ECU Health recently hosted the Provider Patient Choice Awards at a luncheon honoring more than 200 ECU Health providers.
The Provider Patient Choice Awards recognize ECU Health providers who rank in the top 10% in the nation in the Watson Human Caring[1] question for “Creating a caring environment that helped me heal.”
Attendees, both in-person and virtual, heard from ECU Health leadership as they thanked the winners for their work and discussed how compassionate care impacts patients, families and the health system. ECU Health CEO and Dean of the Brody School of Medicine at East Carolina University Dr. Michael Waldrum said there is no greater honor than being recognized by the patients and community members a provider serves.
“We teach medical students and nurses about all of the technicalities and the hard work that it takes to take care of other humans,” Dr. Waldrum said. “However, one of the most important elements of excellence in providing health care is connecting with other people and caring. We know the data is very clear, it’s been shown many times that the better connection you have with that patient, the better they do. They’ll take their medications, they’ll follow your advice and their outcomes are better.”
He also noted that with expanding technologies and societal changes, the connection aspect in health care is needed now as much as ever and acknowledged a shift toward even more compassionate care in recent years. He expressed deep gratitude for the care teams making caring environments for patient and their families a priority.
Dr. Jason Foltz, chief medical officer with ECU Health Physicians, shared that the morning of the event, he had multiple visits with patients who did not have medical needs, but just needed someone to talk to about anxieties around medications or upcoming procedures. He said these interactions with patients and families are just as important, if not more important, than the medical care he provides.
“These are our patients and what they need is what you all provide them, which is a listening ear and the fact that you choose to care,” Dr. Foltz said. “At the heart of all this, everything we do—we’re just people serving people. That’s what today is about, to recognize and highlight that amazing spirit you bring and what really makes ECU Health, ECU Health.”
Dr. James Powell, a Patient Choice Award recipient, agreed with Dr. Foltz about the heart of a provider’s work. He said his team makes all the difference by starting each visit with a warm smile and a helping hand for patients.
He said he was excited to share the award with his team and recognize them for going above and beyond and developing positive patient relationships, which he uses for the foundation of each visit.
“We’ve been truly blessed, because we have a wonderful head nurse who has really created a good vibe among the staff as they go through day-to-day work. I’m sure a lot of you feel the same way about your staff,” Dr. Powell said. “When patients are calling, they’re calling because they need something. The something that they get is an answer to that question but a lot of times, it’s also just something that helps to calm them down and to make them feel good about things. I think that we’d really be remiss on a day like today if we didn’t think about the staff with whom we work, who really allow us to do what we do every day.”
ECU Health Chief Experience Officer Dr. Julie Kennedy Oehlert served as Master of Ceremonies for the event and encouraged providers to take their award boxes – filled with a plaque, stickers, star pins and more – and share them with their teams who support them every day.
She said during the event that the awards are truly special because they come from the patients these providers serve.
“The patients really showed us that you create a caring environment,” Dr. Oehlert said. “As much as you love them, they love you right back. We just want to thank you all for everything you do every day and recognize that the patients think you are amazing.”
About ECU Health Patient Choice Awards
Established in 2023, Patient Choice Awards recognize and honor ECU Health team members and providers for their dedication, effort and support to eastern North Carolina and the patients and families ECU Health serves. Winning teams and providers are chosen based upon commentary and feedback collected from patient surveys. Recognition events are held throughout the system in the fall and winter to showcase the people and teams who go above and beyond in support of our mission to improve the health and well-being of eastern North Carolina.
More Reading
Teams across ECU Health recognized by patients with Patient Choice Awards
[1] Jean Watson’s Theory of Human Caring is a foundation of patient care and focuses on the importance of the interpersonal relationship between a caregiver and care receiver. The theory states that this relationship helps not only the person receiving care, but the caregiver as well.

Zach Martin served as a North Carolina state trooper, and after dealing with pain in his leg that began in August of 2022, he went to the doctor to find out what was going on. “The doctors did several rounds of steroid injections, but by December of 2022, he couldn’t walk and they did more tests,” said Ginny Martin, Zach’s wife. “It showed a large tumor in his left femur.”
Zach was diagnosed with Ewing sarcoma, a rare bone or soft tissue cancer that primarily affects children and young adults. Zach was 33 at the time of his diagnosis, and his cancer progressed rapidly. “You think someone our age shouldn’t get cancer,” Ginny said of Zach’s illness. “He had his whole career ahead of him. He should have watched our kids grow up. Sometimes life isn’t fair, but he gave it one heck of a fight.”
On Feb. 10, 2024, just after his 35th birthday, Zach Martin passed away at the Service League of Greenville Inpatient Hospice, an ECU Health hospice house with eight beds, private rooms, a health garden and a chapel/meditation room. “From the moment we walked in the door, they treated us like they’d treat their own family,” Ginny said.
A difficult road
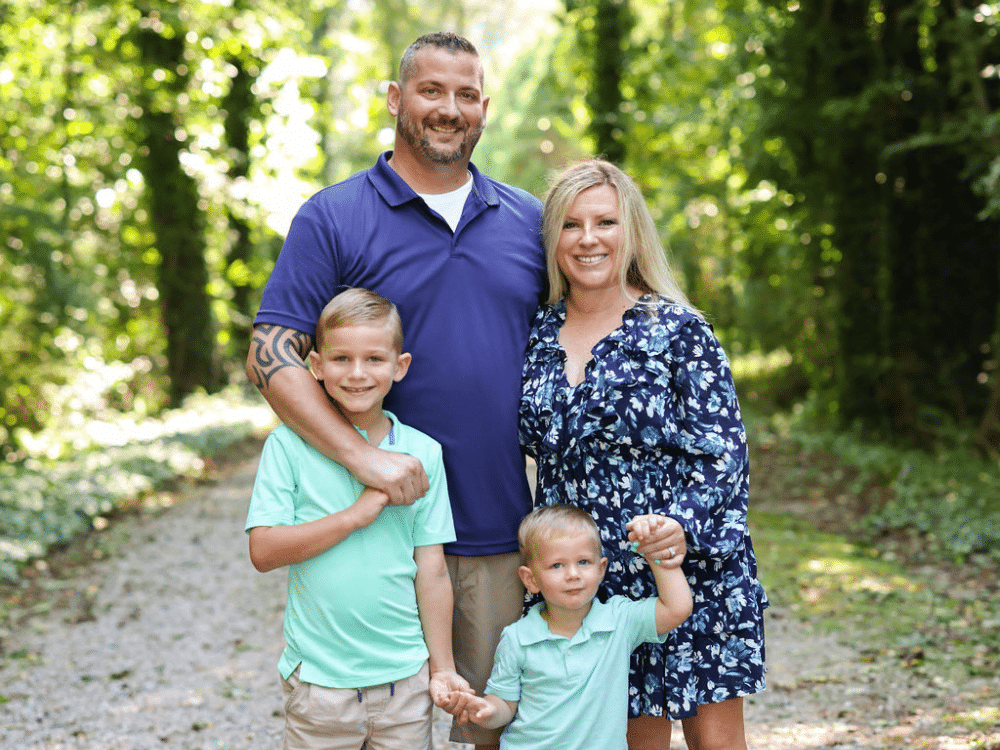
Zach was a High Point, North Carolina native, and he and Ginny met when he moved to Belhaven to work in law enforcement. “Zach was a jokester, and he never met a stranger,” Ginny recalled. “He was always making people laugh.” They married in 2014 and had their first son, Greyson, in 2015. Their second son, Lawson, was born 6 years later.
After Zach’s surprising diagnosis, he began chemotherapy as soon as possible. Yet, his recovery wasn’t easy. At one point, he rolled over in bed and snapped his femur; he required surgery to replace 40 percent of the bone with a titanium rod. He was in the hospital for 10 days, and after returning home, he went through intense physical therapy from January to May of 2023. “He had to learn to walk again, and all during this time he was having chemo,” Ginny said. This was followed by radiation, during which time the family temporarily relocated to High Point so Zach’s family could help watch the boys. In August, Zach completed radiation, but later that month, scans showed the cancer was back and spreading rapidly. He began another type of chemotherapy, but he didn’t react well to it. “Between October and December, we were in the emergency department at least four times a month because of his pain,” Ginny shared.
Just before Christmas, Zach was in a great deal of pain, but no medication helped. He was admitted to the hospital on Jan. 2 in the hopes they could control his pain and to administer inpatient chemotherapy, but he again didn’t respond well to the treatment. “He had neurological toxicity, where he slept for days, didn’t eat or drink and didn’t know me or his mother or our kids,” Ginny said. “They started talking about hospice then, but thankfully he came out of it.”
Zach was able to go home on Jan. 20, but after a week at home, he was readmitted to the hospital for uncontrolled pain. “We knew at that point that his cancer was spreading like wildfire. He started having blurry vision, so we asked for a scan of his head and brain to be done, and the scan revealed that the cancer had spread to the lining of his brain. At that point, there was nothing they could do, and they suggested we discharge to hospice,” Ginny said.
Ginny said she knew there was the option to have in-home hospice, but she had been Zach’s caregiver for the past 18 months and she didn’t want her kids to see their dad so sick at home. “I told Zach I would rather we go to an inpatient hospice with nursing care 24/7 so I could be his wife for his remaining time.”
A home away from home
Zach was brought to the ECU Health inpatient hospice house via ambulance, accompanied by an escort of state troopers. “The first person I met when we arrived was the chaplain,” Ginny recalled. “And Dr. Clifton was his doctor. I can’t say enough great things about the hospice house.”
Marilyn Davis-Okubudike, the bereavement coordinator at the inpatient hospice house, recalled meeting Ginny for the first time. “I met her at the door, and when she came in, I had my arms out and hugged her,” Marilyn said. “I felt her need and the connection. There were others there for Zach, but I wanted her to know we were also there for her. I took a special interest in her and the children, as well as Zach’s mother.”
Marilyn said doing this sort of work is a calling, and not one that everyone can do. “It’s a beautiful service to take care of people. I feel rewarded by this experience because it’s all for the patients and their families. We’re called to care for each other.”
Dr. Margaret Clifton is the hospice medical director, and she also feels a close connection to the patients and families she serves. “It can be really emotionally challenging, but it’s meaningful work,” she said. “I enjoy getting to know the patients and their families. For me, there is a lot of meaning in making death a little less awful. If I can do that, I feel like I’m making the world a little softer.”
Ginny remembers Dr. Clifton – and all of the hospice staff – as being very supportive. “They listened and were nurturing through the whole thing,” she said. “If we didn’t understand something, they explained it. I got to bring the kids there, and his state trooper friends came to visit. The night he took his last breath, I came down the hall crying and Dr. Clifton was crying too. They all cried with us. One nurse came in on her day off just to be with us. You don’t find people like that – they are angels on earth.”
“Zach’s time at the hospice house will be something I carry around forever,” Dr. Clifton shared. “The thing that stands out is the community involvement. When he arrived here, he was escorted by the highway patrol. They shut down the road and there was a firetruck with a flag and highway patrol cars lining the ambulance bay. There were always officers here to visit, and they even brought his patrol car and parked it outside his room so he could see it. And when he died, they escorted his body to the funeral home in Washington, and there’s a picture of his oldest son with all of the highway patrol saluting Zach’s casket.”
After his passing, the Memory Bear program made bears not only for Zach’s boys, but also his mother, brother and sister. “They made the bears from his uniforms because I wanted the boys to have bears with the actual uniforms he wore,” Ginny said. “They were very accommodating as to what I wanted.” She also wanted a recording of Zach’s voice, but when they realized he was unable to speak, Dr. Clifton suggested they record his heartbeat instead. “Now it’s something sitting on the boys’ shelf that they can have forever, and they can press that bear and hear their dad’s heartbeat,” Ginny said.
While Zach and his family were at the inpatient hospice house for just six days, their experience was memorable. That’s because it’s like a home away from home, said Marilyn, a place where every team member works to meet the needs of the patients and their families. “A lot of people haven’t heard of us, but this is one of the best things ECU Health can offer the community and the 29 counties we serve. We need people to see what a beautiful jewel this place is.”
Resources
ECU Health Home Health & Hospice

It’s been a year since the state of North Carolina passed Medicaid Expansion, bringing with it much-needed coverage and financial reprieve for the communities ECU Health serves.
North Carolina’s former governor, Roy Cooper says “One year of Medicaid expansion in North Carolina,” said Dr. Michael Waldrum, ECU Health CEO and Brody School of Medicine’s dean. “As we celebrate this moment. We’re proud to say we’re building the national model for rural health care right here in eastern North Carolina.”
That model depends on Medicaid Expansion and affordable access to care.
“It is a comprehensive health benefit where you can go see a primary care provider, have it covered,” said Kody Kinsley, secretary of the North Carolina Department of Health and Human Services. “Where you can have pharmacy, vision and dental and a copay that is never more than four dollars.”
Cost-effective health care is an important component, but it’s not the only one. ECU Health’s Dr. Karen Coward states “This is the power of Medicaid expansion. It’s not just about providing coverage, it’s about dignity.”
And peace of mind for the patients who need it most. Medicaid Expansion beneficiary and ECU Health patient, Darcy Guill spoke during the event.
“Sixteen years ago, I found myself unable to work and I lost my health insurance,” Guill said. “For the next 15 years, I was either uninsured or under insured.”
Her inconsistent coverage hit home in a different way following a car accident.
“I was hospitalized for two months right here at ECU Health,” Guill said. “I knew I was going to be uninsured again and I didn’t know what to do and I was terrified.”
That panic subsided when she realized share now had another option.
“It didn’t dawn on me at first that it was going to include me but it did,” she said. “Medicaid is literally saving my life. I am the person that benefitted from it and I am no different than all the other people that could benefit.”
In recognition of the one-year anniversary of Medicaid expansion in North Carolina, Gov. Roy Cooper visited ECU Health Medical Center in Greenville to reflect on the impact of expansion and celebrate a year of reaching North Carolinians in need.
Since Medicaid expansion officially launched in North Carolina on Dec. 1, 2023, more than 80,000 eastern North Carolinians and nearly 600,000 people statewide have benefited from access to vital health insurance. Along with Medicaid expansion, the state also passed the Healthcare Access and Stabilization Program (HASP), which provides critical relief to rural hospitals.
Gov. Cooper said Medicaid expansion’s reach in rural communities, like ECU Health’s 29-county service area, has been especially impactful in the last year.
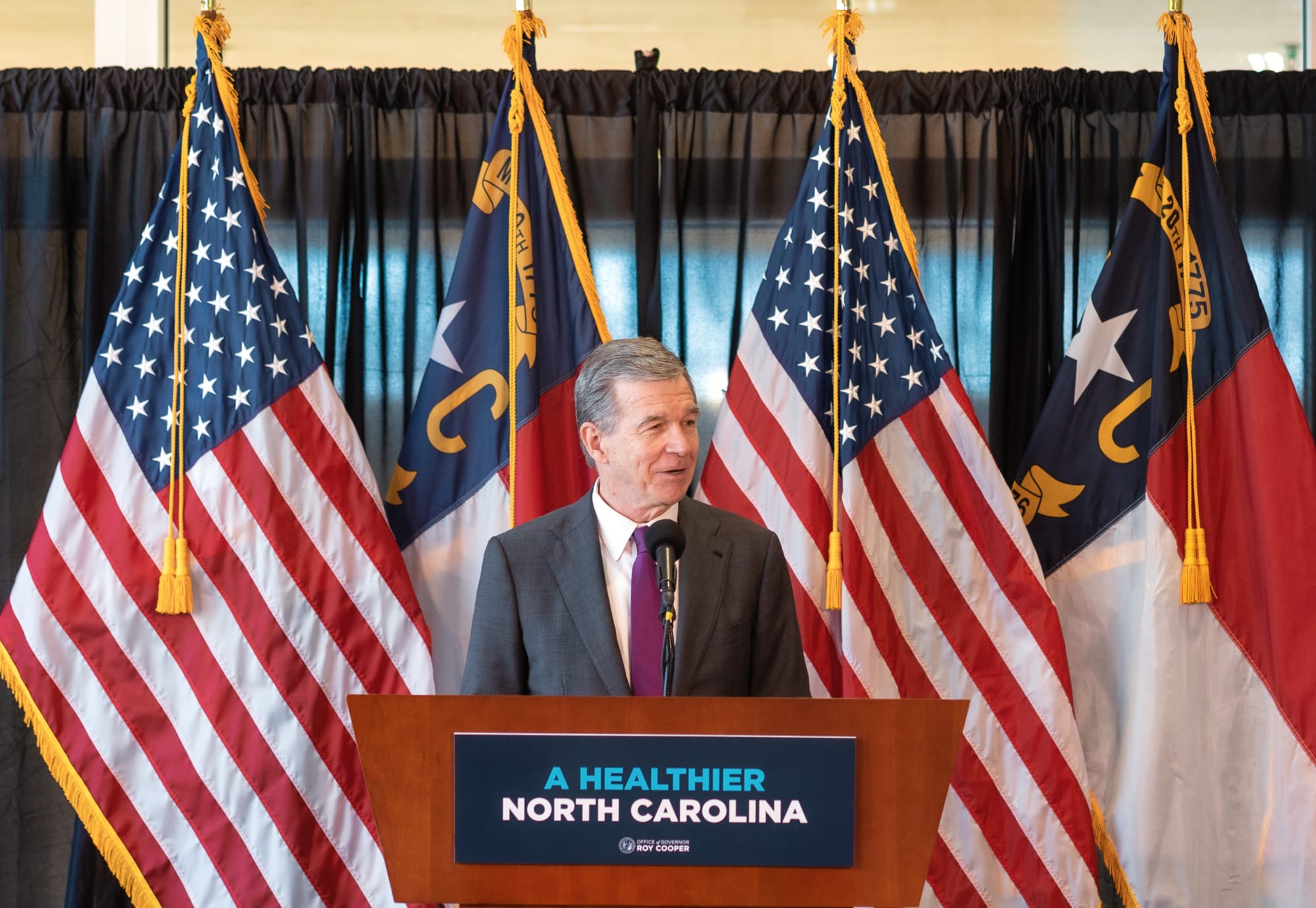
“The last year showed us that this is something that people desperately needed, particularly here in rural North Carolina,” Gov. Cooper said. “I grew up in Nashville and we know that rural North Carolinians have been helped more by Medicaid expansion than anyone else. I hold close to my heart the mission of getting people healthier. I knew getting Medicaid expansion passed and signed into law was the most important thing we could do to accomplish that.”

This milestone reflects the culmination of more than six years of advocacy by ECU Health, driven by the challenges faced by uninsured and underinsured patients.
Dr. Michael Waldrum, ECU Health chief executive officer and dean of the Brody School of Medicine at East Carolina University, said Medicaid expansion and HASP funding is creating real differences for patients, health care workers and the future of health care in places like eastern North Carolina.
“Medicaid expansion has helped improve access to primary care, empowering people to take control of their health and their lives,” Dr. Waldrum said. “It is also an investment in rural health organizations like ours. At the same time and in partnership with the state, ECU Health and the Brody School of Medicine are also committed to doing their part to support primary care expansion efforts in rural health care.”
He highlighted the expansion of the Rural Family Medicine Residency program, which will train nine rural residents per class across three training sites in the East and the upcoming Center for Medical Education Building on Brody’s campus. This investment has helped and will continue to help ECU Health and Brody serve the combined mission of improving the health and well-being of eastern North Carolina.
Dr. Karen Coward, a family medicine physician with ECU Health, is a Kinston native and practices in Tarboro. She said she knew by age 10 she wanted to be a family physician in her home community. She attended Brody and stayed true to her dream of serving eastern North Carolina.
She said before Medicaid expansion, many of her patients would rely on the emergency department for care. Even if a patient was connected with primary care, it was difficult for them to follow through with appointments or afford medications. Chronic conditions like diabetes, hypertension or even cancer would go unchecked. Now, she said, she’s seen a life-changing shift.
“Patients who once cycled through the emergency department are now establishing relationships with primary care providers like me,” Dr. Coward said. “They are keeping their appointments, following through on recommendations, treatments, and gaining access to medications and specialist referrals that were previously out of reach. For many, this will mean earlier diagnoses and interventions, reducing the burden of advanced diseases.”
Kody Kinsley, secretary of the North Carolina Department of Health and Human Services, joined the event and said that in the past year over $58 million in dental claims alone were filed, millions of prescriptions were filled and hundreds of millions of dollars in claims supporting hospital care were taken care of through Medicaid expansion.
He said this comprehensive health insurance is already making a real difference for individuals and families.
“Medicaid expansion is life changing for families,” Sec. Kinsley said. “It is peace of mind for people as they sit up late at night thinking about how the next day will impact them. Will a sickness impact their family? Will they end up in debt? They don’t have to worry about that anymore.”

The event also included remarks from a Medicaid expansion beneficiary, Darcy Guill from Ayden, who shared her gratefulness for regular care she’s receiving, specialists she’s able to visit and prescriptions she can fill, thanks to Medicaid expansion.
As we look back over the previous year, we’re proud to build the national model for rural health care here in eastern North Carolina at ECU Health and we’re grateful for the support the region and health system through Medicaid expansion and HASP.
Greenville, N.C. – Trish Baise, ECU Health chief nursing executive, was recently honored as one of Becker’s Hospital Review’s 2024 Chief Nursing Officers (CNOs) to know. Since stepping into the role in 2022, Baise has cultivated a dynamic nursing environment that drives innovations to enhance patient care quality and elevate patient experiences across eastern North Carolina.
“This recognition by Becker’s reflects the collective efforts of the incredible nurses across ECU Health, all of whom are dedicated to creating an environment where nurses and patients alike can thrive,” said Baise. “Together, we are driving innovative approaches in rural health care, committed to excellence in all we do and enhancing patient care across eastern North Carolina. I am honored that ECU Health has been recognized for this commitment.”
Tasked with addressing nurse staffing shortages, managing budgets and fostering growth opportunities for emerging nurses, the nursing leaders recognized by Becker’s play a crucial role in shaping the future of nursing.

Beyond leading nursing departments, CNOs drive innovative initiatives that uphold high patient care standards. Their roles demand a unique blend of clinical expertise and executive leadership. This list honors CNOs for their commitment to optimizing health care.
Baise has led efforts to establish a supportive environment where both nurses and patients can thrive. Under her leadership, ECU Health has achieved its third Magnet recognition, underscoring a commitment to nursing excellence. The Advancing Nursing Practice and Excellence (APEX) initiative has been foundational to this strategy, focusing on innovation, research and collaborative efforts to advance nursing in rural health care. Through partnerships with East Carolina University and local colleges, ECU Health also invests in the future of nursing, offering residency programs to equip new nurses with essential skills. This vision represents ECU Health’s dedication to defining a new standard for patient care and nursing excellence in eastern North Carolina.
“As the region’s largest health care provider and educator, ECU Health has a unique role in shaping community health, and Trish understands that our mission’s success depends on attracting the best providers, nurses and care teams to our health system,” said Dr. Michael Waldrum, CEO of ECU Health and Dean of the Brody School of Medicine at East Carolina University. “Trish’s dedication to service and our mission aligns with ECU Health’s work to build the model for rural academic health care. ECU Health is proud to lead the way in defining the future of nursing in our region.”
Resources
Amy Campbell, PhD, RN, CPHQ, LSSBB, quality nurse specialist III, represented ECU Health on Sept. 25 at a side event held in parallel to the 79th session of the United Nations (UN) General Assembly in New York City. The meeting, titled “2030 Global Agenda for Sepsis for Attaining Sustainable Development Goals,” was convened as a collaborative effort of the Global Sepsis Alliance (GSA), Medical Women’s International Association, Sepsis Stiftung and UNITE Parliamentarians Network for Global Health.
The meeting was the first-ever global strategy spearheaded by the GSA, with collaboration from 70 partner and member organizations from Regional Sepsis Alliances across Africa, Asia-Pacific, the Caribbean, eastern Mediterranean, Europe, Latin America and North America. The meeting’s objectives were:
- To present the 2030 Global Agenda for Sepsis as the first multi-year global strategy to alleviate the significant human, societal, economic and health care burden of Sepsis.
- To reach consensus on the urgent need for reinvigorating the Sepsis responses at global, regional and national levels for the attainment of 2030 SDGs including the aspirations for Universal Health Care, Maternal, Neonatal and Child Health, AMR, Pandemic PPR, Gender Equality, Peace and Partnerships for Development.
- To discuss the critical role of health care workers, especially the medical women, representing over 70% of the health workforce globally, in the promotion and implementation of the 2030 Global Agenda for Sepsis.
- To call for establishment of a High-Level Political Platform for Sepsis to lead integration of this global health threat into the mainstream of health and development dialogue and architecture, including G7 and G20 Summits, World Health Assemblies, UN General Assemblies, and World Economic Forums.
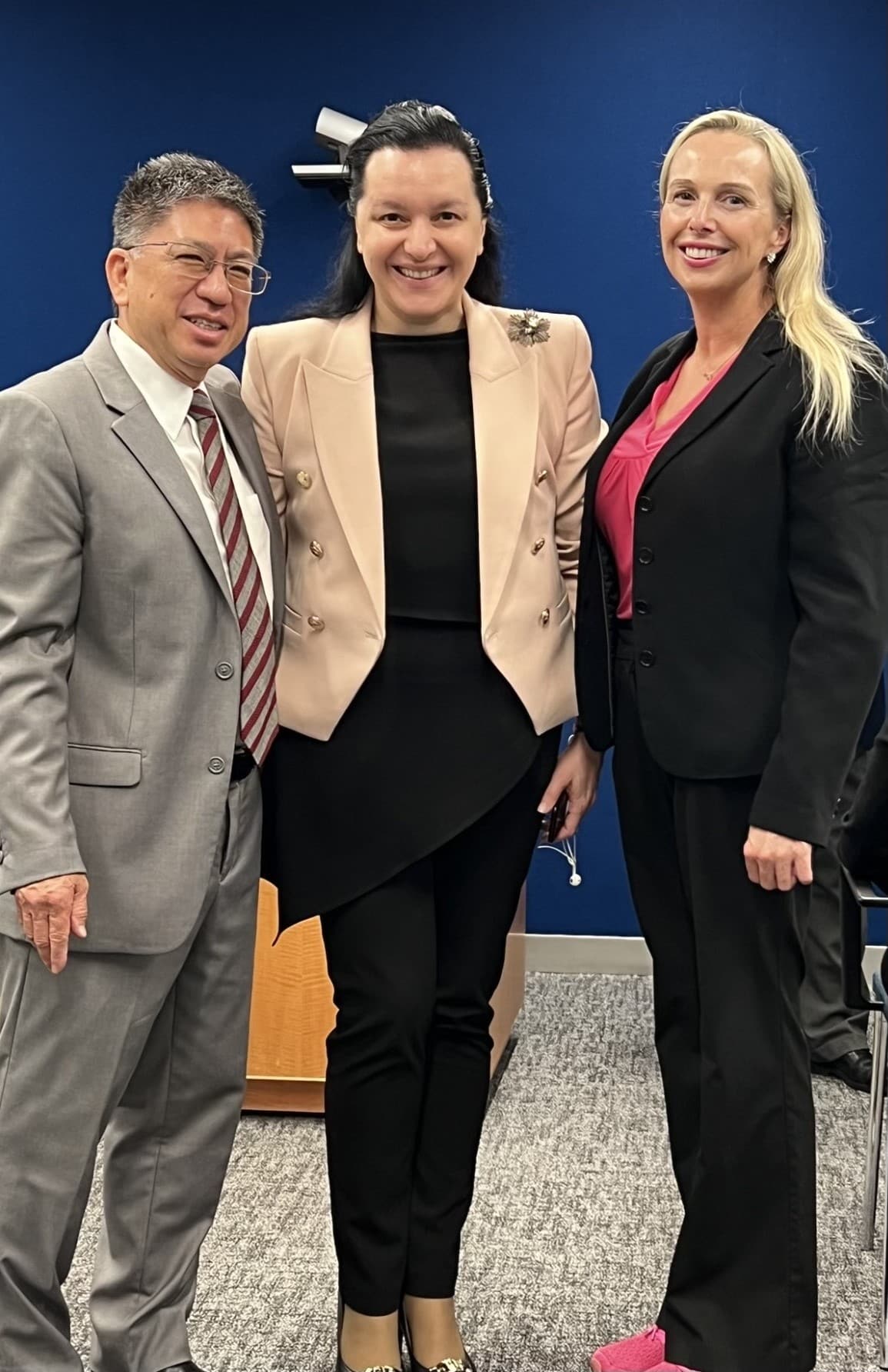
Dr. Campbell was personally invited to attend and speak by Dr. Mariam Jashi, MD, MPH, MPA and the CEO of the Global Sepsis Alliance, and Michael Wong, founder and executive director of the physician-patient alliance for health and safety. This invitation came as a follow-up to the 2024 World Sepsis Congress held this past April, during which Campbell served on the Scientific Committee. “I saw the invite and initially blew it off,” Dr. Campbell laughed. “I wasn’t sure it was real.” But after reassurance the invitation was legitimate, and with the encouragement of her team and Michael Wong, Dr. Campbell decided to go to New York. “I had a training session scheduled at work, but my colleagues covered for me,” she said. “I’m so thankful to my team and leaders who made it so I could attend.”
Once she arrived at the New York University campus, where the parallel session was held, Dr. Campbell said she met many leaders from across the world. “I met Dr. Eleanor Nwadinobi, the president of the Medical Women’s International Association (MWIA), Thomas Heymann, the president and CEO of the Sepsis Alliance and the Honorable Dr. Ricardo Baptista Leite, a member of the Portugese Parliament. People were speaking all these different languages and here I was from eastern North Carolina.”
The meeting focused on early detection of sepsis and how to treat patients with sepsis, no matter where they live. “As one of the speakers, I had the opportunity to emphasize the urgency of early detection, the critical need for continued research and the importance of securing funding so that everyone, regardless of their geographic location, can receive the same standard of care and chance for survival,” Dr. Campbell said. The speakers also discussed what they anticipated to be the next big problem with sepsis: antibiotic resistance.
Dr. Campbell said it was a great opportunity to represent the work she and ECU Health are doing to address the global problem of sepsis. “The attendees were impressed with the work we’re doing. ECU Health is a big deal; we have incredible people and talent, and we deserve a seat at the table,” she said. And next year, she has a seat waiting for her. “I’ve been invited back to speak next year, and I’ll work more with the GSA,” she shared. “We all have a lot to learn and do. Sepsis transcends borders, affecting individuals of all ages, races and socioeconomic backgrounds. However, the most vulnerable populations – children, the elderly and those in low-resource settings – are disproportionately impacted. Sepsis doesn’t wait, and neither can we.”
Greenville, N.C. – ECU Health Medical Center has been nationally recognized as a national leader in patient experience for the second consecutive year, according PEP Health’s 2025 rankings. PEP Health evaluated more than 35 million online reviews from patients and their families in 2024, offering a real-time look at patient experiences across health care providers nationwide.
ECU Health Medical Center’s recognition was highlighted by top-5 national rankings in several categories including overall patient experience, communication & involvement and emotional support.
“At ECU Health, creating caring experiences for our patients and team members is at the core of our mission,” said Dr. Julie Kennedy Oehlert, chief experience officer at ECU Health. “Our definition of excellence is shaped by feedback from our patients and fostered by the compassion and dedication of our team. Being recognized nationally for our excellence in communication and emotional support is a rewarding acknowledgment of the safe, healing environments we strive to create. We are committed to continually listening and evolving to meet the needs of those we are honored to serve.”

PEP Health’s 2025 Rankings focus on hospitals with at least 750 staffed beds and at least 250 patient experience comments left online between Sept. 1, 2023, and Sept. 1, 2024. These comments, sourced from patients and their families on social media and review platforms, were analyzed against seven internationally recognized domains of patient-centered care: fast access, effective treatment, emotional support, communication & involvement, attention to physical and environmental needs, continuity of care, and billing and administration.
According to PEP Health, research has shown that enhancing patient experience is not only associated with improved care outcomes, but also strengthens financial performance, safety and health equity. Positive patient experiences directly impact CMS Star Ratings, which are closely tied to reimbursement rates and play a critical role in driving new patients and increasing patient retention. ECU Health’s commitment to delivering exceptional care in eastern North Carolina ensures that the most vulnerable populations in receive the support and attention they need.
“This recognition is a testament to the unwavering dedication of our team members who bring compassion and empathy to every patient interaction,” said Brian Floyd, chief operating officer, ECU Health. “Caring for patients during some of life’s most challenging moments is more than a job – it’s a calling. I am incredibly proud of the heart and commitment our team demonstrates every day. Earning this national recognition for patient experience reflects their hard work and the trust our patients place in us, and we will continue to prioritize compassionate, patient-centered care in all we do.”
ECU Health serves a vast rural region and understands the critical need for accessible health care in these communities. The demand for health services is exceptionally high, and many residents face significant barriers to receiving the care they need. ECU Health launched the Health Hub initiative in May 2023 as a strategic effort to bridge these gaps and help meet patients where they are. These Health Hubs are designed to improve access to vital health care and community resources, specifically targeting underserved areas.
“These hubs are strategically placed based on data indicating regions of high social vulnerability,” said Kasey Perkins, community health engagement coordinator, ECU Health. “Oftentimes, these areas have limited access to primary care services and individuals have difficulty seeing a doctor for those unexpected acute illnesses we all get.”
Health Hubs are currently located in four counties: Pitt, Martin, Edgecombe and Beaufort.
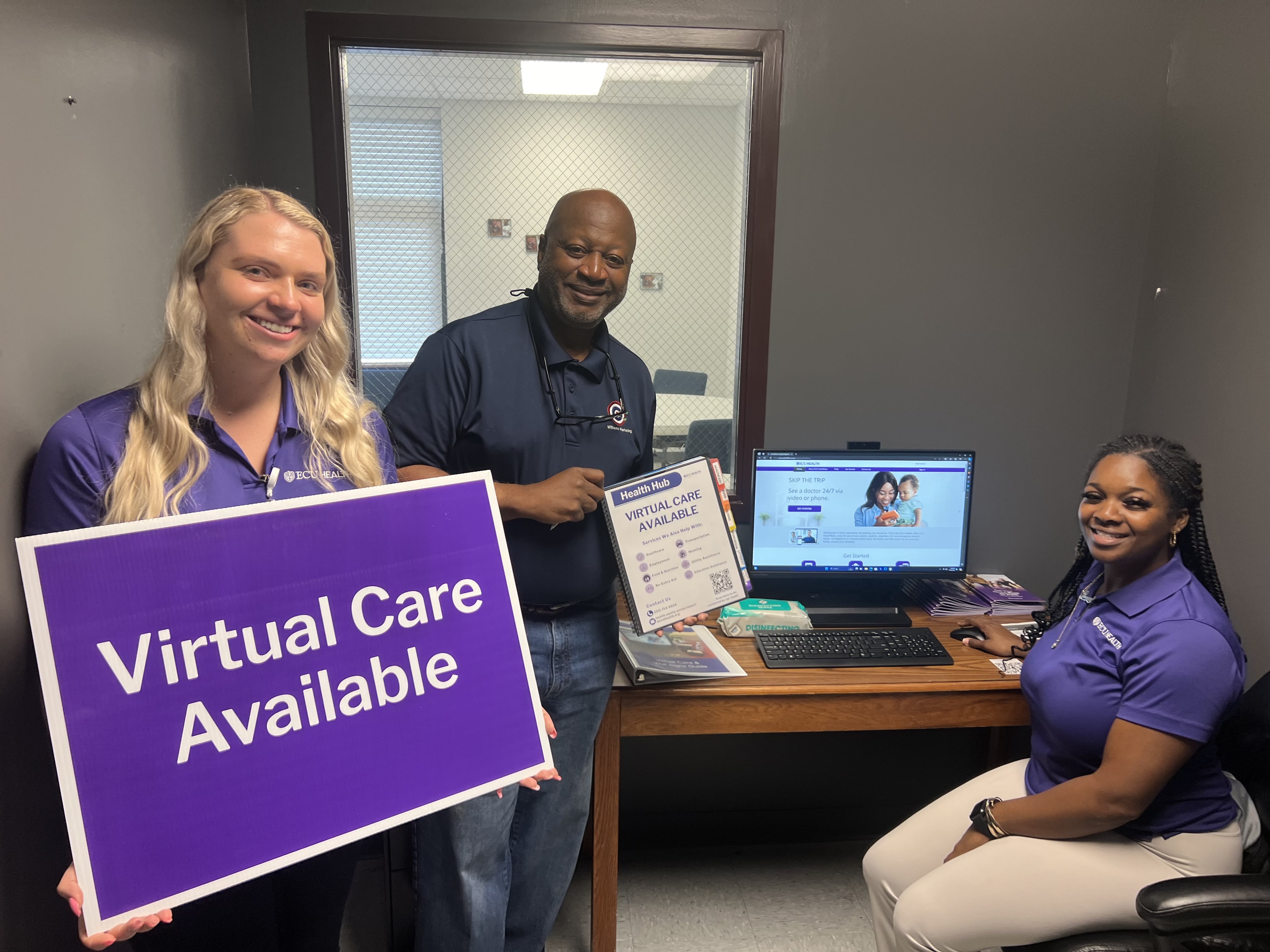
The hubs serve dual purposes. First, they provide access to virtual care, which is particularly vital in areas where individuals might otherwise visit emergency departments for non-urgent issues. By educating the community about virtual care options, Health Hubs help people get appropriate care quickly and more efficiently. Second, Health Hubs offer a gateway to community resources, addressing social determinants of health such as food insecurity, housing and employment.
“Each hub features a community resource guidebook, organized into tabs for different social needs, filled with contact information and details on various agencies and services available in the area,” said Perkins.
Health Hubs are located at local churches, businesses and organizations, and a designated Health Hub ambassador serves as the community’s point of contact. These ambassadors help residents connect with virtual care services and navigate the resources available to them. The hubs are equipped with necessary devices, including a computer with a webcam and microphone, and vital sign monitors like blood pressure cuffs, pulse oximeters and thermometers. This equipment allows individuals to have virtual visits on-site if they don’t have access to the technology at home.
Three new locations were added in July 2024, bringing the total amount of Health Hubs to 21. Health Hubs are open to everyone in the community. Residents can walk in during designated hours to learn more about virtual care or access community resources. The virtual care service, ECU Health Now, is available for anyone throughout eastern North Carolina and can be accessed on a computer or mobile phone. It is free to register and make an account, and it only costs $55 per visit when you speak with a provider, which is often less than a typical insurance co-pay or Emergency Department visit.
“The Health Hub initiative represents a significant step toward making health care more accessible and addressing broader social needs,” said Perkins. “By partnering with local organizations and connecting individuals with vital resources, Health Hubs are making a real difference in the communities they serve.”
As ECU Health continues in its journey toward leading positive changes in support of the health and well-being in the communities it proudly serves, its impact can be seen – and tasted – in the health system’s nine hospital cafeterias where Food and Nutrition team members create delicious and healthy food options for patients and visitors.
With a focus on plant-forward meals that support health, well-being and a healing experience, the Food and Nutrition team has been instrumental in ECU Health’s team member and community-focused Blue Zones initiatives, which recently won the North Carolina Hospital Association’s 2024 Highsmith Award for Innovation.
The four Blue Zones initiatives implemented by ECU Health include the Team Member Blue Zones Challenge, Plant-Forward Meals for patients and team members, Wellness Center Blue Zones, and targeted initiatives in Bertie, Chowan and Dare County. ECU Health is prioritizing the community and engaging in partnerships with local foodbanks and churches to spread the word of the initiative – and make sure the community knows that healthy, plant-forward food is not only nutrient-dense, but also delicious.

None of it would be possible without the expertise of the Food and Nutrition team. With nearly 300 Food and Nutrition team members helping prepare nearly three and a half million healthy and delicious meals at ECU Health locations across the region, this team is making healthy food accessible to patients, families and team members. On any given day, the ECU Health Food and Nutrition team prepares a menu inspired by international cuisines which heavily feature plant-based ingredients: Tandoori chicken, chipotle chicken tacos, sushi, to name just a few.
“It’s hard to describe how fortunate we are at ECU Health to have such an incredible Food and Nutrition team, which is truly at the heart of our work to encourage healthier lifestyles through the Blue Zones initiatives,” said ECU Health Chief Well-being Officer Dr. Christina Bowen. “Our team members and communities benefit from the amazing work they do. Their passion for creating meals that not only taste good, but are also good for you, is a critically important part of the positive change we are leading in eastern North Carolina.”
The summer break was no break for more than two dozen East Carolina University College of Nursing students who got to see what their post-graduation life could be like with a new student nurse extern program sponsored by ECU Health Medical Center in Greenville.
In the summer of 2023, shortly after an expansive academic-practice partnership agreement was signed between ECU Health and the College of Nursing, leaders from both organizations explored options to help expand the number of new graduates who could fill vacant nursing ranks across eastern North Carolina.
One of the initiatives the group quickly agreed on was an extern program: nursing students would be certified as nursing assistants and then work in a variety of care settings across the health system to gain practical experience before starting their final semesters of nursing school.

To be eligible for the extern program, student nurses would be required to complete Nurse Aide II certification, which all nursing students are eligible for, but not all take advantage of. Nurse Assistants are allowed to perform limited patient care activities as well as assist licensed health care workers with taking notes and uncomplicated wound care.
Dr. Jeanne Martin, chair of the baccalaureate nursing program, said the certification gave ECU Health leaders the confidence that the nursing students could “function within the scope of an NA II all the while learning the RN role with their preceptor.”
“During clinical experiences, students function under the licensure of their faculty and may administer meds or other skills not part of NA II certification,” Martin said.
While their practical role was limited, Martin stressed that the intangible skills the students learned – like how to comfort a patient and translate complex medical terminology and procedures to a patient’s families, was invaluable.
On July 9, the graduates of the first extern program gathered at the Monroe Center on the ECU Health campus to celebrate their accomplishments with their preceptors and the leaders who originated the program.
“I’m so grateful that you took this journey with us and congratulations. We appreciate the opportunity to partner with you on your professional journey,” Dr. Trish Baise, ECU Health’s chief nursing executive, said to the graduates during the ceremony. “Our goal is for you to be as prepared as you possibly can be as you transition into practice.”
Baise said she plans to expand and evolve the program so that more nursing students have an opportunity to gain valuable experience while still in school because nursing care is increasingly complicated and challenging.
Dr. Bim Akintade, dean of the College of Nursing, was an early proponent of the academic-practice partnership and said he is thrilled at the results the inaugural cohort of externs achieved during their eight-week experience.
“We are very thankful for ECU Health’s efforts to give our students a chance to learn some of the inner workings of their profession now, before they graduate. Once they are licensed and at the bedside, their nurse managers, and more importantly their patients, will rely on them to be ready on day one, and this experience puts them in an excellent position to be ready,” Akintade said.
Tracy Langston, ECU Health’s director of nursing professional development and innovation, was the medical center’s lead for the extern program and responsible for placing the students in their roles. She is most proud of the growth the student nurses achieved with developing their time management and communication skills.

“It’s been a phenomenal experience for our externs. They really increased their confidence as nurses, they are excited about the skills they were able to achieve and experience, and they’ll use that as they finish nursing school,” Langston said. “They spoke about how this program helped them work on their time management skills and prioritization as they prepare to hopefully join us as new graduate nurses after graduation.”
During the ceremony, students recounted their experiences during the extern program.
Blair Beaulieu, a nursing student from Greenville, said working alongside the family medicine team gave her insights into the working life of a nurse that she just couldn’t get from textbooks and classroom lectures.
“This program allowed me to explore the various opportunities and interdisciplinary communication, walking information down to the laboratory, transferring patients who needed higher acuity needs of various floors — just seeing those inner workings of a hospital,” Beaulieu said.
Kiley Fisher almost missed the graduation ceremony and was dressed in grey scrubs, rather than Pirate nurse purple, having raced over from the hospital after helping with a birth.
Fisher credits her experience with reinforcing foundational skills — like drawing blood and placing Foley catheters — which gave her space to work on critical thinking and communication with all members of the care team.
“I can now not freak out when a patient asks a question that I don’t know the answer to and how to continue to look professional while saying I don’t know, let me find out for you,” Fisher said. “It’s reaffirmed that nursing is where I’m meant to be.”
Emma Campbell, a nursing student who worked in the ambulatory clinics, found her footing, and her voice, while working directly with patients.
“I was challenged to develop my interprofessional communication, my confidence in my interactions with patients,” Campbell said. “Working with family medicine clinics, I was able to improve in these areas substantially.”

Kinsey Cook, one of the student nurses, said the extern program forced her to gain new levels of self-confidence, largely because she wasn’t given a choice.
“I was shy and nervous around other team members, but I gained confidence throughout this program by answering the phone and assessing the plan of care with doctors. I was able to talk to pathology, labs, pharmacy, nutrition services, and I got to see more than just the nursing aspect of patient care,” Cook said.
Cook spoke with pride at learning to believe in herself in the clinical role, as well as advocating for the patients she interacted with, a skill fostered by spending time with a charge nurse in the unit to which she was assigned.
Ankita Das said her experience working with palliative care teams helped her to develop a set of skills that can’t be learned in the classroom — one-on-one interactions with patients and the loved ones in the room with them.
“During this externship I realized I needed to further develop, and learn more about, comforting patients, family members and what to say when their loved ones passed,” Das said. “I observed the chaplains’ interactions with the families — they were empathetic and always offered to talk about memories with family. They lent a shoulder to cry on and a listening ear, this helped me learn what to do and what to say when a patient passes.”
The program’s success has given its leaders hope for future iterations, and opportunities to expand student participation in the future across the health system’s locations in eastern North Carolina.
“One of the reasons for implementing a student nurse extern program is that it’s an excellent recruitment and retention tool,” Langston said. “This is just the start. We are looking forward to continuing our student nurse extern program in 2025, so students — get ready to apply in December.”



