, and Elizabeth Seawell, manager of the adult trauma program, credited the collaboration with Brody to produce research and get articles accepted to journals.
“That was a big win for us,” Greene said. “We have an academic medical center with the resources and processes in place to care for injured patients, and we’ve done an amazing job to achieve Level I for pediatrics. We have the capabilities to take the best care of those patients to the highest level of the accrediting body.”
Sustained excellence in adult trauma care
The pediatric trauma center’s new Level I verification accompanies the ECU Health Medical Center’s adult trauma center re-verification of Level I, a title they have proudly held for 40 years.
“We were one of the first Level I Trauma Centers in North Carolina, and we were verified by the American College of Surgeons in 2005,” said Seawell. “We are recognized nationally for how we care for patients in a rural area.”
This recent re-verification was made possible in part due to the resources available to the program including neurosurgical, interventional radiology, orthopedic trauma neurology, and vascular resources, operating room capabilities and blood access, as well as a trauma team of 11 surgeons.

“We are the only Level I Trauma Center for 29 counties, and to reach that far and care for that many patients – we served more than 4,000 patients last year – we have to rely on local community hospitals and emergency response teams to ensure timely transfers and communication,” said Seawell.
Seawell noted that ECU Health Medical Center and Maynard Children’s Hospital have a 60 percent transfer in rate, when the national average is 30 percent, which means they work closely with local EMS agencies, regional transfer facilities, other ECU Health organizations and non-affiliated organizations to serve patients from all over the region.
“The role of our trauma program is to not transfer patients but to have all the resources we need. It provides excellence in patient care and helps keep our patients local,” said Seawell.
Dr. Eric Toschlog, medical director of the adult trauma program, emphasized the tremendous preparation required to achieve Level I. He noted that there are more than 100 standards to prepare for, including paperwork, infrastructure, teamwork and more.
“The visit from ACS is a two-day adventure in stress and anxiety,” Dr. Toschlog said. But at the conclusion, he felt immense pride. “This visit was my seventh in 24 years at ECU Health, and it was clearly our best; we were found to have no deficiencies, and the reviewers used words such as ‘exemplary’ and ‘blown away’ regarding multiple aspects of the trauma center.”
Having two Level I Trauma Centers at ECU Health is no small thing, and both centers achieving the highest level of care is due to the dedication of the trauma center teams.
“I am surrounded by brilliant, compassionate, hardworking, mission-driven individuals who share a singular vision of saving the lives of the patients we have the honor to care for each year. Our success is owed to those truly extraordinary people,” Dr. Toschlog said.
Greenville, N.C. – James and Connie Maynard Children’s Hospital at ECU Health Medical Center received verification from the American College of Surgeons (ACS) Committee on Trauma as a Level I Pediatric Trauma Center, becoming one of only four in the state. Maynard Children’s Hospital now joins ECU Health Medical Center as the only Level I Trauma Centers in eastern North Carolina.
“We are proud of the dedication that all of our team members at Maynard Children’s Hospital have made to prioritizing the delivery of high-quality care close to home, and achieving Level I Trauma Center verification is a demonstration of that commitment,” said Tara Stroud, vice president, Women’s and Children’s Services, Maynard Children’s Hospital. “This verification aligns with our mission to improve the health and well-being of eastern North Carolina by ensuring patients receive prompt and specialized critical care, right here in our region.”

According to the ACS, Level I Trauma Centers must be capable of providing system leadership and comprehensive trauma care for all injuries. In its central role, a Level I Trauma Center must have adequate depth of resources and personnel. Most Level I Trauma Centers are university-based teaching hospitals due to the resources required for patient care, education and research. In addition to providing acute trauma care, these centers have an important role in local trauma system development, regional disaster planning, increasing capacity and advancing trauma care through research.
“Being a Level I Pediatric Trauma Center reaffirms our ability to provide timely, life-saving care for pediatric trauma patients,” said Dr. Shannon Longshore, pediatric trauma surgeon and medical director of the pediatric trauma unit, ECU Health Medical Center. “We see pediatric patients with injuries as the result of falls, motor vehicle collisions, ATV and dirt bike accidents and firearm injuries. The change from Level II to Level I demonstrates Maynard Children’s Hospital’s ability to maintain the highest level of care for patients and advance research publications, national presence as a trauma center and community outreach.”
In Fiscal Year 2023, ECU Health Medical Center cared for a total of 4,057 patients – 3,721 adult and 336 pediatric cases. Nearly 60 percent of patients at ECU Health Medical Center and Maynard Children’s Hospital are transferred in from other hospitals for a higher level of care; the national average is 30 percent.
ACS listed the following as major strengths of the Pediatric Trauma Program: The Eastern Carolina Injury Prevention Program, the outstanding commitment and quality of care provided by the adult trauma/acute care surgeons, availability of whole blood for pediatric trauma patients, three trauma bays, having at least two radiologist in-house 24/7 performing reads and available for consultation, neurosurgical and orthopedic support, disaster management planning and pediatric rehabilitation center.
Maynard Children’s Hospital was previously verified as a Level II Pediatric Trauma Center first in 2017. The verification lasts for three years, until February 2027. ECU Health Medical Center has been a Level I Trauma Center since 2005 and recently received re-verification in 2024.

“Maynard Children’s Hospital and ECU Health Medical Center serving as the sole Level I Trauma Centers in eastern North Carolina underscores the value of having a robust system of care with different levels of specialization, ensuring patients receive timely and appropriate treatment for all injuries, from pediatric to adult cases,” said Brian Floyd, chief operating officer, ECU Health. “Maynard Children’s Hospital’s recent verification as a Level I Pediatric Trauma Center reflects ECU Health’s commitment to clinical excellence and academic research, leading to tangible, life-saving benefits for the communities and patients we serve.”
Asthma is a chronic lung disease that causes inflammation and swelling of the airways, and it affects an estimated five million children in the United States. The annual economic cost of asthma is more than $81.9 billion, and in children ages 5-17, asthma is the number one cause of school absenteeism and is among the top reasons for pediatric emergency department (ED) visits and hospital admissions.
World Asthma Day, which is May 7, seeks to raise awareness about asthma and improve the lives of all people with asthma. The ECU Health Regional Pediatric Asthma Program has similar goals, including to reduce ED and inpatient admissions for children with asthma, decrease school absenteeism and to increase the quality of life for asthmatic children in eastern North Carolina. It does this by offering asthma testing, asthma education, tools to manage asthma, access to community resources and medication assistance. Their work with eastern North Carolina public schools has been a particularly effective way to reach children in rural North Carolina communities.

The ECU Health Regional Pediatric Asthma Program, first begun in 1995, initially served Pitt and Greene counties. The pilot program was a partnership between the ECU Health Maynard Children’s Hospital, Community Health programs and a local elementary school. In 1996, the hospital was awarded a three-year grant from the Duke Endowment to further support the development of a comprehensive pediatric asthma program model that focused on children in grades K–5. As a result, they saw a 40% decrease in ED visits by school-aged children, a 50% decrease in student absences and a 50% decrease in inpatient cost of care for school-aged asthmatic children.
The program has since expanded to serve 29 counties in eastern North Carolina, and the number of public schools served has increased to 16.
“Our legal team and the school boards establish contracts with the elementary schools that renew on a rolling basis, and these allow us to do asthma testing, communicate with parents, liaise with the children’s PCPs, help the kids access medication and ensure they are compliant,” said Bailey Edwards, respiratory care manager of the Pediatric Asthma Program. A respiratory therapist who has worked at ECU Health for nine years, Edwards joined the team after working bedside in the NICU and PICU. “I saw so many kids with asthma come through our hospital with severe symptoms.”
In addition to Edwards, the team is comprised of a medical director, a social worker, nurses and three additional RTs. Edwards and the team have worked hard to grow and improve the Pediatric Asthma Program’s scope. Once a child is referred by the school nurse, an asthma care manager contacts the parents for the consent to treat.
“I call the parents and introduce myself, tell them about the program and learn more about their child,” Edwards said. Then, Edwards goes to that child’s school and performs a fractional exhaled nitric oxide (FeNO) test with the child, which determines how much lung inflammation is present and how well inhaled steroids suppress that inflammation.
“Some of these kids have outrageously high FeNOs but didn’t know it – they didn’t realize they couldn’t breathe,” Edwards said. “I call their doctor after my assessment and let them know my findings and recommendations. Then we figure out how to get the child what they need.”
Medications are a key part of the child’s treatment, but often their families cannot afford them.
“We provide medications for free or at low cost through a Children’s Miracle Network Hospitals grant. These medications can keep kids out of the hospital,” Edwards said.
The asthma team also provides education to the children and their parents about how to use the medications properly and potential causes of asthma exacerbations, such as tobacco smoke, dust, weather change or exercise. Once a treatment plan has been established, the asthma team follows up regularly for several months to ensure the child is compliant and the plan is effective.
“A month after initial treatment, I often hear parents say, ‘My kid is my kid again,’ and the child is laughing and playing because they can breathe,” Edwards said.
The program’s reach into public schools continues to grow; nine more schools have pending contracts.
“Our outreach to schools is based on what we see in the emergency departments and hospitals,” Edwards said. “Once we identify these problem areas, we connect with primary care physicians and school nurses to establish relationships.”
Many of those connections are made through lunch and learns the team hosts at regional schools.
“We bring treats and give an hour presentation about our services, update the school nurses on asthma guidelines and tell them how they can refer to us,” she said. Doing this has allowed the program to get many more referrals. “What started as a trickle has now turned into a waterfall.”
Going through the schools, said Sue Anne Pilgreen, manager for the Pediatric Asthma and Eastern Carolina Injury Prevention Programs (ECIPP), is the best way to connect with children in rural areas.
“It is impossible for us to physically be in every county, but our regional partnerships with school nurses and primary care providers gives us a direct pipeline to these children, and they know we are only a phone call or school visit away,” Pilgreen said. “We take a holistic approach in caring for our patients and their families, and sometimes that means helping them find better housing, reliable transportation or mental health resources. Looking at a family’s social determinants of health and helping to fill some of those gaps is a critical piece of caring for children in eastern North Carolina.”

This program aims to overcome the disparity in health care options for many of the children they treat.
“You see families with no food, no electricity and no ability to afford medicine,” Edwards said. “The parents don’t want to take their kids out of school to see the doctor because that child has already missed so much school because of their asthma, and they can’t afford to take the time off work themselves. This program strives to eliminate those barriers.”
While the public school outreach is a major part of the program, it’s not the only way they are treating asthmatic children in rural North Carolina.
“We work with Dr. William Wooten, our medical director, in having monthly pulmonary clinics that provide specialty level care in places that don’t have those resources,” Edwards said. “It started in Jacksonville and moved to Richlands. Now we have three clinics — Richlands Pulmonary Clinic, ECU Tarboro and ECU Edenton — and more locations requesting clinics of their own.”
Like the school outreach, these clinics reduce the burden for families who cannot travel farther away.
“We’re cutting into that lack of transportation or gas money,” Edwards said. “And in places that don’t have clinics, we are gaining more school contracts.”
Looking forward, Edwards said the next goal is to increase their scope of research and apply for more grant money.
“We applied for a Vision Grant, which we should hear about this summer, and we are exploring research options, especially ones that demonstrate the program’s efficacy,” Edwards said.
These efforts will support the program’s continued growth and help them meet new opportunities to better serve eastern North Carolina.
That’s important, Edwards said, because since 2021, they’ve seen a 378% increase in the number of referrals and a 312% increase in the number of cases managed. This program, she emphasized, is unique in that it helps children and their families understand asthma so they can control it and have a high quality of life.
“There’s no program in North Carolina like us, and a lot of people reach out to us about what we’re doing,” Edwards said.
The program is always looking for more effective and efficient ways to reach families, because children with asthma are often invisible to those not looking for specific symptoms.
“You see a kid at school who doesn’t speak above a whisper or doesn’t speak in complete sentences. They don’t run around and play. They look fine, but to someone who is trained, you can tell their asthma isn’t well controlled,” Edwards said. “Asthma can go dormant and then come back; it can silence you. But this program can set you up for the rest of your life.”
Resources
While the East Carolina University (ECU) baseball team is rounding into form as postseason play nears, they’re also taking time out to make a special difference in their community.
After a visit to ECU Health Medical Center last November, as part of a career shadowing opportunity, senior first baseman Carter Cunningham felt compelled to do something to help patients and families.
“I’d been praying for ways to give back to the community,” Cunningham said. “As we’re doing a tour of the entire campus, we walked into the [Maynard] Children’s Hospital and it was like God had smacked me in the face. It was like, this is what I have to do. I didn’t know what it would look like yet, though.”
He said that week, he went back to the team and asked for a small donation from everyone to spread some holiday cheer to patients and families at the children’s hospital. The response was more than he expected.

“We got about $500 and we were able to drop off some presents to the children’s hospital right before break,” he said. “It was awesome. We had about 20 players come in and we hung out in the playroom and had a great time.”
Tara Tadlock, a child life specialist at Maynard Children’s Hospital, said patients and families would subsequently talk about the visit for the next month. The same held true for Cunningham and his teammates, who also went on talking about how special the visit felt.
He said over the Christmas break he took more time to think about what he could do to make an impact for patients and families like those he’d met a few weeks before. Then the idea to start a foundation, Homers That Help, came to him.
It started with a call for donations on social media, one sponsor for each of ECU’s 33 home baseball games in 2024. The sponsor makes an up-front donation to the fund and an additional donation for each home run hit during the game. While he expected to need some time and make some calls to fill every game, the fund was complete after about 15 hours.
“The community here, I can’t describe it,” Cunningham said. “I get goosebumps talking about it because they’re so generous and so supportive, not only of ECU athletics, but the whole community. It was a testament to all the people that are here and I’m thankful and blessed to have an opportunity to be here.”
Because of the outpouring of support, Cunningham opened a “Fund B” for those who were not able to directly sponsor a game but still wanted make a donation. Cunningham is making donations himself as well, contributing $25 to the fund for each of his own home runs. With nine home runs, Cunningham is tied for the team lead and backing up his own efforts.
Along with the funds, which Cunningham and Tadlock recently started to distribute to patients and families, Cunningham and his teammates are continuing to make bi-weekly visits to the Maynard Children’s Hospital. He said taking a step back to give time to others is important to him.
“As a Division I athlete, you get so caught up in the games and practices, the wins, the losses, but every other Monday it’s just eye-opening,” he said. “I’ll never forget one patient, the day before we went to play Campbell, he said, ‘Have fun at your game tomorrow.’ It was so refreshing and offered great perspective. It’s way bigger than baseball. These visits are the best part of my week every time I visit.”
Tadlock said the program has been a great benefit for everyone involved and she’s looking forward to its continued success.

“I’ve been doing this for a long time with scheduling our visitors and working in Child Life and these visits are a bright spot of our month, too. It’s great to see the patients and families so excited, seeing the guys so excited and knowing that they’re making a difference for our patients is huge,” Tadlock said. “Some of the kids that are here are going through really hard stuff and finding out hard news. If they’re able to leave that behind for a few minutes and hang out with the ECU baseball team, it’s really important to try to create those special moments. All we want to do in Child Life is provide some normal experiences for the children. Working with this team has been amazing.”
Though this is Cunningham’s last year at ECU, he said the plan is for Homers That Help to carry on. He’s looking to younger members of the team to pick up the torch and build upon the positive momentum the foundation has today.
Resources
To be a health care provider is to answer a calling. For some, the journey to health care is a straight line; for others, the road is winding. This series features stories from ECU Health team members who took the winding road, but found the destination to be worth the effort.
Lacey Boldyrev, staff nurse II in the Pediatric Intensive Care Unit (PICU), has worked for ECU Health since 2020. “I started in the middle of COVID,” she said. “My last semester of nursing school was entirely online and we weren’t even allowed to go into the hospital for clinicals, so it was a challenge.” Prior to attending Coastal Carolina Community College for her RN degree, Boldyrev was a stay-at-home mom while her daughters were young, and once they went to school, she pursued her dream of being a teacher.
“I started school but didn’t finish my degree,” Boldyrev said. “I was a substitute teacher and a paraprofessional in Brooklyn, where we lived, for seven years.”
At that time, she and her family moved to North Carolina where she worked in a preschool at Camp LeJeune until the birth of her son.
“He was born at Onslow Memorial Hospital,” Boldyrev said. “We had a normal pregnancy and ultrasounds, nothing special. But after he was born and I went to get him, they told me I couldn’t pick him up. They told me to return to my room and the doctor would see me.”
It was at that moment Boldyrev learned that her son had congenital heart disease and the hospital was sending him to Maynard Children’s Hospital at ECU Health Medical Center in Greenville. “I had never had a child with health issues before,” Boldyrev said. “All of the sudden we’re living in a hospital for a year and a half and taking medical flights to different states.” Her son died on Christmas Day, 2015.
“After he was gone, there was this big empty hole,” Boldyrev shared. “I didn’t know what to do with myself.” The time she spent with her son in the hospital, she said, inspired her to pursue a degree in nursing. “I had given him his medications and his oxygen and feeding tubes,” she said. “All these things I’d done for him, and I learned from the nurses taking care of him. I took that as a sign.”
Although she had never previously considered a career in health care, her work with children in education set a foundation for how to communicate with kids and their families in the hospital. “I understood from my work in the schools some of the challenges children face and how they develop,” Boldyrev said.
After graduation, Boldyrev knew she wanted to work at Maynard Children’s Hospital. “Everyone who was working there when my son was there treated me with such compassion and listened to me. The PICU was the only place I wanted to be; I’m not sure I’d be as happy if I was anywhere else.”
Part of what makes her work so special, Boldyrev said, is the PICU team. “The reason I came back to Greenville, and keep in mind I commute over an hour to get here, is my team,” she said. “The people I work with provide exceptional care. Not once since I started have I felt alone or that my team doesn’t have my back. There are other places I could work that are closer but that’s not what makes a good job. It’s the people and the pride you take from what you do.”
Boldyrev’s experience with her son has given her a unique perspective for the patients and families she serves in the PICU.

“You don’t know anything about what it’s like if you’ve never had an unhealthy child. When my son was born, it opened a new world. I didn’t even know what congenital heart disease was, but now it’s unfathomable that I didn’t know,” she said. She recognizes that working in health care can be challenging, but it’s also the most rewarding thing she’s ever done. “If you’re passionate about medicine and helping people, but you’re hesitant to start the journey into health care, I say put your fears aside and take that first step.” Being able to provide compassion and support to children and families is something she’s very proud of, and she’s glad she took that first step. “I can be there for families going through the same type of situation I experienced,” Boldyrev said. “I feel like I’m able to make a difference in their lives. I believe there are reasons why we’re set on a path, and I take a lot of pride in saying that I’m a nurse.”
