Leaving a child, senior or pet behind in a car can pose serious danger, even if it’s just for a few minutes.
That was the message of the hot car safety event hosted by Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center, along with the Pitt County Health Department and the Martin-Pitt Partnership for Children.
Walston said it’s dangerous for anyone to be left alone in a vehicle because of how quickly they can heat up, but especially for children.

“Children’s bodies heat three to five times more quickly than adults,” Walston said. “They all have a smaller amount of body surface so they can’t cool themselves very quickly. A small child, like the families we’re serving today, they can’t verbalize when they’re thirsty if they’re under a certain age. You really have to be very careful. The message is never leave a child alone in a car, not even for a minute.”
The team had a demonstration with temperature gauges and s’mores roasting in a vehicle on an 80-degree day, one of the coolest days in recent weeks in eastern North Carolina. Despite the cooler than normal temperatures, the interior of the van rose to 90 degrees within 15 minutes, over 100 degrees after an hour, and approached 120 degrees in an hour and a half.
The s’mores demonstration showed how quickly things can literally cook inside of a car when left alone.
“As you see we have this temperature gauge here and just in the last 15 minutes, it’s already gone up 10 degrees,” Walston said. “This is a white car with light interior, and with a dark car and dark interior it can heat the car more quickly.”
Walston noted that there have already been 10 deaths across the country this year from children left alone in cars. In North Carolina, we have seen one this year and another in neighboring Virginia.
She said more than 50 percent of child deaths from hot cars are from children that have been forgotten in vehicles. She said children can be forgotten when routines are broken and leaving something like keys, your cellphone or a briefcase in the backseat next to the child is a safe way to ensure the child is not left alone.
According to Walston, about 17 percent of hot car fatalities are children that are intentionally left behind. She said no amount of time is safe for a child to be left alone, even with windows cracked.
“Many times folks think that, I’m just going into the store for a few minutes, but anything could happen inside, you could become distracted and forget the child,” Walston said. “There is a misnomer that if you crack a window and that will offer some less heat, but that really is a myth. It doesn’t affect the temperature of the car.”
As a rural health care organization, we know there are many challenges to fostering a healthy community. That doesn’t stop ECU Health team members from finding creative solutions to bring health care outside the walls of our hospitals and clinics in eastern North Carolina and into the communities we serve.
KaSheta Jackson, DNP, RN, vice president of Health Equity and Social Impact at ECU Health, and her team developed Community Pop-Ups: A Rural Approach, an innovative health care delivery model implemented as community-based pop-up clinics across eastern North Carolina to address social and economic health care barriers.
This program makes health care both more accessible and approachable by directly providing preventative services, improving health care equity, and offering resources within communities with the greatest need.
Jackson was recognized earlier this year by the American Nurses Association (ANA) and the American Nurses Foundation (the Foundation) as the recipient of the 2022 ANA Innovation Award. The ANA Innovation Awards highlight, recognize and celebrate exemplary nurse-led innovations that improve patient safety and health outcomes. The innovation award also generated a $25,000 grant, which will fund future community health events.
Jackson said nurses are on the leading edge of connecting their fellow community members to health care and should feel empowered to innovate in that space.
“Our innovation has empowered many nurses to think and behave differently with regards to changing health care delivery and where care is delivered,” Jackson said. “By aligning the community and the health care system, we are addressing social, economic, equity, and population health, allowing us to meet our mission of improving the health and well-being of eastern North Carolina.”
Through partnerships with community leaders and other ECU Health team members, these clinics have evolved from solely offering health care screenings to providing COVID-19 testing, vaccinations, mental health resources, access to fresh produce and employment opportunities.
In 2021 alone, Community Pop-Ups provided care to more than 400 community members, identified acute diseases, provided numerous jobs, gave away 500 produce boxes, and delivered 500 health passports in rural locations across eastern North Carolina.
“We are following the model of doing health care on the outside to make health care better on the inside,” Jackson said during a July 2021 community health event in Farmville. “We’re working to address the social determinants of health, offering employment, trying to take care of the need for vaccines, taking health care into communities versus having people come to us – we’re taking services to those that need them.”
As these pop-up events evolve and grow, Jackson hopes they will help create a healthier eastern North Carolina, strengthen ties between community organizations and improve relationships between community members and health care providers.
“I am so excited to see our innovation become reality,” Jackson said. “The advice I would give to any nurse who wants to take their innovations from just an idea to action: be inquisitive, be nosey, ask questions, listen and it will be easy to make it happen.”
This is just one example of how Jackson and her team break down barriers to bring health care to the communities we serve. ECU Health also hosts a myriad of community events including: a foot clinic with Joy Soup Kitchen and Access East, which gives free foot care supplies to diabetic patients who visit the event, over-the-counter medication giveaways and Kids Eat Free with Sodexo, which provides free lunches and afternoon snacks for kids and teens up to age 18.
For more information, visit the Pop-Up Community Health Events page on our website.
GREENVILLE, N.C. – ECU Health and Acadia Healthcare announced today plans to build a state-of-the-art, 144-bed behavioral health hospital in the medical district of Greenville, N.C., less than a mile from ECU Health Medical Center. This new facility will be a center of excellence, providing North Carolinians with important access to behavioral health services and treatment from specialized clinical teams in a carefully designed environment.
Slated to open in spring 2025, the hospital will be operated through a joint venture between ECU Health and Acadia, the largest standalone provider of behavioral healthcare services across the United States. Together, the organizations will invest approximately $65 million in expanding behavioral health resources in eastern North Carolina.
![Perspective View 2 - NIGHT [no-logo] Conceptual rendering of new behavioral health hospital](https://www.ecuhealth.org/wp-content/uploads/2022/07/Perspective-View-2-NIGHT-no-logo.jpg)
The hospital will include 24 inpatient beds specifically for children and adolescents with mental health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
“This hospital will be a tremendous resource for our patients and our state, and we’re thrilled to bring a partner and a national leader like Acadia to eastern North Carolina,” said Dr. Michael Waldrum, chief executive officer of ECU Health and dean of the Brody School of Medicine at East Carolina University. “Acadia has an established track record of providing high-quality, compassionate care in communities across the country. Together, we will strengthen our level of expertise, implement proven best practices and enhance the quality and number of behavioral health services available to patients throughout the region.”
Prior to the pandemic, nearly one in five North Carolinians were experiencing a mental, behavioral or emotional disorder, according to a report from the North Carolina Institute of Medicine’s Task Force on Mental Health and Substance Use. In the last two years, national data indicates a growing trend of depression and anxiety symptoms. This partnership demonstrates a commitment to talking about mental health disorders, normalizing and treating them with the latest science and medicine in appropriate care settings.
“As a clinician, seeing this type of investment and understanding the significant impact it will have on patients is exciting,” said Dr. Syed A. Saeed, an ECU Health board-certified psychiatrist with more than 40 years of experience. “The needs of behavioral health patients differ from other patients and vary widely even within the same diagnosis. This state-of-the-art hospital will allow us to fully meet our patients’ unique needs in a safe, patient-centered environment and ensure clinicians have the resources and training needed to deliver excellent care.”
The new hospital will also serve as a teaching hospital, training students and residents from the Brody School of Medicine, many of whom will go on to practice in eastern North Carolina and carry forth ECU Health’s mission to improve the health and well-being of the region.
“We are always seeking like-minded partners who share our commitment to expanding access to high-quality behavioral health services and transforming the way mental health patients are seen and cared for,” said Chris Hunter, chief executive officer of Acadia Healthcare. “Establishing a center of excellence in partnership with ECU Health presents a unique opportunity for us to support the development of the next generation of behavioral health care workers and clinicians. We’re excited to begin this important work with such a committed, patient-focused partner.”
Construction is expected to begin in 2023, pending standard state and regulatory approvals and gaining a Certificate of Need. To facilitate the development of the new 144-bed behavioral health hospital, ECU Health will transfer 80 of its current behavioral health beds.
To learn more about the potential partnership between ECU Health and Acadia Healthcare, visit
ENCBehavioralHealth.org.
Find more information in our Press Kit.
With our continued focus on the imperatives of quality, experience and finance, ECU Health’s transplant program at ECU Health Medical Center has consolidated their treatment and office spaces into the newly renovated 3 South. The area is now known as the 3 South Transplant Clinic.
The transplant program performs an average of 80 to 100 living and deceased donor kidney and pancreas transplants per year. Patients that are seen in the clinic include pre-transplant (patients being evaluated for transplant), living donors and post-transplant. This program and the services offered have continued to grow over time, but have been limited by clinic space. To enhance patient and team member experience, the pre- and post-transplant clinics have now consolidated into one, centrally-designed space on 3 South, as they have been operating in separate clinics at the Cancer Center and ECU Physicians.
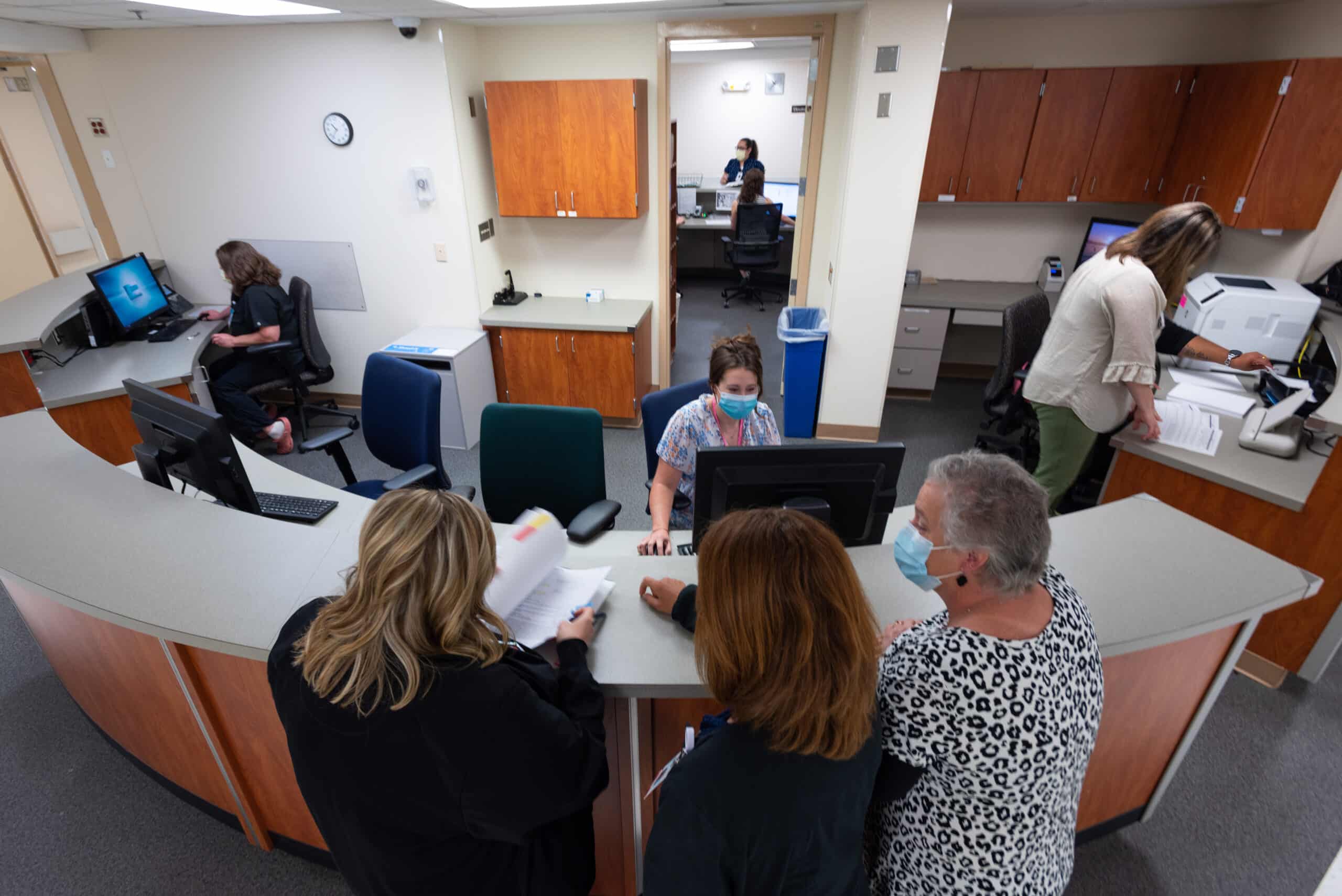
Previously, the transplant team worked in separate clinics, sometimes limited to three rooms. 3 South Transplant offers 18 patient exam rooms, which in addition to consolidating space for patients, will also help to shorten wait times for new referrals and follow up appointments.
Another benefit of 3 South is the accessibility of team members such as dieticians, social workers, pharmacists, nurses and physicians, which provides patients the accessible support of various teams of health care workers critical to patients’ transplant journeys.
Lastly, this consolidation allows for expansion of potential future services such as phlebotomy, expanded pharmacy services, infusion services and vascular access.
In 2022, as we build the future of ECU Health, the exceptional care and services we provide have a positive impact on the communities of eastern North Carolina that we serve through our considerations of patient quality and experience.
For more information on transplant services at ECU Health, visit the transplant section of our website.
A team from the Brody School of Medicine’s Internal Medicine Residency Program won first place and the Osler Cup in the American College of Physicians Doctor’s Dilemma competition.
Coached by Dr. Lacy Hobgood, clinical associate professor in East Carolina University’s Department of Pediatrics, the team competed for three days against some of the world’s brightest medical residents, including teams from the United States, Canada, Central America and the Caribbean. Drs. Alex Bradu, Omar Khdeir and Swethaa Manickam earned the right to compete at the national level by first winning the North Carolina chapter’s competition.
Past winners of the ACP Doctor’s Dilemma competition include the India chapter, Albert Einstein Medical Center, Indiana University School of Medicine, Northwestern University and the Mayo Clinic.

Khdeir said Doctor’s Dilemma is the biggest competition based on knowledge of internal medicine, featuring as many as 60 teams each year in a friendly but highly competitive environment. The format is similar to the television show “Jeopardy,” with each game consisting of a set of questions teams must buzz in to answer, and a final round in which they must wager their points before seeing the question.
“We wagered all of our collected points in the final dilemma and got the question right,” Khdeir said. “After we won, we took turns calling our parents on speakerphone. Seeing our parents and siblings proud and happy was the biggest award.”
Dr. Herb Garrison, associate dean for graduate medical education, said the team’s performance on the national stage reflects the quality of medical education at Brody and also helps enhance its reputation.
“They competed against the best residents from around the world in a test of medical knowledge and speed and emerged as the winning team,” Garrison said. “In addition to demonstrating the type of great physician trainees we have at the Brody School of Medicine and ECU Health, this win provides us a huge recruiting advantage as other schools will take notice and want to send their best medical students our way. … I couldn’t be more proud.”
The Internal Medicine Residency Program is an integral part of the Brody School of Medicine and the ECU Health Medical Center. The Department of Internal Medicine includes nine subspecialty divisions and serves the Greenville and Pitt County area as well as 29 surrounding counties.
Read more from ECU News Services.
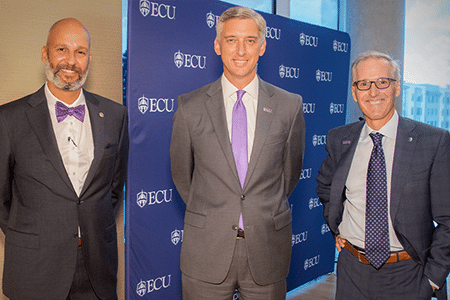
Dr. Mike Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University was recently named to Business North Carolina’s 2022 Power List. ECU Chancellor Dr. Philip Rogers was also named to Business North Carolina’s 2022 Power List in the Education section.
This yearly list names the most influential leaders in the state of North Carolina across various industries. The awarded leaders are nominated for this list based on their influence as strong leaders.
“This recognition represents the tireless work ECU Health team members do every day to serve the region and educate the future physicians for North Carolina,” said Dr. Waldrum. “At ECU Health, we strive to become a national model for rural health delivery by providing high-quality care to the region we proudly call home. Our regional health care organization, combined with the Brody School of Medicine, strengthens our shared mission to improve the health and well-being of eastern North Carolina. ECU Health will continue to innovate and provide high-quality care to those we serve.”

We are proud to have strong leadership moving ECU Health forward to meet the joint mission of improving the health and well-being of eastern North Carolina by training the providers of tomorrow, collaborating with community partners to solve complex issues and bringing clinical innovations that improve the lives of those who proudly call this region home.
To read the Business NC Power 100 List article, please visit https://businessnc.com/2022-power-list/.
It’s a natural evolution for two organizations that have worked together for years.
“This announcement has been 40 years in the making,” said Dr. Michael Waldrum, Vidant Health CEO and dean of East Carolina University’s Brody School of Medicine.
“We are super excited for this name change, said Vidant team member Carol Ramirez, RN. “I think it’s going to be a really, really good change for eastern North Carolina.”
“This is not a moment to sit idle,” said ECU Chancellor Philip Rogers, upon the announcement of the joint operating agreement in January 2022. “It is instead a moment to launch an innovative solution for rural health care delivery and education in eastern North Carolina. And that is exactly what we aspire to do with this announcement.”
With a logo reveal that followed in April and a transition to ECU Health that will begin in May, it is an exciting time for eastern North Carolina.
“As with any change, there is a lot of angst about ‘what’s the future for me as an individual within the organization,’” said Jason Higginson, executive dean of the Brody School of Medicine at ECU. “I think one of the key things, our guiding principal, is the people within the organization are equally important to achieving the mission as anything. So, as we look to the future, we are trying to ensure that everyone in the organization is valued and that their contributions are honored.”
It’s a process that will take months to complete. The Vidant Health logo will be phased out over the next two years, replaced by ECU Health on everything from building signage and vehicles to organizational websites and social media channels.
“There is a plan to roll that out,” said Dr. Waldrum at the logo announcement in April. “And today we are showing the brand but beginning in May you’ll start seeing that happen and that will evolve over time.”
These changes will unfold across hundreds of locations in 29 counties. A visual unveiling of a forward-focused partnership benefitting those who serve — and are served by — the health system and the Brody School of Medicine.
“I think it’s awesome that two of the biggest entities here in town have collaborated to support and help the whole eastern North Carolina,” said Vidant team member and social worker Robinque Willis-Brown. “So together, I know they can make a great difference.”
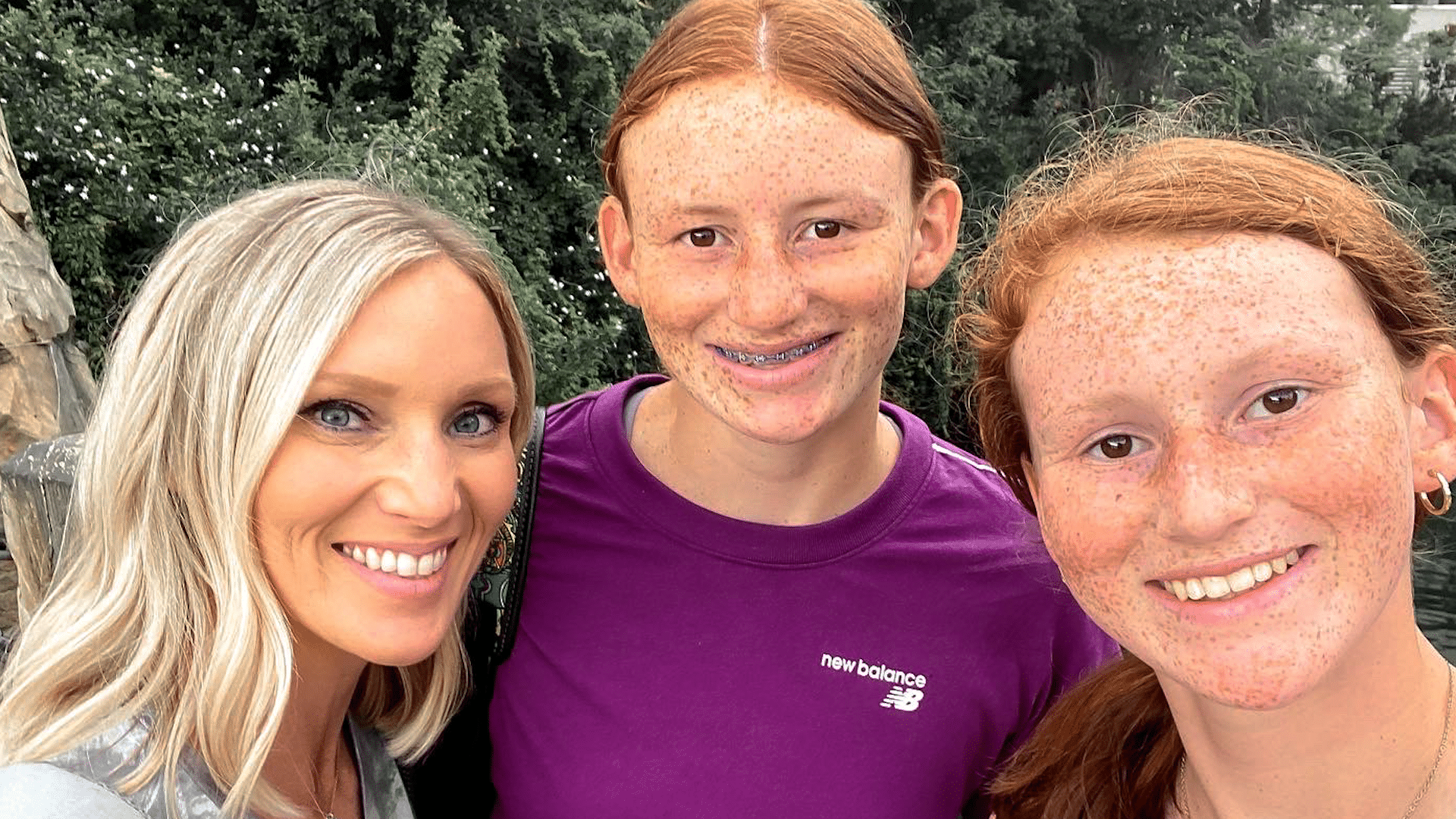
It started out as a typical holiday weekend for Dana Parker and her two daughters.
“We had plans to go hang out with my family the next day, for a cookout,” Dana said, about their plans last summer. “Fourth of July is a big holiday in our family.”
But overnight, those plans for a celebration quickly changed.
“I woke up a few times the next morning and thought, ‘Man, the house is really quiet. I’m surprised the girls aren’t up yet,’” Dana said.
Next came a horrifying discovery, as Dana found her oldest daughter Parker unresponsive on their living room floor.
“She’s just covered in vomit. She had definitely aspirated, I can hear it gurgling in her lungs,” Dana said, as she recounted the experience that day. “Her body is cold, I mean it is cold, stiff, she’s not responsive at all.”
Dana then finds herself reeling as first responders hone in on a possible cause. “They just kept saying, ‘Do you think it could be an overdose?’ They’re hooking her up to all these things and they just keep going back, like ‘Ma’am, she’s young, she’s healthy, all of these symptoms point to an overdose,’” she said.
Evidence found on Parker’s cell phone confirmed those suspicions. “In the course of about 25 minutes, she consumed almost 26 shots of alcohol,” Dana said.
“Depending on how old you are, how much you weigh, how much alcohol you’re ingesting, every child is different in terms of the effect it’s going to have on you,” Nicole Belcher, PA-C, a physician assistant at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center (VMC).
In Parker’s case, she consumed enough alcohol for the care team at the Children’s Emergency Department at VMC to warn of an unknown outcome.
“They said, ‘At this point we don’t know if she’ll wake up. And if she does we have no idea what condition she’ll be in,’” Dana said. “She was already on borrowed time. I mean, it is literally by the grace of God that she was even still breathing at that point.”
Breathing then – and thriving now. While minor nerve issues persist, the multi-sport student athlete has made nearly a full recovery. And Dana is grateful for the care her daughter received.
“The little things that they do mean more than what they realize. Just the little kind words and taking the time to ask the questions and to say, ‘Hey, are you ok? Is there anything I can get you?’ I would just love to say ‘thank you,’” Dana said.
Now Dana wants other parents to learn from her family’s experience, and to consider how they talk to their children about the dangers of drinking.
“In her eyes, maybe she was drinking responsibly. She wasn’t out on the street, she wasn’t at a party, she wasn’t driving, you know – she’s in the comfort of her own home. She gets curious, she wants to experiment,” Dana said.
Experts agree.
“Bottom line, is to have the conversation. I think the earlier we walk about it, the better,” said Belcher. “The reality is, they are going to learn it from you, or they’re going to see it on social media, they’re going to see it on television, they are going to see it on the movies. Being able to have that open communication and being able to model safe behaviors with alcohol is the most important thing.”
Resources
April is Alcohol Awareness Month. If you or a loved one needs support, resources or treatment, the Substance Abuse and Mental Health Services Administration (SAMHSA) can help.
SAMHSA’s National Helpline is free, confidential and accessible 24 hours a day, seven days a week: 1-800-662-HELP.
They also offer an online treatment locator: https://findtreatment.samhsa.gov/
Watch more ECU Health News videos
Each day at Vidant Health, incredible nurses go above and beyond to care for the patients and families of eastern North Carolina.
In February, ECU Health Medical Center (VMC) volunteer Frank Crawley had a moving experience with nurse Felicia Parker at ECU Health Cancer Care that he felt compelled to write about.
“What you don’t know is you did something to me that day,” Crawley said to Parker, as the two met again exactly a month after their interaction. “You moved me to do some things that I’ve wanted to do for a long time. That’s to write about some things having to do with this hospital and how much it has meant to me.”
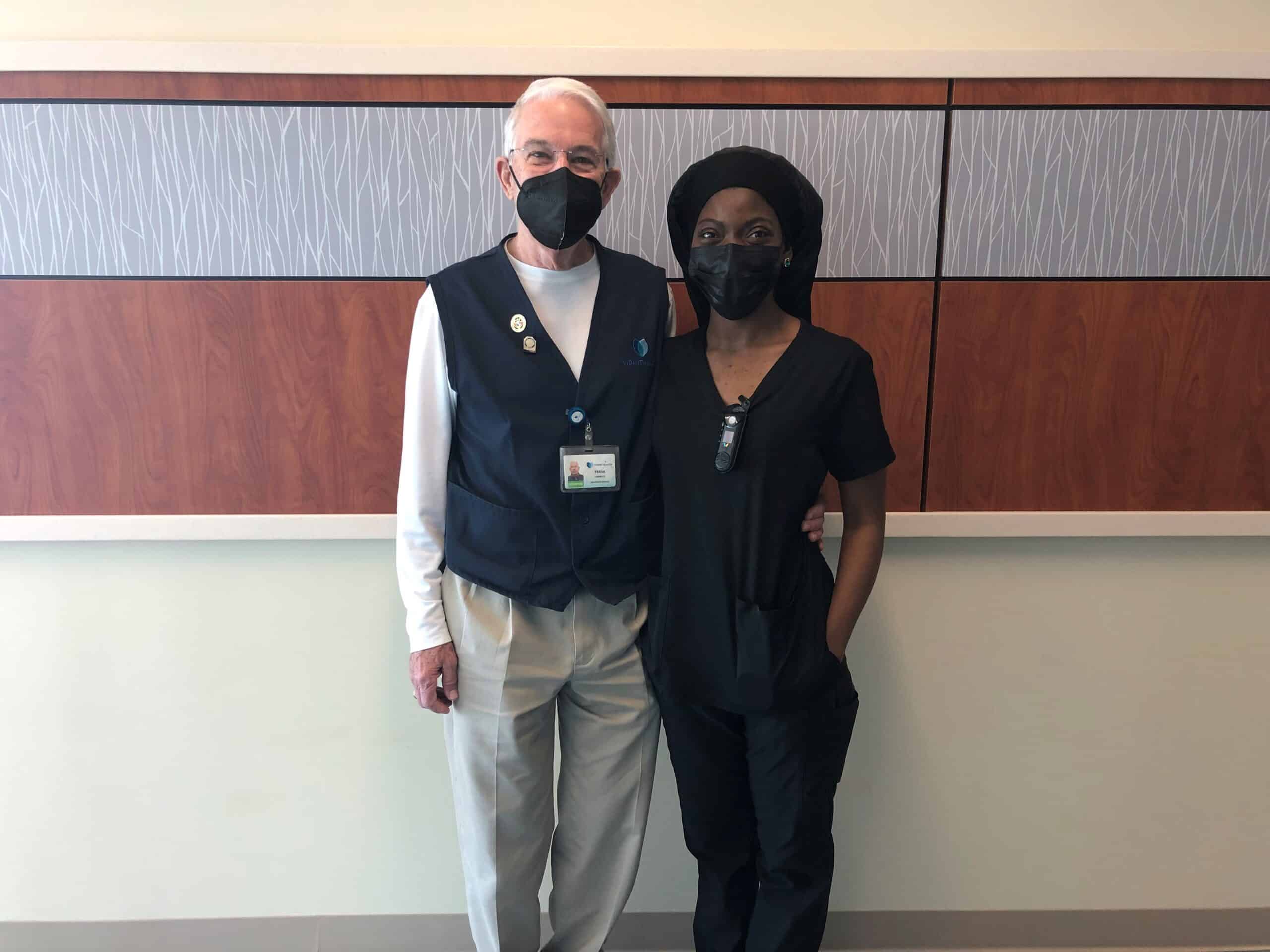
This National Health Care Volunteers week, we are proud to share the below story written by Crawley after his experience at VMC.
“On the morning of Feb. 15, 2022, a call came to Patient Escort to bring a wheelchair to the Cancer Center, room 418, to transport a patient to the Dental Clinic. I took the call. When I arrived, I knocked on the door, opened it, greeted the occupants and announced that I was there to take the patient to the Dental Clinic. Lying in the bed was a frail, elderly man. Standing by his side was his wife, who immediately said there was no way her husband was able to make the trip to the clinic in a wheelchair.
I left the room and located the nurse assigned to room 418, whom I later learned was Felicia Parker. She and I both entered the room. Ms. Parker explained to the patient’s wife that her husband desperately needed dental work. The wife seemed very concerned that her husband lacked the strength to make the trip, that his blood pressure would drop and that he could have a seizure, particularly if taken in a wheelchair. She said that he might be able to make the trip in his bed. The soft-spoken Ms. Parker explained that the bed was too large to transport into the clinic. Additionally, she said that to alleviate the wife’s concerns, she would accompany her husband to the clinic, assuring her that every precaution would be taken. First, she explained that we would exchange the Staxi for a Stryker wheelchair, carry an oxygen tank with us, along with a blood pressure/heart rate attachment to monitor her husband’s vital signs.
The wife began to weep quietly. She walked into the bathroom and continued to sob, fearing for the welfare of her husband. Ms. Parker followed her to the bathroom. She spoke softly, lovingly to the patient’s wife, hugged, consoled and reassured her that we would take every precaution to see that her husband made the trip to the clinic without incident. Still hugging, Ms. Parker told the patient’s wife that she would call her once we reached the clinic. I was so impressed at that moment with the love, patience, caring and empathy Ms. Parker showed her — far beyond what I had expected to witness that day. With the wife comforted and reassured, Ms. Parker and I located a Stryker chair, added an oxygen tank and a vitals’ monitor. Next, Ms. Parker said that she was raising the bed to a sitting position so that the patient could sit upright for a few minutes and adjust to the change in position. Doing so, she explained, we would be able to see whether his blood pressure and heart rate would respond favorably to the positional change. Next, Ms. Parker and I moved the Stryker chair next to the bed and slowly moved the gentleman’s feet off the side of the bed. All went well — at first.
Within seconds of moving his feet off the bed, there was a sudden drop in the patient’s blood pressure and a change in heart rate. Carefully but quickly, Ms. Parker moved the patient’s feet back onto the bed and slowly lowered the bed. She immediately left the room and called for backup help — not calling for a “code blue” but the next level below, as I heard her say. Within a few minutes, the room was filled with attending physicians, nurses and aides. I quickly moved back, stepping out of the room to allow Ms. Parker and the medical staff space to work. Within what seemed like only a few minutes, the patient’s vital signs were restored to normal, and the room was calm again. Ms. Parker then turned to the patient’s wife, hugged and comforted her.
With the room restored to calm and the father’s vitals stable, Ms. Parker came to me and thanked me for my help.
“No,” I said. “Thank you for allowing me the privilege to witness, firsthand, nursing at its very best.”
Not only was Ms. Parker highly competent, as evidenced by the technical skills she displayed, she also possessed that rare ability to sincerely comfort, console and empathetically connect with the very distressed patient’s wife. Empathy is near impossible to teach. Neither can it be faked. Deeply moved and with tears in my eyes, I hugged Ms. Parker.
“Never had I expected to report to volunteer duty Tuesday morning and see the loving, compassionate face of Jesus on display,” I said.
That day was most rare and wonderful, and I knew it.
After writing down his experience, Crawley shared this with the volunteer team and eventually it found its way to Parker. When she received the email, she had her daughter read the story to her sons. Parker said she was moved by him sharing his experience with her and her family.
“It’s nothing that I gave a second thought to – it’s just what we do every day,” Parker said, who will celebrate three years in the system in June. “Sometimes we kind of don’t look at what we do, how it impacts others. Especially, we feel like it’s just something that we’re just supposed to do. You’re supposed to get up, you’re supposed to greet people when we see them. We don’t think anything of it. That’s what it was for me. It was just, ‘Hey, what you do does matter.’”
Crawley said he has been volunteering at the medical center for nine years. Previously, he was an education professor at East Carolina University.
“In the busyness of life, and I think it has a lot to do with my age, I look for those moments that I can connect with people or when I can see them connecting, because I believe that’s what we were born to do,” Crawley said.
“We do a lot of things for which we get paid and it’s difficult to find something in you down deep that in that busyness,” Crawley said. Then looking at Parker, he continued, “I know you had lots of other patients, but in that busyness to console the woman who wasn’t your patient. You saw something there that was a greater need and you met that need. That was just powerful.”
We are so proud to have experiences like this unfold along the halls of Vidant hospitals each day. Thank you to the care teams, volunteers and team members who serve eastern North Carolina. If you are interested in joining the Vidant team, visit our Careers site.
Greenville, N.C. – April 14, 2022 – Vidant Health and East Carolina University are excited to announce a logo for the ECU Health system, which will launch in the region starting in May.
“Eastern North Carolina’s vibrancy depends on strong collaboration between the institutional pillars that have long represented this region’s unique needs,” said Dr. Michael Waldrum, Vidant CEO and dean of ECU’s Brody School of Medicine. “The ECU Health logo is a symbol of our shared commitment to transforming and elevating health care for millions, training the providers of tomorrow, collaborating with community partners to solve complex issues and bringing clinical innovations that improve the lives of those who proudly call this region home.”

The ECU Health logo captures the essence of an innovative regional health system comprised of more than 13,000 dedicated health care workers, a thriving university, current and future generations of doctors committed to caring for North Carolina and the unwavering commitment of two organizations working collaboratively to transform the East.
“It is exciting to be a part of ECU’s continued transformation as we work to build pathways for sustained excellence here in Greenville and the region,” said ECU Chancellor Philip Rogers. “This partnership strengthens our institutions’ shared mission and ultimately betters the communities we serve. Sharing the new ECU Health logo begins an exciting chapter as we work collaboratively to build the health care enterprise for the region and expand our reach further into eastern North Carolina.”
The rebranding process for most Vidant entities is expected to begin in May and will take several months to complete. The Brody School of Medicine’s name will not change.
Naming conventions are as follows:
Hospitals:
- ECU Health Medical Center
- ECU Health Beaufort Hospital – A Campus of ECU Health Medical Center
- ECU Health Bertie Hospital
- ECU Health Chowan Hospital
- ECU Health Duplin Hospital
- ECU Health Edgecombe Hospital
- ECU Health North Hospital
- ECU Health Roanoke-Chowan Hospital
- The Outer Banks Hospital
- ECU Health Maynard Children’s Hospital
Other entities:
- ECU Health Physicians and ECU Physicians: the naming of the practice groups will be shared at a future date.
Vidant and ECU have a rich history of collaboration in health care, education and research. Vidant’s role as a regional rural health care leader, and Brody’s status as North Carolina’s leader in graduating physicians who practice in state, in primary care and in underserved areas is a natural partnership that will advance the combined mission of ECU Health.
ECU Health will strive to more effectively and efficiently address current issues facing the region – such as health disparities and care delivery obstacles – while also better anticipating future health care and educational needs.
“The rebranding to ECU Health is symbolic of the importance and longstanding cooperation of ECU’s Brody School of Medicine and Vidant Health. Together, we have long stood side by side advancing the health delivery, research and education mission for eastern North Carolina,” said Dr. Jason Higginson, executive dean of the Brody School of Medicine. “Having one brand will make our close and important relationship apparent to everyone.”