In a ceremony more festive than formal, fourth-year medical students in the Brody School of Medicine at East Carolina University learned March 15 where they will spend the next three to seven years completing residency training.
This year, 100% of Brody’s 79 members of the Class of 2024 — which began its medical school journey during the COVID-19 pandemic — matched with a residency program.
The traditional event is arguably the pinnacle of the medical school experience for Brody students.
Before they opened their envelopes to reveal their next stop, the students were presented to the audience of family, friends and members of the Brody community to strains of music they each selected as they marched — or danced — across the stage in the ballroom of ECU’s Main Campus Student Center.

“Match Day is such a special time for these students from the Brody School of Medicine, all of whom have worked incredibly hard to reach this exciting moment,” said Dr. Michael Waldrum, dean of Brody and CEO of ECU Health. “Our medical students, by virtue of the education they receive here at Brody, are uniquely prepared to provide high-quality, human-centered care to the patients they will soon serve as part of their residency training and beyond. I want to extend a heartfelt congratulations to the Brody Class of 2024. We are grateful for the positive impact they will have on the lives of so many.”
Dr. Jason Higginson, executive dean of the Brody School of Medicine, said the class of 2024 represents Brody’s mission — a diverse group of students who come from all parts of the state, who will largely return to serve North Carolina as doctors.
“We have a 100% match rate, well above the national rate, which is also a testament to our faculty and staff,” Higginson said. “About 50% of our graduates are staying in North Carolina, which is our primary mission, and about 20% are staying locally.”
One of Brody’s secondary missions is getting future doctors to practice primary care, and half of the class of 2024 have committed to being on the front lines of health care.
“They are great kids. It’s one of our best classes ever,” Higginson said.
A perfect match
Before he even knew the mission carved out by the Brody School of Medicine to reach underserved patients and address health disparities, Connor Haycox was intent on improving lives.
During his undergraduate years at Davidson College, Haycox volunteered and interacted with patients from underserved communities and saw himself as a future physician to help bridge gaps in care.
“I wanted to go into medicine to help address that,” said Haycox, a native of Chapin, South Carolina. “I could see myself as a primary care physician; I figured I could do the most good for people on the front lines.”
Haycox matched in family medicine at ECU Health.
“I know this is where I’m supposed to be,” he said.
After college, Haycox spent two years completing a MedServe fellowship — an AmeriCorps program through which fellows assist in key primary care services and engage in community health work including outreach, education and other projects that impact community health. During the fellowship, Haycox worked in a rural family medicine practice in Benson, North Carolina, where he witnessed “the breadth of the problems patients presented,” he said. “I wanted to be able to meet them in their particular situation and help them maximize their health goals. I really started to see myself in that role.”
By the time Haycox was ready to take on medical school, he knew Brody was the place for him. His goals and his philosophy naturally aligned with the school’s mission, making it a perfect fit.
“The mission of Brody to develop family medicine doctors to serve the state was really a natural transition for me,” he said. “It just made the whole process that much more streamlined. I saw myself here from the start.”
Haycox sees himself serving eastern North Carolina long term — especially since his wife, Dr. Natalie Malpass, a 2022 Brody graduate, is completing a family medicine residency with ECU Health. The two met during Haycox’s stint in Benson, and that experience has cemented his view of medicine as part of teamwork and partnership.
“I think it’s invaluable to have a partner in medicine,” Haycox said. “It’s such a challenging field and an emotional investment, and I feel like having someone to be able to talk to about the things you see has helped me professionally, but it’s more just being able to walk through life with someone who understands.”
Working with the Benson clinic to respond shortly before medical school to help the team coordinate the practice as a COVID-19 testing site also showed him the importance of taking unforeseen circumstances and transforming them into something meaningful.
“Medicine is personal, and we adapt,” Haycox said. “We do that because we need to for our patients. The pandemic was a whole learning process, and it taught me that we may not have all the answers, but we can learn with our patients how to best come out.”
Navigating the pandemic with his classmates also taught him lessons about adaptation, appreciation and taking advantage of opportunities that presented themselves over the years. Haycox served as an anatomy tutor and was part of Brody’s Medical Education and Teaching Distinction Track cohort — which prepares students to be effective medical educators and develops their interest in academic medicine.
“I can see myself going into academic medicine in the future, so I wanted to develop those skills,” he said.
As for the culmination of his Brody experience, Haycox is excited to celebrate his next step alongside his family. For him, Match Day is the beginning of a new adventure in primary care and family medicine.
“Medical school is a long haul, so I’m excited to celebrate with my family,” he said. “Today, all of this kind of becomes more real.”
From motherhood and maternal medicine
For most medical students, finding out where they will complete their residency during Match Day is plenty to celebrate. For Ahoua Dembele, that’s just the start of the day’s festivities as her family is in town for an equally joyous celebration: a baby shower for her third child, due in just four weeks.
Dembele moved with her family from her home in Ivory Coast to Senegal, then attended boarding school in France. She returned to Africa’s north coast, this time Tunisia, with her family for six years before finally settling in Charlotte after graduating high school in 2011.
When Dembele arrived in the States, she had some measure of command of a number of languages – French, Arabic and an understanding her first language, Dyula, a dialect of Mande, but she didn’t speak English. She enrolled at Central Piedmont Community College for a crash course in a new language and started her educational journey.
After a few years at the community college and managing a pizza restaurant, she transferred to UNC Charlotte, where she graduated with a degree in biology because she was always fascinated with science.
She soon had her first son and worked for a while as a medical assistant in a doctor’s office in Charlotte.
Dembele was accepted as a medical student at Brody just before the COVID-19 pandemic complicated just about every aspect of life – especially education. The disconnected learning was tough, but she excelled, especially in light of having her second son just before starting school and getting married to her long-time partner who was frequently out of the country for business.
“I started medical school when my oldest was 2 or 3 and my youngest was 1. Daycare regulations were a little weird and my school was, too. We couldn’t go to Brody because of COVID, so I had to find ways to study,” Dembele said.
Her mother stayed with her to help with the boys and when her husband was home “he would do everything so that I could find places to study, but it was hard because they still need their mom, so I had to find ways to at least do bedtime every day.”
Dembele matched to undertake her residency in obstetrics and gynecology at ECU Health. She wants to make a difference in the lives of mothers and babies, especially after witnessing health conditions in eastern North Carolina through her clinical rotations. She hopes to sub-specialize in maternal and fetal medicine.

“Something about pregnancy has always attracted me. It’s miraculous, phenomenal, that a body can do that,” Dembele said. “It’s mind blowing. I’ve seen a lot of deliveries, but I’m always amazed, every time, even at my own.”
She credits Dr. Jill Sutton, a clinical associate professor at Brody who specializes in obstetrics and gynecology, with invigorating her desire to focus on pregnancy and women’s health.
“The first time she taught us she was so bubbly, so excited and so joyful when she was talking about pregnancy,” Dembele remembered. “Her enthusiasm, her devotion. I was like, ‘Oh my God, this is who I want to be.’ She’s been a mentor for a long time, and I hope to stay here and continue to train with her.”
At Match Day, Dembele was joined by her husband, her boys and her mother, who traveled from Wisconsin, where they now live. She beamed with pride amidst a family that had travelled so far, and made real sacrifices, to stand with Ahoula as she tore open the envelope that revealed where the next few years of their lives would play out.
Dembele will have a few weeks with her newest child before starting residency as she and her husband planned — calculated — the pregnancy meticulously.
She is a scientist, after all.
‘That’s the kind of doctor I want to be’
The few minutes it takes for the National Resident Matching Program’s mathematical algorithm to match applicants and programs across the country can be daunting for many medical students to think about — but for Emmalee Todd, reflecting on those fateful moments feels a bit zen.

“I think that no matter where I end up, I will find a way to be happy and fulfilled and feel like I’m moving in the direction I want to move in,” Todd said. “I feel like regardless of where I have ended up, I’ve been able to find my own path in that setting.”
And they will do it again.
Todd, who crossed the stage to the inspiring lyrics of Shakira’s “Try Everything” from the movie “Zootopia,” was joined by their parents and girlfriend Friday as they opened their envelope to reveal that they matched in internal medicine and pediatrics — known as “med-peds” — at the University of Maryland.
“I’m really excited,” Todd said. “Maryland made a really good impression on me. I’m excited for it.”
Todd’s journey through medical school was inspired by leadership experiences, bonding with fellow students and learning to adjust to what comes in ways that ensured not only success but a lesson to carry with them into the next chapter. A member of Brody’s first class to begin medical school under “pivoted” protocol because of the COVID-19 pandemic, Todd said their class made up for lost time later.
“For most of us, 2020 was pretty lonely,” they said. “We were thrown into this whole new level of work and new level of stress, and we wanted to be able to lean on our classmates.”
The Class of 2024 leaned into the changes, however, and started forming bonds as they interacted during some classes and labs and outside of school. Those bonds have stood the test of time and have been a vital part of Todd’s experience — which really began when they were an undergraduate at Northeastern University in Boston studying behavioral neuroscience.
Todd became an emergency medical technician and got a firsthand look at medical care — after getting a taste of the health care field over the years from their mother, Dr. Karen Todd, a pediatrician and Brody alumna herself. That exposure, coupled with making friends from all over the country and world, helped lead Todd toward a career in health care.
“I was meeting people from places I’d never been before,” they said.
After working for two years as a medical assistant, Todd brought that same energy to Brody, where they could see themselves as part of a smaller class.
“It really came down to the vibes,” they said. “It was one of the few places I interviewed where I felt a connection to the people, students and faculty right away. I could see myself here.”
Todd has thrived, taking on leadership roles including class diversity representative, executive treasurer and vice chair on the Medical Student Council, an elected organization that represents the medical student body as a voice in education, political and social interests.
“I got nominated our first year and decided I was going to run,” Todd said. “I got elected, and there I was. When you’re asked for your input, it’s because someone thinks your input is valuable. It is an honor, the trust [my classmates] have placed in me to be a voice for my class, to speak up and advocate for changes, policies and guidelines that are going to improve or rectify parts of our experience.”
Todd, who was drawn to med-peds because of an experience during a third-year rotation.
“I was trying to be open-minded, though I initially thought I wanted to do emergency medicine,” Todd said. “During my internal medicine rotation, I spent two weeks in the med-peds clinic and fell in love with the feel of it, with the attendings and residents and their personalities and the way they thought about medicine and approaching their patients. The more I got to interact with them, the more it reinforced that that’s the kind of doctor I want to be. They were passionate about trying to do the right thing for their patients.”
Drawing upon every memory and experience they gained along the way — from undergrad to Match Day — Todd is ready to embrace the next step and to take advantage of all the lessons waiting on the horizon.
“I thought when I was in undergrad that I wanted to get my Ph.D.,” they said. “I love neuroscience; I loved feeling like I was on the cutting edge of the frontier of knowledge, pushing into something that people have never known about before. But the more I got into the clinical environment, I really liked the detective work aspect of medicine, the team feel of it. All of the members of the health care team bring their own skills to the table but have the same goal, which is making the patient better.”
Stay on ECU Health’s rehabilitation unit inspires Kasey Shue to pursue recreational therapist degree
To be a health care provider is to answer a calling. For some, the journey to health care is a straight line; for others, the road is winding. This series features stories from ECU Health team members who took the winding road, but found the destination to be worth the effort.
Kasey Shue, a recreational therapist, had no idea that a fulfilling career in health care was awaiting her when she got sick nearly eight years ago.
“I had an undergraduate degree in public relations and communications from East Carolina University,” Shue said. “I worked for the American Red Cross educating people about and coordinating blood drives. Then I went to the hospital with Guillain-Barre syndrome.”
Guillain-Barre is a condition in which a person’s immune system attacks the peripheral nerves, and it can result in near-total paralysis and breathing problems in the most severe cases. Shue’s case was, she said, pretty severe.
“I needed help with everything: I had to learn how to chew, swallow, sit, stand and walk again. It was like being a toddler.” Even more than the physical stress, Shue said that the emotional burden of being in the hospital was trying. “I had a husband and two small children at home,” Shue said. “We actually held my son’s second birthday party in rehab while I was there. It was difficult being away from my family and coming to grips with not being able to do the most simple of things.”
Shue spent two and a half months at ECU Health Medical Center, six weeks of those being on the rehabilitation unit. During her stay, Shue said all therapies were instrumental in her recovery, but recreational therapy (RT) made the biggest impact.
“I didn’t know what RT was before I was in the hospital,” Shue said. “RT affected me the most because it helps people keep being who they are despite their physical barriers. RT helped me schedule my son’s birthday party, and they took me on an outing to Target.” During her stay, Shue said she had a literal epiphany: “It hit me – I was going through this so I could go back to school to be an RT and give back. I wanted to pay it forward.”
After her recovery, Shue went back to school and graduated with her master’s degree in recreational therapy from East Carolina University. She also added an aquatic therapy certification to her degree because of her own personal experience in the therapy pool.
“Aquatic therapy was extremely beneficial to my recovery, so when I went back to ECU I was determined to get that certification,” Shue said.
Shue also knew she wanted to work in inpatient rehabilitation because, “you see people get better in a short time frame, and I like seeing that progress.” She didn’t know, however, that she’d end up working for ECU Health in the same rehabilitation unit where she recovered just a few years prior. “I had no idea I’d end up back here in the Medical Center, but in a lot of ways, it’s my perfect job to come back and help people in the same facility where I received help.”
Shue attributed her success both to the skills she learned in her previous career and the experiences she had as a patient.
“From my work with the Red Cross, I was already familiar with this hospital, as well as general health and wellness education. I also know how to work with people – not everyone does that well.” Shue said her time in the hospital gave her a unique perspective that allows her to be more empathetic with her patients. “I can relate to patients on a different level because I’ve been the one in the bed not wanting to get up or feeling like I couldn’t do the work. I have a rapport with patients and help them work through their pain. It’s made me successful in the patient care side of things.”
That professional perspective also bleeds into her personal life. “I tell people that now I’m Kasey version 2.0,” Shue laughed. “After being sick, I don’t take things for granted. I have more empathy for people, and the smaller things don’t stress me out like they used to.”
Shue said it’s an honor to work with the rehabilitation team, some of whom were there when she was a patient.
“A lot of my primary therapists when I was sick have moved on to other roles, but we still pass each other in the halls and have that relationship,” Shue said. “And some of my former therapists work with me every day. I have a professional respect for them, but we also have a deeper bond because they watched me and helped me get better.”

Working beside the people who helped her and providing services to people who are in the situation she was in eight years ago is gratifying.
“I really enjoy what I do, and it doesn’t feel like work. I tell people that I get paid to play.” Shue is also the handler for Clive, a dog who is a part of the Animal Assisted Therapy program and who helps patients in the rehabilitation unit a few days a week. “I’ve always been a dog lover, and as a patient I had several dogs that visited me. I knew pet therapy fell under the RT umbrella; the pieces came together so we could have Clive come in and work with our patients.”
Shue said these professional experiences fill her cup in a way her previous career did not, and her advice for anyone considering a career change to health care is to listen to their instincts.
“Life challenges, whether professional or personal, happen, and sometimes it requires you putting yourself out there and stretching your comfort zone,” Shue said. “If something draws you, listen to that pull. I’m a big believer that things work together for the good, even if you can’t see it initially. I didn’t ask to be sick, but it impacted my entire future in a positive way. Now I feel like I’m right where I’m supposed to be, doing what I’m supposed to do.”
Resources
In the years following the onset of the COVID-19 pandemic, health care as a whole has fundamentally changed — as have the lives, habits and health care needs of communities across the country.
Today, emergency departments (EDs) everywhere are seeing high volumes while staffing shortages persist. In rural areas with communities that are sicker than many others, these challenges are even more magnified.
“I’ve got patients who can’t see a doctor in the community mixed in with patients who have a pulmonary embolism,” said Dr. Leigh Patterson, chief of services for Emergency Medicine at ECU Health Medical Center and chair of Emergency Medicine at Brody School of Medicine at East Carolina University. “My team and I are trying to see the forest through the trees. Who’s the patient that needs the services? Everyone needs the services, but who’s the patient that medically needs the services next? And that’s hard.”

Meeting the challenge
At ECU Health Medical Center and throughout ECU Health system hospitals, leadership teams have needed to adapt quickly to meet the needs of the many patients seen through EDs.
Alex Baylis, ED nurse manager at ECU Health Medical Center, said she has been proud to see the department’s flexibility and persistence while helping patients through their time in the ED.
“We have flexed and bended, added and changed our spaces, we’ve changed our beds, we’ve changed our staffing patterns, we’ve changed our hours of when team members come in, when team members go home. We’re doing all that we know to do, and have the power to do, to get care to our patients faster and better,” Baylis said. “Right now, we’re facing really difficult barriers and obstacles within our space that are challenging, but we’re doing everything that we can and know to do to help our patients.”
Dr. Patterson echoed Baylis’ sentiment.
“We’ve tried, we are going to continue to try and it isn’t going to look the way it used to look,” Dr. Patterson said. “I think patients have been very understanding when we’ve had to do things in a different way. It is a really ugly reality right now, but we’re going to flex a lot. What I really want people to understand is what you see in the ED is actually all of the hospitals and all of health care right now.”
Matter of perspective
Dr. Patterson said she has seen a great deal of change in eastern North Carolina since she first came to the Brody School of Medicine and ECU Health Medical Center 17 years ago.
When she arrived at what is now ECU Health Medical Center, she became just the fifth female emergency medicine clinician. Today, she said, there are more females than that in the intern class alone.
“I am not the generation that was the first and only,” Dr. Patterson said. “I had other female residents who were with me. We were definitely the minority, but we’re not such a minority today.”
Dr. Patterson estimated there to be about a 50/50 male to female split among emergency medicine training program graduates across the country today and more women are holding education leadership positions.

However, that same shift has been slower to develop on the administrative leadership side.
“It takes some time to get all the way up the ranks so there are probably a dozen women chairs in academic medicine and emergency medicine and other positions like mine,” Dr. Patterson said. “But really, not a large number of us when you consider there are a couple hundred of our programs.”
From an outsider’s perspective, the number of female leaders in the ED may seem unique, but to those on the floor, it’s nothing to bat an eye at.
“We’re kind of past that – ‘Look, that’s so cool.’ Some days we’re still there,” Dr. Patterson said. “A lot of days it’s like, ‘Oh, yeah.’ I mean, I don’t think our nurses notice. We could go 24 hours in one area and it’s all women physicians and it’s just like that’s Tuesday. We don’t stop and notice that.”
Baylis noted that from the nursing perspective, more males in nursing tend to gravitate toward EDs and Intensive Care Units, but on the leadership side it is predominantly females.
Dr. Patterson reflected on the early part of her career and how conversations have shifted and become more normalized. Whether it’s the way patients address female providers or the interactions teams have with each other, she has seen positive change.
“I have men, physicians now who can have open discussions about, ‘Hey, how are you taking your FMLA leave when you have a baby? Are you splitting it, are you taking it at the end?’ The normalization of those conversations, that’s what comes from it,” Dr. Patterson said. “We’re not there all the way, we still have a long way to go. But it was not this normal in my first job.”
Providing compassionate care in trying times
As the care needs in EDs have changed, Baylis and Dr. Patterson noted how crucial it is to connect with patients on a human level and provide high-quality, compassionate care in stressful situations.
Baylis said the mindset of nurses in the ED has changed drastically in the past few years.
“In emergency nursing, you had to have tough skin and be almost hard,” Baylis said. “I think it’s changed with the population that we’re seeing in our patients, but also the care that we’re giving. We’ve learned to be more soft and more caring and taking that time to make a connection. We can be nice while still setting boundaries with our patients.”

Dr. Patterson said providing care in eastern North Carolina is a very unique situation. She shared that she trained at a county hospital in New Orleans and that in large, urban environments, it’s less common that she or her family members would be patients at the same hospital at which she practices.
Here, there is no line.
“So much of what I saw when I was in my own training, in my mind, I could pretend it wasn’t going to happen to me and you get this lovely distance that you don’t have here. And that’s good for you but, wow, some days it’s really hard,” Dr. Patterson said. “This is the same hospital you go to, right? I had my baby here. My husband has been a patient in our ED. My dad has been admitted here. I think this place is really challenging for that because it’s your community, you know, there’s no separation here.”
Baylis and Dr. Patterson said while that challenge exists, they are proud to serve in the same community they call home. What’s not lost on either of them: that solutions they are working to find in support of the communities they serve also directly impact their own family and friends — and light the path for ED teams to follow.
Resources
Like many health care organizations across the nation, ECU Health is facing an immense challenge: solving the growing health care workforce shortage.
Through community partnerships, the health system is doing its part to grow its workforce, starting right here in eastern North Carolina.
More than 200 high school students from Pitt County, Duplin County and other surrounding communities spent the day learning about various rural health care career opportunities at ECU Health’s Health Sciences Academy career fair Tuesday, March 5.
The event featured 30 hospital departments and exhibitors from partners including Pitt Community College and Beaufort County Community College hosted interactive and creative booths to educate students on different health care careers.

“It is such a joy to host these students and to expose them to so many interesting and important health care career opportunities available to them right here in eastern North Carolina,” said Nancy Turner, workforce development program coordinator, ECU Health. “Our students are our future workforce at ECU Health and partnerships like this are essential to ensuring we can care for our region. There are so many exciting and fulfilling opportunities to make a difference right here in their community, and we hope that today served as inspiration for them as they make important decisions about their future.”
The career fair is another representation of ECU Health’s commitment to growing health care talent locally. Through the Health Sciences Academy, ECU Health partners with public schools to provide eastern North Carolina’s youth with the education and resources to pursue exciting and fulfilling futures in health care. During high school, Health Sciences Academy students complete a minimum of six courses that expose them to potential health care careers and prepare students to pursue college-level health science programs upon graduation. They participate in job shadowing, mentoring, internships, medical research opportunities, career exploration and volunteering.
The Pitt County Health Sciences Academy is a partnership between ECU Health, Pitt County Schools, Pitt Community College, East Carolina University, the Brody School of Medicine, Colleges of Allied Health Sciences, Engineering and Nursing at East Carolina University, School of Dental Medicine at East Carolina University, the Eastern Area Health Education Center and the Greenville-Pitt County Chamber of Commerce.
Resources




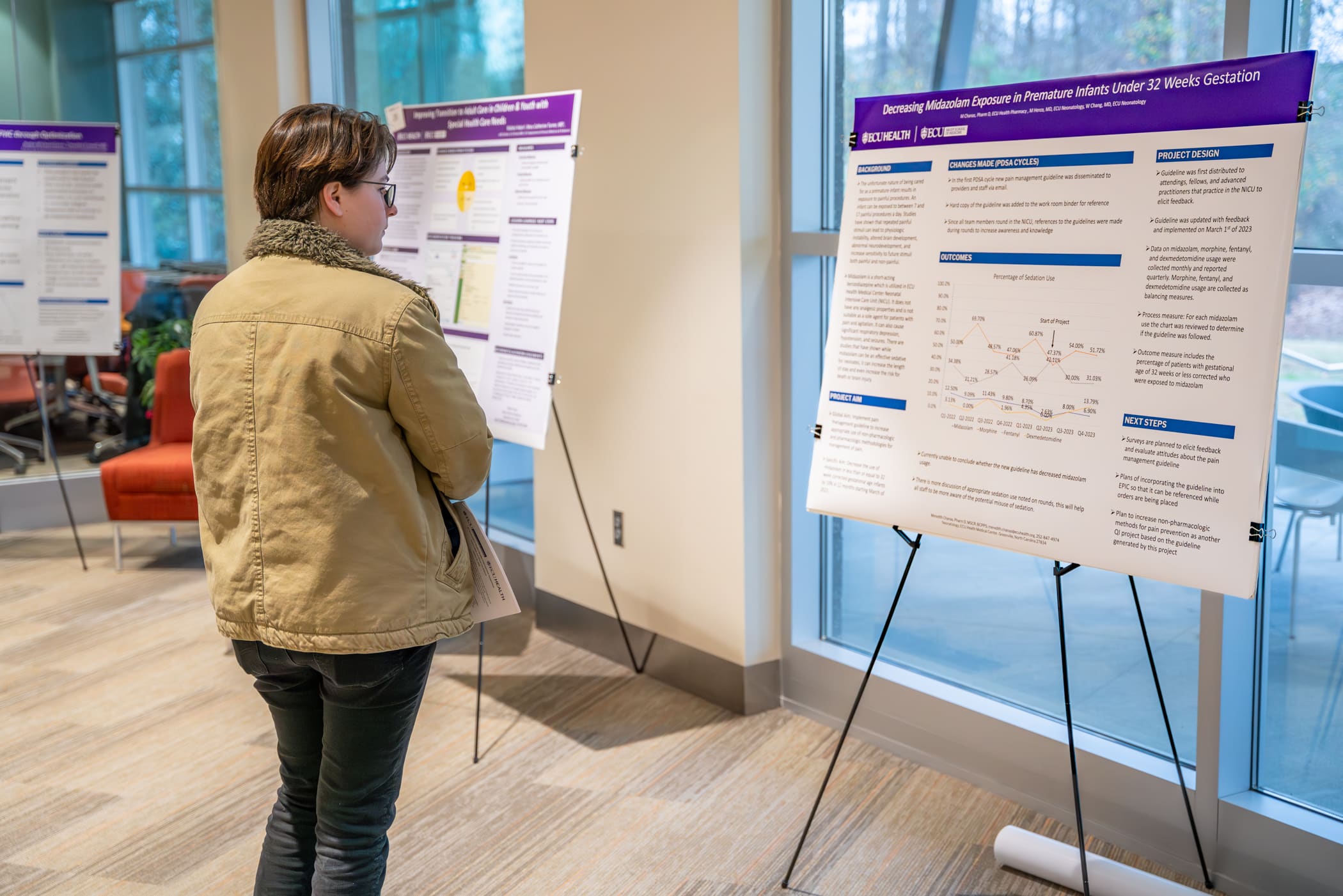
Each year, the ECU Health Quality Improvement Symposium brings together a diverse group of academic and community physicians, health professionals, health care teams, residents, fellows and students from the Brody School of Medicine at East Carolina University to present their work to an audience of peers and health system leaders.
On Wednesday, Jan. 31, ECU Health and ECU’s Brody School of Medicine hosted the eighth annual event at Eastern AHEC. This year’s event was held in-person and virtually, and showcased more than 40 projects related to quality improvement, patient safety, population health and interprofessional practice.
The day kicked off with opening remarks from Dr. Mike Waldrum, CEO of ECU Health and Dean of Brody School of Medicine. After welcoming attendees to the event, Dr. Waldrum expressed his pride in the symposium’s contributions, highlighting the collaborative efforts of teams in addressing regional challenges.

“When I look at these posters and our presenters, I see multidisciplinary, diverse teams coming together to educate, engage in dialogue and drive quality improvement for ECU Health and the patients we serve. I am incredibly proud of our team members and students for their commitment to addressing the immense challenges we face as a region,” Dr. Waldrum said.
Following the opening remarks, selected presenters who were chosen from an application process that took place in late-2023, shared their work with the audience of 178 in-person and virtual attendees.
Presentations were categorized into podium presentations, poster presentations, and works-in-progress poster presentations. Awards for the top three podium and poster presentations were announced in the early afternoon.
PODIUM PRESENTATION:
- Outstanding podium presentation: Erin Atwood, MD, MEd, Department of Pediatrics, Division of Endocrinology, Brody School of Medicine, “Increasing Counseling about the Risk of Hypoglycemia Associated with Alcohol Consumption and Insulin use for Adolescent Patients with Diabetes at the ECU Health Pediatric Diabetes Clinic”
- Honorable mention: Jennifer Stahl, MD, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Brody School of Medicine, “Right Care at the Right Location: Tele ICU Project”
- Honorable mention: Benjamin Copeland, MD, Department of Pediatrics, Brody School of Medicine, “Improving Mental Health Access for Children in Foster Care in Eastern North Carolina”
QUICK SHOT PODIUM PRESENTATION:
- Outstanding quick shot podium presentation: Juan Guillen-Hernandez, MD, Department of Pediatrics, Brody School of Medicine, “Reducing Unplanned Extubations in the Neonatal Intensive Care Unit”
- Honorable mention: Juli Forbes, MSN, RN, ECU Health Beaufort Hospital, a Campus of ECU Health Medical Center, “Improving Efficiency and Staff Satisfaction in the Operating Room Through a Revised Block Scheduling Framework at a Rural Community Hospital”
- Honorable mention: Titilola Babatunde, BS, MS4, LINC Scholar, Brody School of Medicine, “Improving Documentation of a Pediatric Early Warning Score in the Electronic Health Record”
- Honorable mention: Kate Knowles, MSN, RN, CNL, Management, ECU Health Duplin, “Back to the Basics: Hand Hygiene”
POSTER PRESENTATION:
- First place: John “JC” Rowe IV, MD, Department of Obstetrics and Gynecology, Brody School of Medicine, “Optimizing Outcomes for Patients with First Trimester Bleeding”
- Second place: Gabriella Boccia, MHA, Administrative Fellow, ECU Health, “Improving Sick Visit Clinic Access at ECU Health Physicians Adult and Pediatric Health Care”
- Third place: Stephanie Smith, MSN, RN, ACM-RN, Maynard Children’s Hospital, ECU Health Medical Center, “Improving Fall Risk Identification in Pediatric Patients”
With a total of 15 podium presentations and 29 poster presentations, symposium attendees gained insights into a variety of Quality-related projects. Dr. Waldrum emphasized the importance of what these presentations can offer.
“These presentations cover complex health care problems and this symposium enables us to think deeply about how we can tackle important issues facing our region,” Dr. Waldrum said. “It is always gratifying to see our team members and students come together to demonstrate their expertise and showcase the passion they have for the work they do.”
The symposium closed with two concurrent education sessions led by ECU Health team members:
- Patient Safety, Reliability Science and Root Cause Analysis Application presented by Susan Ingram, MSN, RN CPHQ, Director of Patient Safety
- Fostering Psychological Safety for Team and Quality Outcomes presented by Randy Cobb, DSL, ACC, CPCC, Director of Organizational and Leadership Development
To learn more about the symposium and view a list of presentations, click here.
Dr. Niti Singh Armistead, the chief quality officer and chief clinical officer at ECU Health in Greenville, keeps making the right career choices.
In college at George Mason University, she switched her major from engineering to physics and pre-medicine after she discovered that there were loans available to pay for medical school. “I appreciate what programmers do every day, but I realized that my own joy was working in the medical field,” she says.
After graduating from the University of Maryland School of Medicine, she specialized in anesthesiology, thinking her physics background would be helpful. She switched to internal medicine because she found the long-term relationships with patients more enduring and satisfying.
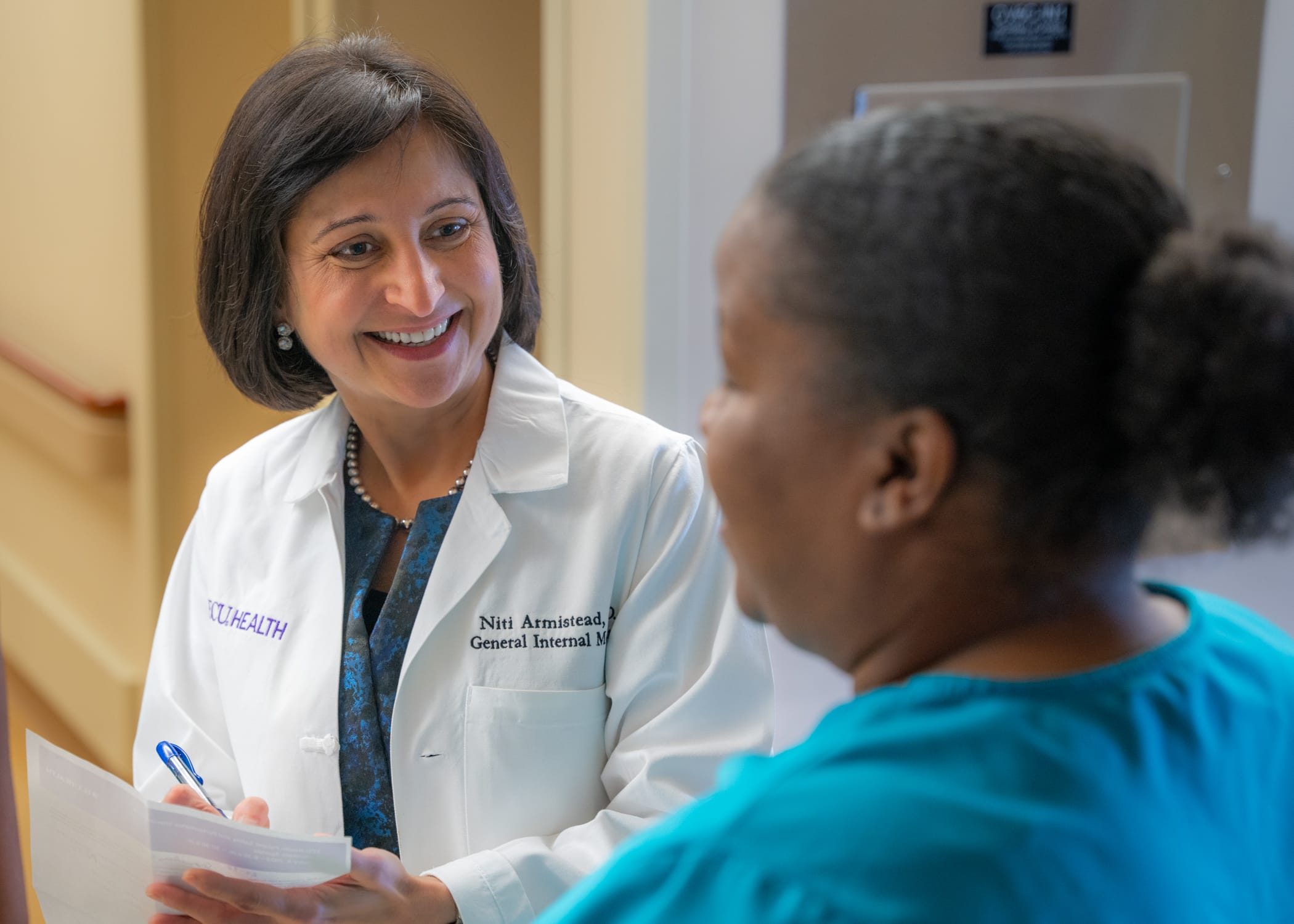
Now, at ECU Health, she’s focused on acute care and still sees patients on a regular basis. She took on administrative roles in 2018 and 2019 before the start of the COVID-19 pandemic, successfully helping steer the healthcare system during a challenging time.
“None of us knew what we were in for,” says Armistead. “For me, it all just kind of came together. How do you support an already underserved population? How do you rise to the occasion as the only healthcare system east of I-95 with an academic arm to do it all, to build the infrastructure for the testing and to educate the community? Those were the kind of interventions I got to lead.”
Read the full story in Business North Carolina.
ECU’s clinical laboratory science students — who after graduation run the nation’s medical labs in hospitals, for public health offices and in the pharmaceutical and biotech industry — got a huge boost recently with the acquisition of a new device that automates the process for identifying blood types.
Funding for the new system, some $6,600, came in part from the American Society for Clinical Pathology and the ECU Medical and Health Science Foundation’s CLS Priority fund.
The instrument, known as the Ortho Clinical Diagnostics workstation, replaces a laborious process of mixing blood samples with reagents by hand to allow laboratory professionals to quickly and accurately establish blood types and identify donated blood that can be safely transfused to a recipient.

Traditional blood analysis methods, which ECU’s Department of Clinical Laboratory Science chair Dr. Guyla Evans and her faculty peers still teach their students, involves mixing drops of blood with antibodies that register specific blood types. The process also registers Rh factor, proteins on the surface of some people’s blood cells that affect who can receive blood donations from whom.
Using the established test tube method is a time and attention intensive process.
“It can be kind of hard to teach students how to read the tubes because it’s subjective. You have to read the tubes right away, and there are a lot of steps,” said Michael Foster, a senior from Roanoke Rapids, who already works in the blood bank at ECU Health Medical Center in Greenville.
Using test tubes to identify blood samples is a tricky business: laboratory personnel must identify cell reactions by eye and they have a limited time to observe and interpret the results.
“The name of the game in blood banking is accuracy, but it’s also speed. You want to get it in the centrifuge and as soon as it’s ready to come out of the incubator and get it going,” Evans said.
The new system uses a cartridge, which requires less blood in the sampling process and has the advantage of leaving the sample readable by technicians for up to 24 hours. This allows laboratorians to double check their work or have a peer review their results.
An added benefit for the cartridge system is baked-in surety of the testing chemicals.
“You don’t have to worry about adding the wrong reagents because the cards are color-coded and the reagents are already added in,” Foster said.
Each cartridge may cost up to $25, which isn’t cheap, but Evans and Lorie Schwartz, a research technician and CLS instructor, both agree that the new system is at least as cost effective as traditional testing methods due to labor costs and the intangible benefit of assurance that the results are valid.
The new system is less mentally taxing for the medical laboratory scientist, Evans explained.
“In the blood bank, everything has to be carefully documented. Nothing is ever assumed or taken for granted—blood bankers trust no one, they believe no one,” Evans said. “If I’m going to do a cross match for two units, and the antibody screen and the blood typing, that’s 12 to 15 tubes that I have to label every time. It’s a lot faster to label one card or a couple of cards, depending on what testing you’re doing.”
The CLS department received the equipment in December, just a bit too late for the current class of students, including Foster, who will graduate in May. The seven graduating students were able to train on the gel microcolumn system during clinical rotations with ECU Health and Nash UNC Health, where they got hands-on experience.
Evans said the COVID-19 pandemic made teaching blood banking techniques very difficult because, while theory is crucial to understanding lab work, getting hands-on training is critical for learning.
Students who learned during the pandemic were dropped into the deep end during clinical rotations in working labs and had to put theory into practice, both with traditional test tube methods and the gel cartridge system.
“During clinicals, we went through quite a number of cards trying to figure out what antibodies were present in the blood because they would give us unknown samples and we would spend the entire eight hours trying to figure out what the sample was,” said Bryce Glover, a senior from Fayetteville. “If we went down the wrong path, that was one card wasted.”

Because they are eligible to work in clinical labs once their clinical rotations were completed, Foster, Glover and the other members of their cohort already have jobs in area labs.
“ECU Health and ECU’s commitment to incorporating the latest technologies into both health care delivery and hands-on training for our future workforce not only benefits students during their academic journey but also equips them with valuable skills that are highly sought after in the health care industry,” said Carolyn Merritt, ECU Health lab scientist.
“Keeping students up to date on the latest technologies, such as gel testing, is crucial for optimizing their limited time during clinical rotations. Our goal is to help prepare the next generation of high-quality health care professionals, and hands-on experience with innovative technology ensures our students are well equipped to provide important services once they enter the workforce,” Merritt said.
The advances in high tech equipment, combined with severe staffing shortages, have exacerbated what Evans sees a worrying trend — laboratory professionals aren’t seen on the hospital floors or interacting with nursing staff.
Being squirreled away in a windowless lab the majority of the workday means that medical laboratory scientists and technicians are often disconnected from their peers. Evans counsels her students to be part of the hospital and medical communities they will eventually be part of.
“They must make an effort to be seen as part of the hospital team because they usually aren’t seen,” Evans said.
While medical laboratory scientists might not be as visible as other members of the health care continuum, their role in diagnosing and treating patients can’t be overstated. With an expected need of nearly 17,000 more medical lab scientists nationwide by 2032, the critical skill set that Pirate graduates bring to hospitals and clinics is invaluable.
“When our students get into the clinical system, that’s when they really see the workflow and that last piece of their education comes together,” Evans said. “We’ve been really fortunate that our clinical sites, even though they know they’re dealing with personnel shortages, are taking students on which is extra work they don’t get compensated for. They’re doing it because they know it’s important and that is invaluable.”
Sharon and Steve McNally of New Bern have been married for more than 40 years. Now, Steve carries a little piece of his wife Sharon with him everywhere he goes.
Steve is diabetic and in 2015, he went through his first round of transplants at a hospital in their then-home state of Pennsylvania.
“It was supposed to have been a kidney and pancreas at the same time,” Steve said. “When they got me on the operating table, the pancreas wasn’t viable. So they said, ‘We’re going to do the kidney alone and we’ll get you a pancreas.’ What happened then was the hospital eventually became decertified and couldn’t do pancreas transplants anymore.”
Then, they joined the transplant list with a health system in Maryland and Steve received a pancreas transplant 30 days later. In the meantime, the new kidney had been damaged due to the lack of a functioning pancreas, but Steve said it was largely working fine until mid-2023. By that time, the McNallys had moved from Pennsylvania down to New Bern.
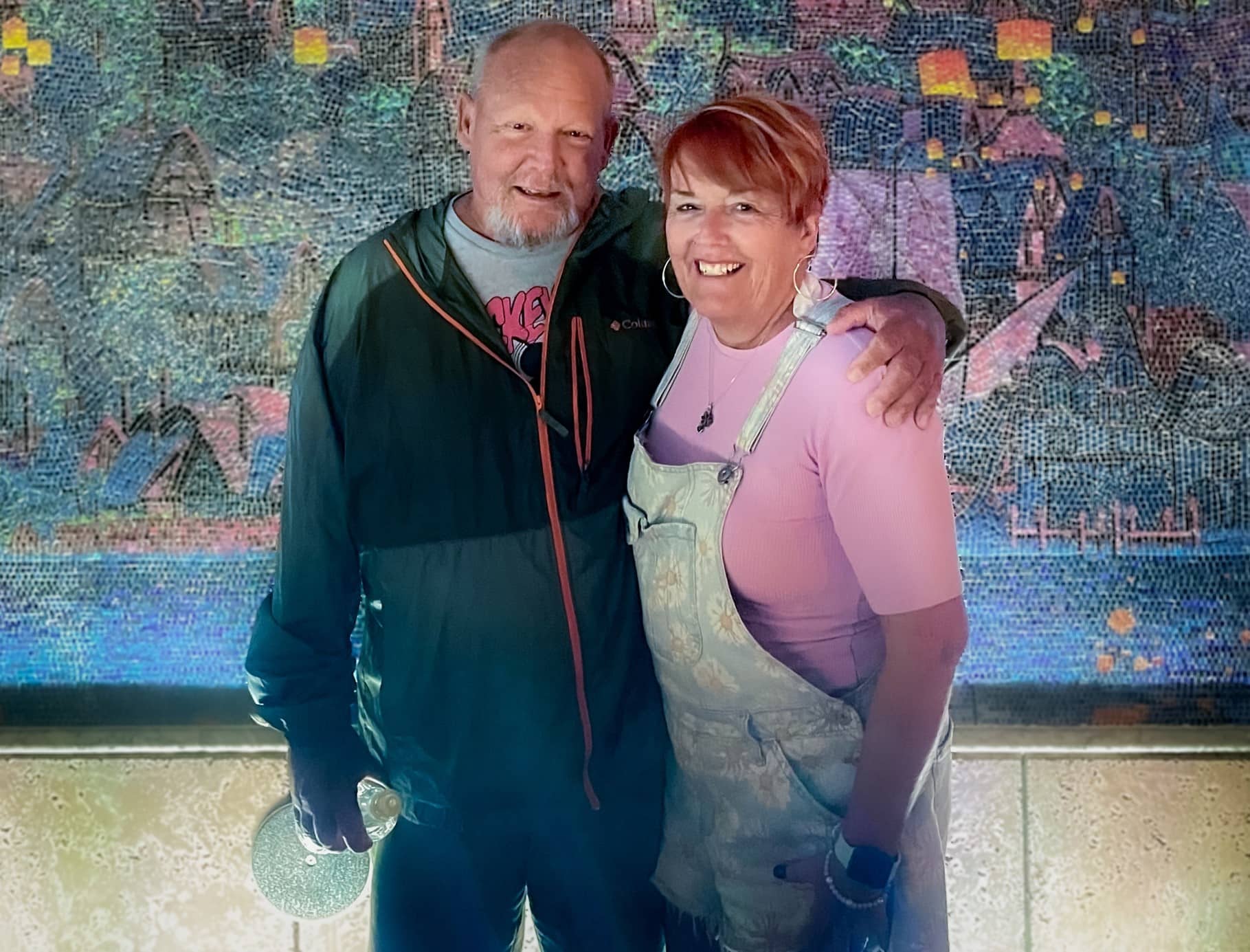
With Steve’s kidney function worsening, there was little time to spare. He could join another transplant list that may take eight to 10 years to find a donor, start dialysis or personally find a match to donate a kidney.
Sharon said she knew she had to step up for her husband and get tested to see if she could be a match.
“It wasn’t really hard for me because a lot of people say, ‘Oh my gosh, you’re so amazing’ or so this and that but I don’t really feel that way,” Sharon said. “I feel like we’ve been married 40 plus years. We have grandkids and kids together and how could you watch someone get more and more ill and not do something if you can? So I didn’t really think about it.”
Testing started for the two in June and preparation began right away. They found out in October they were a match and an ECU Health team performed the transplant on Nov. 7.
“I’m glad that this was something I could do,” Sharon said. “There’s a lot of people that probably couldn’t have, even if they wanted to.”
For Sharon’s part, she went home the next day while Steve stayed a couple extra days for monitoring before heading home. While they each needed some help early on after coming home, they were both happy to support each other, as they’ve been doing for more than four decades.
Dr. Margaret Romine, transplant surgeon at ECU Health, and Dr. David Leeser performed the transplant along with other members of the ECU Health transplant team. She said she was most proud that the team could take on a case like the McNallys, especially given Steve had been through a kidney and pancreas transplant previously.
“They had already been through a lot before even coming to us but they had such great attitudes and were great patients to care for,” Dr. Romine said. “We have such a great team and that really sets us apart from other programs. It’s not just about what the surgeon thinks – the nephrologists play a huge role. Our coordinators, nurses, pharmacists, social workers all play a huge role. We can’t do what we do without the entire team. Whenever we make a big decision to take on a patient like him, it’s done as a team.”
Steve and Sharon both said they were happy with their experience at ECU Health and shared appreciation for the care team that helped guide them through the process and into recovery.
Now, they are looking forward to a spring working outdoors, something they both love but missed out on last year.
Sharon said if she could share one message, it would be on the importance of organ donation.
“Organ donation is just such a wonderful thing. I mean, three different times it saved my husband,” Sharon said. “You know, a lot of people don’t want to do something like that even after they’re gone because it just it seems weird to them. But honestly, I think it’s a wonderful thing.”
NAGS HEAD, N.C. — Jan. 30, 2024 — Outer Banks Health is proud to announce the opening of the Carol S. and Edward D. Cowell, Jr. Cancer Center, a 15,000 square-foot, state-of-the-art facility made possible through the collaboration of Outer Banks Health, ECU Health, Chesapeake Regional Healthcare and the generous support of the Outer Banks community. The center opened its doors to patients on January 29, 2024.
This momentous occasion marks the culmination of years of dedication, perseverance, and community support. Outer Banks Health initiated the endeavor in 2015 with a vision to create a cutting-edge facility that would serve as a beacon of hope and healing for cancer patients on the Outer Banks and the surrounding region.
“The completion of the Cowell Cancer Center was made possible through the unwavering determination of the Outer Banks Health Development Council,” said Ronnie Sloan, FACHE, president of Outer Banks Health. “The council is comprised of dedicated individuals who share a passion for enhancing healthcare in the region and it played a pivotal role in bringing this ambitious project to fruition.”

Led by radiation oncologist, Charles Shelton, the new center boasts a dedicated team, including a director, radiation therapists, a radiation nurse, a genetics extender, a physicist, a dosimetrist, pharmacists and pharmacy technicians, LPNs and RNs, lab technicians, navigators, a social worker, a practice manager, and patient access representatives. While the search for a permanent medical oncologist continues, Dr. Michael Spiritos, formerly of Duke Health, has agreed to serve in that capacity on an interim basis along with Dr. John Barton. Katie Caton, FNP is also on staff as a permanent provider.
Of the 1300 critical access hospitals nationwide, Outer Banks Health Hospital is one of only eight accredited by the Commission on Cancer of the American College of Surgeons and is also distinguished as the only one in the country with an accredited breast program. This notable achievement reflects the commitment of Outer Banks Health to maintaining the highest standards of cancer care.
Outer Banks Health remains focused on expanding its list of services and programs to meet the evolving healthcare needs of the community. The organization’s goals include delivering excellent care locally and collaborating with health organizations throughout North Carolina and Virginia to ensure residents and visitors can access the best possible care.
For more information about the Cowell Cancer Center or to inquire about services, visit OuterBanksHealth.org/services/cancer-care or call (252) 449-7272.
Greenville, NC — Yaolin Zhou, MD, associate professor of Pathology and Laboratory Medicine at the Brody School of Medicine at East Carolina University, director of Quality and Test Utilization, and head of Molecular Pathology at ECU Health, was named to the 2023 Becker’s Hospital Review “Emerging Leaders: Provider Organization Leaders Under 40” list.
The Becker’s Hospital Review list recognizes up-and-coming leaders who are quickly rising through the ranks at their organizations, focusing on development, innovation, and improved outcomes.
The “Emerging Leaders: Provider Organization Leaders Under 40” list honors leaders who are 40 years old or younger for their commitment to optimizing health care. The Becker’s Hospital Review editorial team accepted nominations for this list and curated it to highlight the accomplishments of these rising stars.
Dr. Zhou trained at some of the most prestigious institutions in the world and chose to come to ECU Health to help address some of the most challenging problems in health care delivery. As the only molecular pathologist in ECU Health’s 29-county service area, she provides expertise that benefits more than 1.4 million individuals in the region.
“ECU Health is proud to have Dr. Zhou, a nationally recognized molecular test utilization expert, whose work exemplifies the vital connection between research, education and effective health care delivery,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine. “Dr. Zhou’s expertise shapes innovative clinical solutions, addressing unique barriers in rural populations. I am grateful for leaders like Dr. Zhou who are helping to create a healthier present and future for eastern North Carolina.”
Since her arrival in 2020, Dr. Zhou established an innovative molecular consultation service, focused primarily on pre- and post-testing review, to ensure cancer patients receive appropriate molecular tests and treatment. In 2023, she secured a $250,000 industry-funded quality improvement grant to expand her molecular consultation services across practices in eastern North Carolina’s rural 29-county region. This grant aims to identify and address health care disparities in cancer care, ultimately improving patient outcomes.
In addition to her molecular expertise, Dr. Zhou is an internationally recognized quality improvement and test utilization expert. In 2020, she partnered with clinical colleagues to establish a health system-wide initiative to reduce daily repeat lab tests, achieving a 15 to 25 percent reduction in unnecessary repeat daily testing throughout the system. For this multi-specialty and multi-disciplinary collaboration, Dr. Zhou and her team were honored with the prestigious American Society for Clinical Pathology Choosing Wisely Champion Award.
Dr. Zhou is active as a teaching and clinical faculty member and a bioethics and quality improvement instructor at Brody and for ECU Health. She also represents eastern North Carolina on the board of directors for the Association for Molecular Pathology (AMP), the world’s largest association for molecular professionals. Dr. Zhou recently authored an invited guest editorial in the Journal of Molecular Diagnostics, the official AMP journal. This editorial, based on her grant work, presents a national solution to reduce barriers in precision oncology.
“As a cancer survivor myself, I strive to bring quality and equitable cancer care to those I am honored to serve,” said Dr. Zhou. “All patients deserve high-quality and guideline-recommended cancer treatment. Through this recognition, I hope we can bring greater visibility to how we are addressing disparities in cancer care in our patients. Through collaborative efforts, we can develop solutions for providing equitable cancer care on a broader scale – and it starts here in eastern North Carolina.”