Seven key priorities served as the central discussion point as community-based health partners joined ECU Health and Pitt County Department of Social Services (DSS) in October for the second session of a conference series designed to support the emergency department and improve access to non-emergent care across eastern North Carolina.
The seven key priorities, identified during the first conference session in early October, represent the unique viewpoints from stakeholders across the community and all of whom share a common goal: reduce unnecessary utilization of the emergency department in Greenville.
The seven priorities include:
- Placement/disposition – getting patients placed in the appropriate care settings outside the emergency department such as skilled nursing facilities, in-home care, adult care homes, foster homes, etc.

- Navigating the system – defining roles and responsibilities of each agency
- Collaboration – improve collaboration among systems and across agencies
- Crisis system – more clearly defining how the system operates and clarifying any confusion that may exist
- Community options and wraparound support – ensure a robust support system in the health care setting and in the community to ensure people get the help they need
- Access to services – provide clarity on where patients need to go to access care
- Regulatory – reduce barriers and create efficiencies in key operational areas like timely discharge and clinical assessments
“This was a moment for us as a health care community to not only clearly define the challenges facing the patients we serve, but to also explore how we can implement solutions that improve the emergency care realities here in eastern North Carolina,” said Jacob Parrish, vice president of capacity and throughput at ECU Health, who served as one of the conference organizers. “The challenges facing emergency departments both locally and nationally cannot be solved solely by the hospitals themselves. These conversations help us take our words and put them into collaborative action.”
Health care and community partners in attendance at the conference included ECU Health, DSS Directors from across eastern North Carolina, Juvenile Justice, Trillium Health Services, Public School leaders, NC DHHS, payors, faith leaders, and other eastern North Carolina hospitals and key stakeholders. The conversation focused on both adult and pediatric/adolescent patient populations who present at the emergency department but could be better served in a different setting.
The importance of education and outreach served as a common theme throughout the discussion. Organizations talked not only about the importance of providing critical information directly to patients, but also emphasized the importance of educating themselves on the role that other organizations and agencies play in the care continuum.

ECU Health highlighted the growing demand for emergency department services and the urgent need to streamline care in the community for non-emergent cases. The discussions underscored how patients with non-critical issues are often funneled to emergency departments due to limited access to routine and primary care resources and crisis services, creating unnecessary strain on EDs. ECU Health Medical Center, for example, remaining full nearly half the year due to high patient volumes, which often exceed its 974-bed capacity. This backlog directly impacts how long some patients may wait in the ED.
“Our commitment to improving emergency care access and efficiency for our patients is unwavering,” said Dr. Leigh Patterson, chief of services for emergency medicine at ECU Health Medical Center. “The collaboration we’re seeing across health care and alongside our community partners demonstrates a shared dedication to creating lasting solutions that serve the unique needs of eastern North Carolina.
By addressing the root causes that lead to emergency department overutilization, we’re working to not only improve the experience for our patients but also strengthening health care in our region.”
ECU Health and Pitt County DSS will host a third session of the conference to further discuss action items and strategies to support more collaboration in the community.
It was a packed house at ECU Health’s Monroe Conference Center on Oct. 1, as ECU Health and Pitt County Department of Social Services (DSS) welcomed dozens of community-based health partners for a conference designed to help tackle a complex challenge: reducing unnecessary emergency department utilization to ensure enhanced access for those needing emergency care.
It is no secret that overcrowding in emergency departments is a challenge facing hospitals across the country. ECU Health Medical Center, the only Level I Trauma Center in ECU Health’s 29 county service area, is no exception. The medical center serves a largely underserved rural region where access to care is difficult for many. That includes primary care, behavioral health care and other services best rendered in outpatient settings. Combined with a disproportionate number of uninsured community members, this lack of access to care means patients often times end up at hospital emergency departments.
Dr. Leigh Patterson, chief of services for emergency medicine at ECU Health Medical Center and chair of emergency medicine at the Brody School of Medicine at East Carolina University, said ECU Health’s nine hospitals will see nearly 250,000 visits to the emergency department this year, with more than half of those occurring at the medical center. She said conversations with key community health leaders, like the one hosted by ECU Health and Pitt County DSS, can help ensure community members are aware of, and have access to, non-emergent health care resources outside the emergency department setting.

“When I look at what happens inside the emergency department, I see the opportunity for us to help fill the care gaps that exist outside of it,” Dr. Patterson told the group, noting that she sees about 225 adult patients per day in the medical center ED, about 40% of whom could be more appropriately served in an outpatient setting. “When it comes to addressing this problem, it will take all of us as a health care community to make meaningful change. That’s why I’m heartened that so many of you have joined us today to work together toward solutions that make an impact in our community.”
The conference represented true regional community collaboration. Health care partners present at the conference included ECU Health, DSS Directors from across eastern North Carolina, Juvenile Justice, Trillium Health Services, Public School leaders, NC DHHS, payors and other eastern North Carolina hospitals and key stakeholders.

“The ECU Health/Pitt County DSS ED conference was an excellent example of cross system collaboration,” said conference co-sponsor Sharon Rochelle, director, Pitt County DSS. “This was a day to build mutually beneficial partnerships that have common goals to better serve the children and adults of the community.”
The conversation focused on both adult and pediatric/adolescent patient populations and heavily examined the challenges that behavioral health patients face accessing care. Despite the new inpatient behavioral health hospital slated to open in Greenville in 2025, those in attendance agreed that the issue needed immediate attention which involves creating increased interconnectedness among those providing care both in the community and in the hospital setting.
“We are grateful for all agencies involved in this important and challenging work,” said Jacob Parrish, vice president of capacity and throughput at ECU Health. “We know that the complex challenges we face cannot be solved at emergency departments alone. We are fortunate to have so many committed partners who share our vision for continuous improvement through strong relationships and close collaboration. Together, we can ensure the highest quality of care for communities across the East.”
The recent meeting was the first day of the two-day conference, largely centered around examining the issues through open and honest conversations. Those in attendance will reconvene later in the month for the second meeting to develop an action plan with concrete steps and strategies for improving access to care and reducing unnecessary ED utilization in eastern North Carolina.
“This is a complex set of issues, but I am confident we have the right people in our community committed to finding the solutions,” said Brian Floyd, ECU Health chief operating officer. “While these challenges are not exclusive to our health system or region, I know that together we can help support our emergency departments and improve the experience for those needing access to high-quality emergency care which is rendered at our hospitals every single day.”
Resources
As part of its mission, ECU Health prides itself on readiness to respond to any emergency scenario that could impact the health and well-being of the people we serve. Preparedness is imperative for a health system, especially when facing potentially unpredictable emergencies.
ECU Health Medical Center recently hosted a training exercise centered around a Chempack container from the Strategic National Stockpile, part of the Administration for Strategic Preparedness and Response. The containers contain antidotes to treat the symptoms of a nerve agent exposure in response to a possible chemical incident.
“While we hope never to encounter such extreme situations, like a chemical incident, being ready to respond is essential to protect our patients and communities,” said Chris Starbuck, manager of the Eastern Healthcare Preparedness Coalition at ECU Health Medical Center. “Training for scenarios ensures that the ECU Health team is equipped to act swiftly and effectively.”

Team members from across ECU Health, including pharmacists, pharmacy team members, EastCare providers, hospital police and Emergency Management personnel, partnered with Pitt County EMS to learn more about the nationwide Chempack program. The training, led by Monica Ricks, PharmD, with NC Public Health Preparedness and Response, included an overview of possible scenarios where Chempacks may be needed and their vital role in responding to chemical emergencies.
“The Chempack program began in 1983, and luckily we have never had to deploy one,” said Starbuck. “However, a large scale chemical incident like what happened in Japan in the mid-1990s would have very negative consequences to the patients and to our health care system. I’m thankful that as a health system, we continue to prioritize preparedness through ongoing education and training. In the coming months we will conduct a table top exercise with more partners that will lead up to a regional full scale exercise.”
Learn more about how ECU Health and the Eastern Healthcare Preparedness Coalition proactively plan to help care for our region: www.easternHPC.com
ECU Health emergency medicine residents took time away from their regular Wednesday morning classroom sessions and dove into an Emergency Medicine Wilderness Day exercise at Wildwood Park in Greenville.
On May 29, about 20 emergency medicine residents spent their morning in small groups, walking around the park and encountering “patients” with different ailments. From poisoning to animal attacks and drowning scenarios to firework accidents, the experience helped residents prepare for real-world scenarios and eventual board exams. Residents received real-time instruction and feedback from the Brody School of Medicine at East Carolina University faculty as they worked through their training.
The patients for this exercise were standardized patients from Brody’s Office of Clinical Skills Assessment and Education. Standardized patients are trained to mimic real patients so that students can learn. Their role is to help prepare future health care professionals for a variety of patient interfaces.

Dr. Sarah Thead is a second-year emergency medicine resident at ECU Health and said she’s attended the training the last two years and has benefited from the experience.
“It’s a great educational experience every time we do this,” Dr. Thead said. “It’s scenario-based and our faculty try to set up the scenarios similar to how they’ll be set up on our oral board exams, so it’s a fun experience but also really important from an educational perspective as well.”
She said the scenarios change from year to year which helps her and her co-residents as they try to work together and think quickly to help patients experiencing a medical emergency.
Dr. Jennifer M. Bennett, an emergency medicine physician at ECU Health, clinical assistant professor of emergency medicine and medical director of the Simulation Center at Brody, said this kind of exercise is important for a number of reasons.
“It’s a great opportunity to demonstrate how we can all work together, even outside of the emergency department. It’s important to work on these skills in a different environment,” Dr. Bennett said. “It’s also a good opportunity to have some team bonding for the residents. Just getting them out for a day and letting them do something a little bit different, getting them out in the sun, that’s a positive as well.”
Dr. Bennett said having Wildwood Park available to run this exercise has helped this program thrive over the last three years.
Along with Dr. Bennett, Dr. Jennifer Parker-Cote, assistant professor of emergency medicine at Brody, helped to create the simulation and organize the event.
In Dr. Parker-Cote’s simulation, residents had to assess a camper who had ingested a toxic mushroom in the woods. Residents assessed the standardized patient, asked about the patient’s medical history and made recommendations on next steps for care.
“These scenarios allow residents to apply the knowledge they’ve gained through their residency and apply it to real world situations and permits them to improvise in wilderness medicine, which you have to do a lot of times,” Dr. Parker-Cote said. “It’s important to put them through these simulations and have them think critically while working together and trying to move quickly to help our standardized patients.”

The training is another example of the valued partnership between ECU Health and Brody. Residents at an academic health system like ECU Health have support and resources for continued education from faculty and the Interprofessional Clinical Simulation Program at Brody, enriching their clinical training experience. Residents participate in trainings like this to prepare for real situations with real patients both behind the walls of the hospital and out in the community.
Resources
When Dr. Shannon Longshore, the medical director of the pediatric trauma program at ECU Health Medical Center, first joined the hospital, the James and Connie Maynard Children’s Hospital at ECU Health Medical Center wasn’t a verified pediatric trauma center. Now, Maynard Children’s Hospital is one of only four Level I Pediatric Trauma Centers in North Carolina and the only one serving the East.
“It is incredibly fulfilling to reflect on the growth we have experienced over the years, to now achieving verification as Level I Pediatric Trauma Center,” Dr. Longshore said. “Our teams across ECU Health have dedicated their work to constantly improving our care over the course of many years. From prevention, to treatment, and being entrusted to provide critical care at the highest level, this verification is a testament to the mission-driven work that defines our hospital and health system.”

The American College of Surgeons’ (ACS) Verification, Review and Consultation (VRC) Program is designed to assist hospitals in the evaluation and improvement of trauma care and provide objective, external review of institutional capability and performance, accomplished by an on-site review of the hospital by a peer review team experienced in the field of trauma care. There are three levels of ACS trauma center verification, with Level I being the highest verification a trauma center can achieve.
Level I Trauma Centers must be capable of providing system leadership and comprehensive trauma care for all injuries and have adequate depth of resources and personnel. These centers play an important role in local trauma system development, regional disaster planning, increasing capacity and advancing trauma care through research.
Recognizing excellence in pediatric trauma care and community outreach
Dr. Longshore herself has been instrumental in Maynard Children’s Hospital’s continued growth as a trauma center through her research and presentations at national conferences and her work with the Eastern Carolina Injury Prevention Program (ECIPP).
The ACS surveyors noted the value of ECIPP, which aims to create a safer environment, change behavior and change policy to improve the quality of life in eastern North Carolina. Sue Anne Pilgreen currently serves as the executive director of the Safe Communities Coalition and the manager of ECIPP, which has been around since 1995. Between 2020 and 2023, ECIPP was awarded more than $1 million in grant funding, which has supported work in areas such as teen driver safety, suicide prevention, firearm safety, and child passenger and bike safety.
“The surveyors were especially impressed with our work around firearm safety and suicide prevention,” said Pilgreen. “We utilize the pediatric trauma registry data, and that is what drives our work.”
Pilgreen was quick to commend ECIPP team’s work in all areas to prevent injuries, and she highlighted that while most trauma programs have one injury prevention person, ECU Health has an entire team. That enables the program to reach out to rural communities and establish new injury prevention processes.
“Even with our incredible injury prevention team, we recognize that injuries will happen,” said Pilgreen. “To have this Level I Trauma Center with the best of the best gives the opportunities for the best outcomes.”
Other specific strengths noted during the pediatric program’s survey included the addition of two pediatric orthopedic surgeons and a pediatric neurosurgeon; outreach clinical simulations in the region; the collaboration among the pediatric orthopedic surgeon, the neurosurgeon and the Pediatric ICU (PICU); and the recent renovation of the PICU to establish a family-friendly place to care for patients. Of note, a large strength also lauded was the academic research and a collaboration with the Brody School of Medicine at East Carolina University’s Department of Pediatrics.
This expansion of the pediatric trauma research footprint was accomplished through more than 10 publications in nationally recognized journals. Both Erika Greene, manager of the pediatric trauma program, and Elizabeth Seawell, manager of the adult trauma program, credited the collaboration with Brody to produce research and get articles accepted to journals.
“That was a big win for us,” Greene said. “We have an academic medical center with the resources and processes in place to care for injured patients, and we’ve done an amazing job to achieve Level I for pediatrics. We have the capabilities to take the best care of those patients to the highest level of the accrediting body.”
Sustained excellence in adult trauma care
The pediatric trauma center’s new Level I verification accompanies the ECU Health Medical Center’s adult trauma center re-verification of Level I, a title they have proudly held for 40 years.
“We were one of the first Level I Trauma Centers in North Carolina, and we were verified by the American College of Surgeons in 2005,” said Seawell. “We are recognized nationally for how we care for patients in a rural area.”
This recent re-verification was made possible in part due to the resources available to the program including neurosurgical, interventional radiology, orthopedic trauma neurology, and vascular resources, operating room capabilities and blood access, as well as a trauma team of 11 surgeons.

“We are the only Level I Trauma Center for 29 counties, and to reach that far and care for that many patients – we served more than 4,000 patients last year – we have to rely on local community hospitals and emergency response teams to ensure timely transfers and communication,” said Seawell.
Seawell noted that ECU Health Medical Center and Maynard Children’s Hospital have a 60 percent transfer in rate, when the national average is 30 percent, which means they work closely with local EMS agencies, regional transfer facilities, other ECU Health organizations and non-affiliated organizations to serve patients from all over the region.
“The role of our trauma program is to not transfer patients but to have all the resources we need. It provides excellence in patient care and helps keep our patients local,” said Seawell.
Dr. Eric Toschlog, medical director of the adult trauma program, emphasized the tremendous preparation required to achieve Level I. He noted that there are more than 100 standards to prepare for, including paperwork, infrastructure, teamwork and more.
“The visit from ACS is a two-day adventure in stress and anxiety,” Dr. Toschlog said. But at the conclusion, he felt immense pride. “This visit was my seventh in 24 years at ECU Health, and it was clearly our best; we were found to have no deficiencies, and the reviewers used words such as ‘exemplary’ and ‘blown away’ regarding multiple aspects of the trauma center.”
Having two Level I Trauma Centers at ECU Health is no small thing, and both centers achieving the highest level of care is due to the dedication of the trauma center teams.
“I am surrounded by brilliant, compassionate, hardworking, mission-driven individuals who share a singular vision of saving the lives of the patients we have the honor to care for each year. Our success is owed to those truly extraordinary people,” Dr. Toschlog said.
Greenville, N.C. – James and Connie Maynard Children’s Hospital at ECU Health Medical Center received verification from the American College of Surgeons (ACS) Committee on Trauma as a Level I Pediatric Trauma Center, becoming one of only four in the state. Maynard Children’s Hospital now joins ECU Health Medical Center as the only Level I Trauma Centers in eastern North Carolina.
“We are proud of the dedication that all of our team members at Maynard Children’s Hospital have made to prioritizing the delivery of high-quality care close to home, and achieving Level I Trauma Center verification is a demonstration of that commitment,” said Tara Stroud, vice president, Women’s and Children’s Services, Maynard Children’s Hospital. “This verification aligns with our mission to improve the health and well-being of eastern North Carolina by ensuring patients receive prompt and specialized critical care, right here in our region.”

According to the ACS, Level I Trauma Centers must be capable of providing system leadership and comprehensive trauma care for all injuries. In its central role, a Level I Trauma Center must have adequate depth of resources and personnel. Most Level I Trauma Centers are university-based teaching hospitals due to the resources required for patient care, education and research. In addition to providing acute trauma care, these centers have an important role in local trauma system development, regional disaster planning, increasing capacity and advancing trauma care through research.
“Being a Level I Pediatric Trauma Center reaffirms our ability to provide timely, life-saving care for pediatric trauma patients,” said Dr. Shannon Longshore, pediatric trauma surgeon and medical director of the pediatric trauma unit, ECU Health Medical Center. “We see pediatric patients with injuries as the result of falls, motor vehicle collisions, ATV and dirt bike accidents and firearm injuries. The change from Level II to Level I demonstrates Maynard Children’s Hospital’s ability to maintain the highest level of care for patients and advance research publications, national presence as a trauma center and community outreach.”
In Fiscal Year 2023, ECU Health Medical Center cared for a total of 4,057 patients – 3,721 adult and 336 pediatric cases. Nearly 60 percent of patients at ECU Health Medical Center and Maynard Children’s Hospital are transferred in from other hospitals for a higher level of care; the national average is 30 percent.
ACS listed the following as major strengths of the Pediatric Trauma Program: The Eastern Carolina Injury Prevention Program, the outstanding commitment and quality of care provided by the adult trauma/acute care surgeons, availability of whole blood for pediatric trauma patients, three trauma bays, having at least two radiologist in-house 24/7 performing reads and available for consultation, neurosurgical and orthopedic support, disaster management planning and pediatric rehabilitation center.
Maynard Children’s Hospital was previously verified as a Level II Pediatric Trauma Center first in 2017. The verification lasts for three years, until February 2027. ECU Health Medical Center has been a Level I Trauma Center since 2005 and recently received re-verification in 2024.

“Maynard Children’s Hospital and ECU Health Medical Center serving as the sole Level I Trauma Centers in eastern North Carolina underscores the value of having a robust system of care with different levels of specialization, ensuring patients receive timely and appropriate treatment for all injuries, from pediatric to adult cases,” said Brian Floyd, chief operating officer, ECU Health. “Maynard Children’s Hospital’s recent verification as a Level I Pediatric Trauma Center reflects ECU Health’s commitment to clinical excellence and academic research, leading to tangible, life-saving benefits for the communities and patients we serve.”
ECU Health EastCare participated in the impactful Prom Promise initiative, engaging students at both Perquimans County High School and Richlands High School on April 23 and 24, respectively. The objective was clear: to dissuade teens from driving under the influence during prom season through vivid reenactments of motor vehicle accidents.
Before the re-enactment, students were presented with facts about the dangers of drinking and driving. According to Prom Promise’s founding organization The Prevention Network, one-third of all teen deaths occur in alcohol-related collisions between April and June, and nearly 41% of teens ages 16-19 are likely to drink or use drugs during or after prom.
Chuck Strickland, EastCare’s outreach coordinator at ECU Health, expressed the initiative’s goal of leaving a lasting impression on students, steering them away from driving under any form of impairment.

The events featured realistic depictions of crashed vehicles, complete with students portraying injuries resulting from the collisions. The students witnessed the arrival of first responders who initiated care and extricated individuals with the Jaws of Life, a tool used by emergency rescue personnel to assist in the extrication of victims involved in vehicle accidents. An EastCare helicopter landed on the scene as part of the demonstration, underscoring the importance of quick response required in such emergencies.
“I want to extend my heartfelt appreciation to our local first responders for their invaluable partnership and unwavering dedication in making our DWI reenactment crash demonstration a success,” said Steve Clarke, principal, Richlands High School. “Their professionalism, expertise and commitment to ensuring the safety and well-being of our students and community are truly commendable. We are grateful for their continued support and collaboration in our efforts to educate and empower our students to make responsible choices and prioritize safety at all times.”
Through collaborative efforts and a commitment to education, ECU Health and its partners aspire to instill responsible decision-making and prioritize safety among students – not only during prom season but throughout their lives.
The Eastern Healthcare Preparedness Coalition (EHPC) recently hosted a regional chemical and radiological tabletop exercise at the ECU Health Monroe Center with local and state partners, including those from hospitals, EMS, EastCare, public health, emergency management, hazmat teams from the Williamston Regional Response Team, and specialists from the 42nd Weapons of Mass Destruction Civil Support Team.
The tabletop exercise – intended to help ensure joint response coordination in response to a large-scale chemical or radiological event – included a brief training session followed by a plausible scenario that led to discussion of possible outcomes and discovery of gaps in preparedness planning.
Following the exercise, an after-action plan will be developed, followed by measures to ensure areas of opportunity are addressed.
The goal, according to event organizers, is to ensure all agencies are best prepared to serve the community.
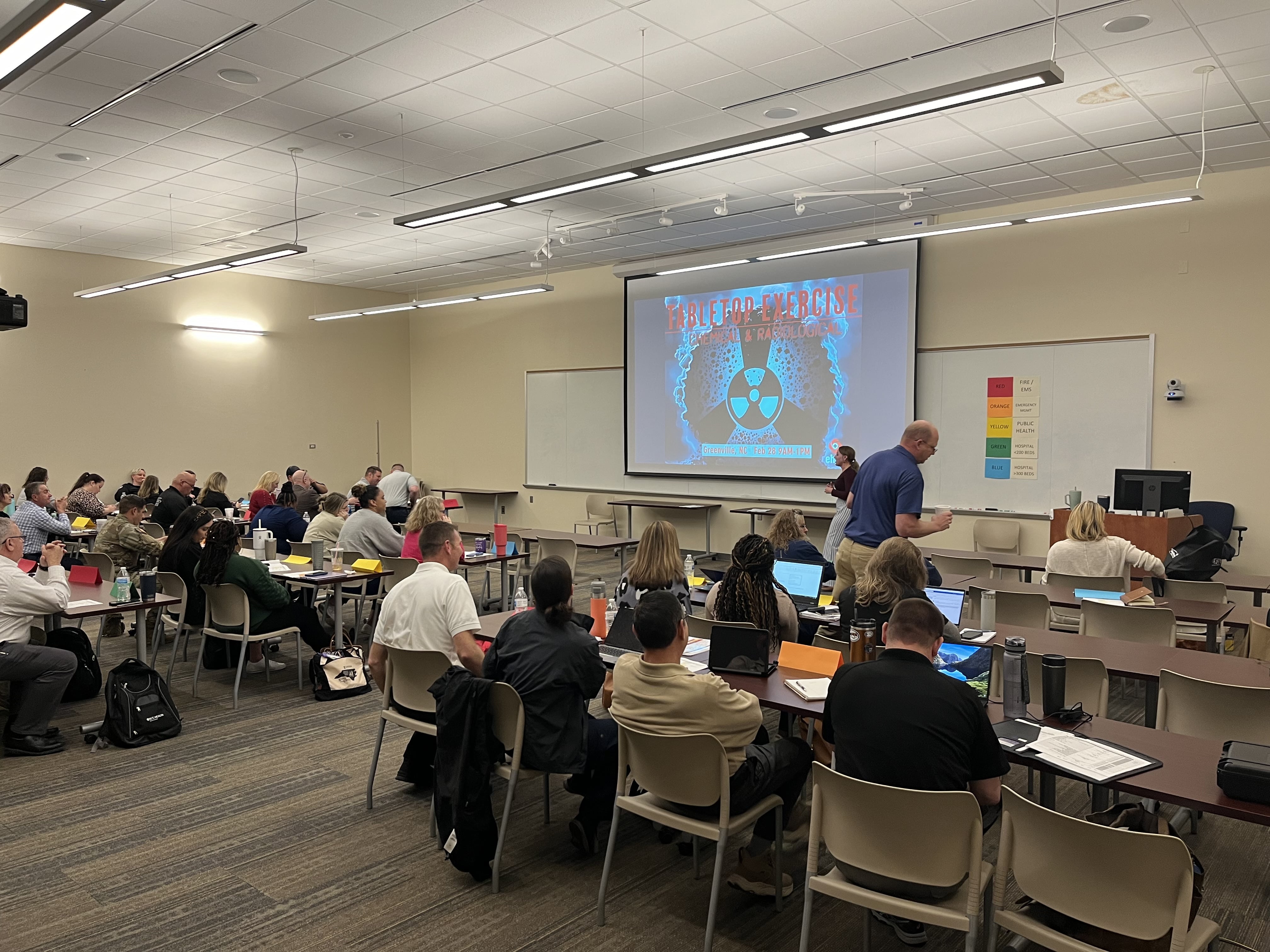
“The tabletop was a fantastic opportunity to collaborate with partners and learn more about regional capabilities available to respond to a radiological incident,” said Christa Radford, Industrial Hygiene Consultant – Eastern Region at the North Carolina Department of Health and Human Services Public Health Preparedness and Response. “EHPC did a great job planning this exercise and bringing the correct response partners together for an extremely successful event.”
EHPC is a multidisciplinary team of medical and nonmedical professionals, established to provide mobile medical support for short and long term disasters or catastrophic events in eastern North Carolina. Roles in which the EHPC can provide support include set up and provision of a mobile field treatment facility, regional and state logistics support, and community alternate care site support.
As the leading health care provider in eastern North Carolina, ECU Health supports EHPC’s mission, in close partnership with other regional and statewide emergency response partners. These partnerships are essential to helping ensure communities across the East have access to high-quality resources and health care, particularly in the event of a disaster situation.
“I feel this exercise was crucial for our disaster preparedness and response,” said Nat Gladding, manager of Hospital Operations at ECU Health Beaufort Hospital. “It helped us assess our readiness, opportunities, and improve coordination between emergency response agencies. The exercise simulated a real-life scenario, allowing agencies the opportunity to practice their regional response to a disaster of this nature. Participation in disaster drills and exercises promote enhancement of our response for the communities of eastern North Carolina.”
In the years following the onset of the COVID-19 pandemic, health care as a whole has fundamentally changed — as have the lives, habits and health care needs of communities across the country.
Today, emergency departments (EDs) everywhere are seeing high volumes while staffing shortages persist. In rural areas with communities that are sicker than many others, these challenges are even more magnified.
“I’ve got patients who can’t see a doctor in the community mixed in with patients who have a pulmonary embolism,” said Dr. Leigh Patterson, chief of services for Emergency Medicine at ECU Health Medical Center and chair of Emergency Medicine at Brody School of Medicine at East Carolina University. “My team and I are trying to see the forest through the trees. Who’s the patient that needs the services? Everyone needs the services, but who’s the patient that medically needs the services next? And that’s hard.”

Meeting the challenge
At ECU Health Medical Center and throughout ECU Health system hospitals, leadership teams have needed to adapt quickly to meet the needs of the many patients seen through EDs.
Alex Baylis, ED nurse manager at ECU Health Medical Center, said she has been proud to see the department’s flexibility and persistence while helping patients through their time in the ED.
“We have flexed and bended, added and changed our spaces, we’ve changed our beds, we’ve changed our staffing patterns, we’ve changed our hours of when team members come in, when team members go home. We’re doing all that we know to do, and have the power to do, to get care to our patients faster and better,” Baylis said. “Right now, we’re facing really difficult barriers and obstacles within our space that are challenging, but we’re doing everything that we can and know to do to help our patients.”
Dr. Patterson echoed Baylis’ sentiment.
“We’ve tried, we are going to continue to try and it isn’t going to look the way it used to look,” Dr. Patterson said. “I think patients have been very understanding when we’ve had to do things in a different way. It is a really ugly reality right now, but we’re going to flex a lot. What I really want people to understand is what you see in the ED is actually all of the hospitals and all of health care right now.”
Matter of perspective
Dr. Patterson said she has seen a great deal of change in eastern North Carolina since she first came to the Brody School of Medicine and ECU Health Medical Center 17 years ago.
When she arrived at what is now ECU Health Medical Center, she became just the fifth female emergency medicine clinician. Today, she said, there are more females than that in the intern class alone.
“I am not the generation that was the first and only,” Dr. Patterson said. “I had other female residents who were with me. We were definitely the minority, but we’re not such a minority today.”
Dr. Patterson estimated there to be about a 50/50 male to female split among emergency medicine training program graduates across the country today and more women are holding education leadership positions.

However, that same shift has been slower to develop on the administrative leadership side.
“It takes some time to get all the way up the ranks so there are probably a dozen women chairs in academic medicine and emergency medicine and other positions like mine,” Dr. Patterson said. “But really, not a large number of us when you consider there are a couple hundred of our programs.”
From an outsider’s perspective, the number of female leaders in the ED may seem unique, but to those on the floor, it’s nothing to bat an eye at.
“We’re kind of past that – ‘Look, that’s so cool.’ Some days we’re still there,” Dr. Patterson said. “A lot of days it’s like, ‘Oh, yeah.’ I mean, I don’t think our nurses notice. We could go 24 hours in one area and it’s all women physicians and it’s just like that’s Tuesday. We don’t stop and notice that.”
Baylis noted that from the nursing perspective, more males in nursing tend to gravitate toward EDs and Intensive Care Units, but on the leadership side it is predominantly females.
Dr. Patterson reflected on the early part of her career and how conversations have shifted and become more normalized. Whether it’s the way patients address female providers or the interactions teams have with each other, she has seen positive change.
“I have men, physicians now who can have open discussions about, ‘Hey, how are you taking your FMLA leave when you have a baby? Are you splitting it, are you taking it at the end?’ The normalization of those conversations, that’s what comes from it,” Dr. Patterson said. “We’re not there all the way, we still have a long way to go. But it was not this normal in my first job.”
Providing compassionate care in trying times
As the care needs in EDs have changed, Baylis and Dr. Patterson noted how crucial it is to connect with patients on a human level and provide high-quality, compassionate care in stressful situations.
Baylis said the mindset of nurses in the ED has changed drastically in the past few years.
“In emergency nursing, you had to have tough skin and be almost hard,” Baylis said. “I think it’s changed with the population that we’re seeing in our patients, but also the care that we’re giving. We’ve learned to be more soft and more caring and taking that time to make a connection. We can be nice while still setting boundaries with our patients.”

Dr. Patterson said providing care in eastern North Carolina is a very unique situation. She shared that she trained at a county hospital in New Orleans and that in large, urban environments, it’s less common that she or her family members would be patients at the same hospital at which she practices.
Here, there is no line.
“So much of what I saw when I was in my own training, in my mind, I could pretend it wasn’t going to happen to me and you get this lovely distance that you don’t have here. And that’s good for you but, wow, some days it’s really hard,” Dr. Patterson said. “This is the same hospital you go to, right? I had my baby here. My husband has been a patient in our ED. My dad has been admitted here. I think this place is really challenging for that because it’s your community, you know, there’s no separation here.”
Baylis and Dr. Patterson said while that challenge exists, they are proud to serve in the same community they call home. What’s not lost on either of them: that solutions they are working to find in support of the communities they serve also directly impact their own family and friends — and light the path for ED teams to follow.
Resources
Frostbite isn’t the only concern with the frigid temperatures expected in eastern North Carolina this weekend.
“You can’t smell it. You can’t see it. You can’t taste it,” said ECU Health Chief for the Division of Medical Toxicology Dr. Jason Hack
Dr. Hack said carbon monoxide poisoning can sicken people when their furnaces malfunction or they use other means to heat their homes.

He said that includes, “HVAC, our heaters in our home. Portable heaters, propane portable heaters that some people might bring in, or if they lose their electricity because of an ice storm or something along those lines, they might want to bring in a generator out of the storm or close to the home.”
Dr. Hack also said people should never sit in a running car to escape the cold if the heat is out at their home.
“Some people would tend to sit in their car and turn on turn on their vehicle while it’s still in their attached garage,” he said, “Even with the door open, these can be sources of enough carbon monoxide to injure or even, unfortunately, kill people within the home itself.”
It’s not a good idea, but a dangerous one, to use the gas stove in your kitchen to warm up the house. Dr. Hack said, “It could be producing low levels of carbon monoxide that might accumulate.”
And the symptoms of carbon monoxide poisoning can be non-specific.
“It can look like a lot of other things,” he said, “Such as weakness or dizziness. Some people complain of some shortness of breath. Headache is one of the most common presenting symptoms of carbon monoxide. Confusion. Some people actually complain of chest pain or palpitations and fainting.”
Dr. Hack said the best defense is a working carbon monoxide detector in every bedroom and living space in the house; he recommends that people to make sure the batteries are fresh and they’re working properly before the cold air arrives this weekend.
According to the National Institutes of Health, about 1,200 people die in the U.S. from accidental CO poisoning annually and more than 100,000 people visit the emergency department each year.
