In honor of Dr. Martin Luther King Jr. Day, community leaders, elected officials and eastern North Carolina residents came together for the 27th annual Community Unity Breakfast, hosted by the Greenville-Pitt County Chamber of Commerce on Monday.
The event brings together the community to reflect upon the life and legacy of Dr. Martin Luther King Jr. while celebrating and expanding diversity initiatives in Greenville and Pitt County.
As a sponsor of the event, ECU Health had an opportunity to present a speaker during the event. Brian Floyd, chief operating officer of ECU Health and president of ECU Health Medical Center, represented the system and shared a few words.
Floyd said that events like this are closely aligned with ECU Health’s mission to improve the health and well-being of eastern North Carolina because it focuses on bringing everyone together and supporting those around you.

“Your well-being is attached to much more than your clinical and scientific makeup,” Floyd said. “You can’t be well if you’re socially isolated. You can’t be well if you don’t have the means to support yourself and your family. You really can’t be well if you have no way to help those around you. So our mission, as complicated as it is, is to make people and communities better. This community comes alongside us and helps us do that as well. We all can participate in what others are doing to improve our society, to improve how people come together, and work together to love and support each other.”
Floyd also highlighted his appreciation for ECU Health’s close collaboration with the Brody School of Medicine at East Carolina University, and the relationships with other colleges, universities and high schools. He said the opportunity to develop and grow talent within the system is something he is proud of as well.
All of this leads to a great financial impact on the region, Floyd said, and that can go a long way to effect positive change in the lives of residents in the East.
“We know that education is important to the fabric of society and the wellness of people and the socioeconomic conditions of eastern North Carolina require us to do something about that,” Floyd said. “We’re fortunate that we can stimulate the economy of eastern North Carolina by more than $4 billion per year. That’s not just money – it’s hope, it’s a way to get started, it’s a way to support your family. When you put all of that together, the pillars of what we’re doing for eastern North Carolina, that’s the difference we can make.”
Pastor Eve C. Rogers, senior pastor at New Dimensions Community Church, gave the keynote address for the event. Chad Tucker, director of Volunteer Services at ECU Health Medical Center, serves as co-chair of the Community Unity Planning Committee and introduced Pastor Rogers during the event.
Pastor Rogers spoke on the importance of standing up to injustices in our communities to help create a future everyone can be proud of. She said showing up for the marginalized members of our communities is a responsibility we all carry.
“As we run and purse this race of life, liberty and the pursuit of happiness, I provoke you to show up with soul-force,” Pastor Rogers said. “Exercise and put into plan the opportunity that God gives you, day after day, season after season, time after time again, to show up and do what is right, fair and equitable.”


Dr. Audy Whitman is an eastern North Carolinian, through and through. He was born in the farming town of Seven Springs – a town of roughly 80 people – in Wayne County.
Like in many towns in eastern North Carolina, its citizens struggle with poverty and access to health care. It is there, in Seven Springs, where Dr. Whitman’s rural upbringing helped him discover a love for medicine that influences his work today.
Today, Dr. Whitman is a family medicine physician for ECU Health and clinical assistant professor at the Brody School of Medicine at East Carolina University, but back in Seven Springs, he was a helping hand in the tobacco fields, braving the eastern North Carolina heat and humidity.
“There is no more powerful motivator in the universe, in my humble opinion, than standing in the middle of a tobacco field in the late summer with 99 percent humidity, no shade and it’s 100 degrees outside,” Dr. Whitman said. “Your hands are caked with tobacco gum. The nicotine is soaking through your skin, so you feel nauseous all the time. Those long days taught me a great work ethic but they were also powerful motivators.”
Rural health care realities
Americans who live in rural areas make up 20% of the United States population and residents in these areas face a myriad of challenges: shorter life expectancy, higher mortality, higher rates of poverty, fewer local doctors and greater distances to travel to see health care providers. Only 10% of U.S. physicians currently practice in rural areas.
Physician shortages are no secret across the country, with the Association of American Medical Colleges estimating a shortage of up to 124,000 physicians by 2034, and rural areas are at an even greater risk.
The Brody School of Medicine was founded over 40 years ago to train primary care physicians to provide care for rural eastern North Carolina. These challenges inform the medical school’s mission and its proven track record is best represented by the fact that Brody is No. 1 in North Carolina and No. 2 in the United States in the percent of graduates in the last decade who chose careers in family medicine.
Programs like the Rural Family Medicine Residency Program take that work a step further by focusing on initiatives that help place providers in rural areas. Studies show that family medicine residents who spent 50% or more of their training time in rural settings were at least five times more likely than residents with no rural training to practice in a rural setting.

“Rural health care is under duress, and our rural communities need solutions,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine. “The Rural Family Medicine Residency Program is another great example of ECU Health and Brody understanding what the community needs are and creating new pathways to educate physicians to meet the community’s needs and improve the health and well-being of those communities.”
Setting a path forward
After Dr. Whitman was approached to create and administer the program, things moved quickly. A “national guru for all things family medicine” made a visit to eastern North Carolina to consider the best locations for residents to begin their rural training. Dr. Whitman and team reached out to other universities and health systems with established programs and traveled to learn about rural organization structure and rural curriculum best practices. Two years later, the Rural Family Medicine Residency Program had its first cohort ready for training.
The first year of the program features training at ECU Health Medical Center, a Level I Trauma Center, and helps set the residents up for success when they get to the rural environments in their second year.
“Anything and everything you can imagine seeing in residency training, you’re going to see at the medical center,” Dr. Whitman said. “We provide this very intense, inpatient-heavy first-year experience for these rural residents where they get to see really sick, really complicated patients with lots of resources at their disposal so they can learn how to take care of these really complicated patients. After their first year of training, when they’ve taken all of these lessons learned, they can go out into these rural communities and apply those lessons learned where they’re the only show in town.”
Dr. Whitman added that while Greenville and eastern North Carolina are rural, the more than 1.4 million patients served through the ECU Health system creates a high volume of patients at ECU Health Medical Center, and the exposure to so many patients during their training is also hugely beneficial for the rural residents.
“An institution like ECU Health boasts a 974 bed, Level I academic medical center where residents train alongside some of the best and brightest health care minds in the state,” said Dr. Jason Higginson, executive dean at Brody. “Medical residents can then serve in our more rural hospitals to apply that knowledge to underserved populations, building a connection to the community in which they serve and making a real difference in the lives of patients.”

Dr. Zeel Shah
Drs. Zeel Shah and Jim Jaralene Porquez were part of the inaugural cohort for rural family medicine residents. Dr. Shah practiced and trained at Roanoke-Chowan Community Health Center in Ahoskie and Dr. Porquez at Goshen Medical Center in Beulaville, both of which are Federally Qualified Health Centers (FQHC) that serve at-risk and underserved rural populations. The mission and vision of these FQHC organizations align with the mission and vision of ECU Health. Together, they seek to augment scarce health care resources in rural communities, improve the health metrics of the communities they serve, and encourage the residents that train in these rural communities to establish roots and continue serving these rural communities after graduation from their residency training program.
Dr. Shah said the year in Greenville was a great experience before continuing her residency training with a focus on serving the rural community of Ahoskie.
“In Greenville you have a lot of resources, but it’s a learning curve to rotate through the different specialties,” Dr. Shah said. “In Ahoskie, the challenges are different. Social determinants of health care, such as finances and distance, play a significant role, and you don’t have the same resources. You learn quite a lot about how to make your limited resources go a long way by relying on creative strategies while using medical expertise you picked up in Greenville.”
Now, as graduates of the program and full-time physicians with ECU Health, Drs. Shah and Porquez feel established in their respective communities and have built trusting relationships with patients, families and fellow team members. Both said the community aspect and truly knowing their patients are among the most rewarding parts of their rural experience. For Dr. Porquez, feeling love, trust and appreciation from her patients has made her time in Duplin County special and a place that she plans to call home after her residency.
“What really drew me into my community clinic in Duplin County specifically, is that my patients are very appreciative of what I do for them,” Dr. Porquez said. “They care so much about my time, my effort and my expertise, and I think in just a couple of years I have built that strong trust and relationship with them. I feel like I don’t just treat them with their disease, but I go further than that. I treat them as a whole, and I get to know their whole well-being. I see them as a whole person and not just the disease that I treat.”
Early milestones

Dr. Jim Jaralene Porquez
For Drs. Shah and Porquez, the personal connections built through the program are so strong that both decided to practice in eastern North Carolina following the completion of the program in 2024. Their graduation, along with the other residents in the first cohort, represent a significant milestone in the program’s short history and help ensure rural communities have access to specially trained, high-quality rural family medicine providers.
Dr. Whitman said he’s proud to see two members of the first cohort choose to stay and make a difference in communities like the one in which he was raised. The successful launch enabled the team to think bigger, and the program now features a new site in Halifax County with an expanded class size of nine residents. The program in general will grow from its original size of 10 residents to a total of 27 residents by 2026.
“Moving forward, I see nothing but growth for us,” Dr. Whitman said. “We are truly doing mission-driven work and trying to bridge the chasm of health care disparities of urban centers and rural areas here in North Carolina.”
Dr. Waldrum agreed and said he sees the program as the beginning of something special for eastern North Carolina and rural medicine.
“My hope is that we can take the knowledge gained through the Rural Family Medicine Residency Program and apply those lessons towards other specialized clinical areas of expertise in the near future,” Dr. Waldrum said. “We are proving that we can be highly successful in creating rural residency tracks and our historic success training rural providers who go on to practice here in North Carolina is a further testament of our ability to create unique solutions that meet the needs of those we serve.”
Resources
Lung cancer is the leading cause of cancer-related death in the United States and is the second most common cancer in both men and women. In eastern North Carolina, where risk factors for the disease are higher than most other areas in the country, screenings are helping save lives.
“We’ve known since the 1990s that using CT scans at a very low dose can actually save lives,” Dr. Mark Bowling, a pulmonologist at ECU Health Medical Center, said. “Now you can do low dose lung cancer screenings once a year if you meet certain criteria.”
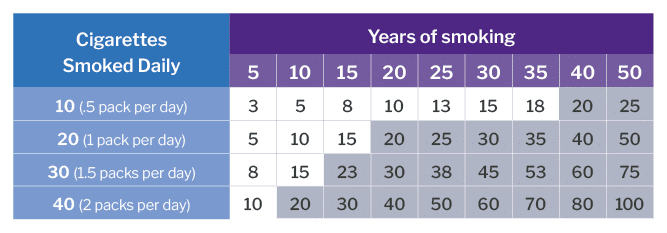
The criteria includes: being between the ages of 50 and 80, having a 20-pack smoking year history – which equals a pack a day for 20 years or two packs a day for 10 years – and having no signs or symptoms of lung cancer.
While low dose CT scans are always available across the system for the insured, a grant program allows ECU Health to offer a once-a-month clinic in Greenville for the uninsured who meet the criteria and have received a referral from their provider.
Jennifer Lewis, Cancer Center outreach coordinator at ECU Health Medical Center, helps run the clinic. She said raising awareness for lung cancer screenings is crucial and can lead to early detection.

“We’re all aware of mammograms for breast cancer screening and colonoscopies for colon cancer, but not a lot of people realize that there’s a screening for lung cancer,” Lewis said. “If we do find something abnormal, we want to find it in its early stages when the outcomes are better, when there are more options for treatment. With lung cancer being a leading cause of cancer-related death, by the time someone starts manifesting lung cancer symptoms, it’s typically very advanced at that time. You have fewer options and your outcomes aren’t positive so our goal is to find cancer before someone begins to have symptoms.”
Lung cancer symptoms are often non-specific, including shortness of breath, coughing up blood, chest pain and inability to move arms among others.
Lewis said she is also passionate about advocating for patients and helping to eliminate stigmas around any cancer, particularly lung cancer.
“We’re here to let people know, if you smoked, if you still smoke, that doesn’t define who you are as a person. We just want to get you screened,” Lewis said. “We’re not here to judge whether or not you smoke. We’re not here to berate you. We will ask if you’ve been educated about smoking cessation, but that’s not why you’re here. We try to make people feel comfortable and feel valued. Your family still loves you and they still want you around so let’s get you screened and make sure you don’t have anything going on that we need to worry about before it becomes a problem.”
Courtney Johnson, Thoracic Oncology Program coordinator at ECU Health Medical Center, has been with the system for 10 years. First, she worked as an inpatient cancer care nurse in the Eddie and Jo Allison Smith Tower at ECU Health Medical Center for about four years and she said it was a rewarding and special time for her.
That led her to her current role in which she helps track and manage at-risk patients through the screening process. She said the best part of her current job is playing a part in early detection.
Recently, she said her team caught cancer in a patient they’d been taking through screenings for about five years. The screenings showed a change in known nodules for the patient and they were sent to surgery to have the cancer removed. Since it was caught in the extremely early stages, the patient did not have any need for chemotherapy and they’ll just have to follow up with future scans for the patient.
“That’s the greatest thing in this position –I can’t prevent everything, I cannot predict outcomes, I can’t prevent what could be the inevitable, but I have a hand in hopefully early intervention,” Johnson said. “I enjoy spending more time with the preventative side of medicine and hopefully allowing our patients to stay out of the hospital. Instead, they come in and we can be proactive with this rather than having to scramble when the patient is in an advanced stage.”
Johnson also shared that radon exposure is a risk factor for lung cancer. She said radon testing kits are available through North Carolina Department of Health and Human Services.
Resources
Each Halloween, patients, families and team members at Maynard Children’s Hospital at ECU Health Medical Center get a chance to break away and enjoy the holiday.
Parade floats from team members and community groups flowed by the Children’s Hospital on Halloween afternoon, giving the children a chance to see some of their favorite characters, like Barbie and Ken, Minions, and floats from Toy Story, Trolls and Encanto. Even the Mystery Machine, a Jeep full of sharks and a pirate ship appeared – all to help make the day a little brighter for the youngest patients at ECU Health Medical Center.
Amanda Jones, a child life specialist at Maynard Children’s Hospital, said there is always a lot of planning that goes into the event, but it’s worth it each year to give the children something to look forward to during the holiday.
“This is a really fun event where they can still celebrate Halloween even while they’re here at the hospital,” Jones said. “It allows kids to be kinds while they’re in the hospital. It’s something that they would normally be doing if they weren’t in the hospital so it kind of brings a little bit of that holiday spirit to the event here.”

For parents, it can also bring a source of comfort. Angela Blanton’s 8-year-old son, Chance, is a patient at the Maynard Children’s Hospital and has a rare condition called Walker-Warburg Syndrome. Blanton said Chance could not be outside for the event, but she still wanted to celebrate Halloween – her son’s favorite holiday – while at the hospital.
She shared photos of past Halloween costume contests he had won and reflected on what this event meant for her. She wore an inflatable chicken costume, worn earlier this month at a Halloween party with her son dressed as Colonel Sanders.
“He would love to be down here, but he can’t be. So I think it’s amazing for the all the children that can be here,” Blanton said. “Seeing them light up, and even me, in this silly costume. Some of the kids wanted to take a picture with me, and I thought that was awesome. To see the smiles from the kids and parents and know how important it is for everyone. Not just the children, but the moms who have been there by the bedside.”
She shared that these events mean a great deal to the patients and families looking for a piece of normalcy in a challenging time.
Patients across the hospital receive goodie bags with art supplies and toys after the event, whether or not they could come. Jones said the event is important for team members
“This is a great event for team members that participate in the parade and for those that come out and watch it,” Jones said. “It’s enjoyable to be able to step away from the bedside and spend time with patients on events like this. I think it’s really uplifting for everyone.”
Ahoskie, N.C. – ECU Health Roanoke-Chowan Hospital hosted a community celebration Tuesday to proudly commemorate 75 years of dedicated service to eastern North Carolina.
Established in 1948, the hospital is dedicated to providing exceptional health care services to its community and has expanded and evolved to meet the changing health care needs of the region.
“We are immensely proud to celebrate 75 years of serving our community,” said Brian Harvill, president, ECU Health Roanoke-Chowan. “Throughout the years, we have strived to provide high-quality health care services with a patient-centered approach. Our commitment to excellence and compassionate care for our community has been the driving force behind our success and continues to positively impact those we are proud to serve.”

Situated in Ahoskie, this 114-bed hospital has been a cornerstone of health care, offering comprehensive services to nearly 40,000 residents spanning Hertford, Bertie, Northampton, and Gates counties. ECU Health Roanoke-Chowan Hospital offers a number of specialty services, including behavioral health, cancer care, pain management, wound healing, sleep services, pediatric asthma management and an ECU Health Wellness Center location in Ahoskie. The pediatric asthma program at ECU Health Roanoke-Chowan Hospital helps children in Hertford and Northampton counties miss fewer days of school, participate more fully in physical activities and look forward to a brighter future.
“Over the past 75 years, ECU Health Roanoke-Chowan has been dedicated to providing exceptional health care services, and this milestone marks a testament to its unwavering commitment to the well-being of the community it serves,” said Jay Briley, president of ECU Health Community Hospitals. “These achievements reflect the hospital’s dedication to improving the overall health and well-being of the community. Today is a day to celebrate the contributions of our current team members and those that came before them to help build a legacy of quality, compassionate care.”
Since its founding in 1948, ECU Health Roanoke-Chowan Hospital has continuously evolved to meet the changing health care needs of the community. On Oct. 24, 1948, the original 40-bed hospital celebrated with a community open house, officially welcoming patients on Nov. 1, 1948. ECU Health Roanoke-Chowan Hospital holds the distinction of being the first hospital licensed by the Medical Care Commission, still bearing license number 1, marking it as the first hospital in the nation constructed using federal funds provided by the Hill-Burton Act. In 1952, the facility expanded with the addition of its first wing, accommodating 25 additional beds, followed by another 34-bed expansion. By 1975, an extra 50 beds, 10 intensive care units and a third floor were added. In response to the growing community’s needs, the original structure was replaced, culminating in the dedication of the present-day hospital in 1992.
“As we celebrate 75 years of service, our hospital’s commitment to clinical excellence remains unwavering,” said Dr. David Lingle, chief of staff, surgeon, ECU Health Roanoke-Chowan. “Our legacy is built on a foundation of dedicated health care professionals who continuously strive to reach the highest standards of care, ensuring that every patient receives the best possible treatment, and making each year better than the last. It is an honor to serve alongside such a great team of professionals.”
ECU Health Roanoke-Chowan has achieved numerous milestones throughout its journey, including recertification as a primary stroke center by The Joint Commission and the American Heart Association/American Stroke Association, Get with the Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll and earning accreditation by the American College of Surgeons Commission on Cancer as a Community Cancer Program.


Students from the Brody School of Medicine, ECU College of Nursing, and Department of Physician Assistant Studies participated in the Interprofessional Triage and Emergency Assessment and Management (ITEAM) Day mass casualty training event hosted by the Brody School of Medicine’s Emergency Medicine Interest Group Saturday, Oct. 14. The training provides a unique opportunity for students from different health care disciplines to collaborate and gain hands-on experience in managing emergency events.
Experts from the ECU College of Nursing, Brody School of Medicine, Department of Physician Assistant Studies and ECU Health EastCare gave students interactive instruction in procedural skills, such as basic airway management, hemorrhage control and triage techniques. Students then applied these skills during a mass casualty simulation at the Interprofessional Clinical Simulation Center at the Brody School of Medicine.

“ITEAM Day was beneficial to promote collaboration and interprofessionalism among different health care providers,” said Stephiya Sabu, first year Brody School of Medicine student. “Doing this in the setting of a mass casualty event was important as they can be very stressful, and having this experience beforehand will help in the future if we are ever in that situation.”
This year’s simulation was a mass shooting incident. The Office of Clinical Skills Assessment and Education provided simulated patients, portraying symptoms and behaviors consistent with injuries sustained in a mass shooting, including confusion and panic.
Adding an extra layer of realism to the exercise, the ECU School of Theatre and Dance lent its expertise in moulage and makeup to create lifelike wounds on the simulated patients. The ECU Student Government Association provided funding for food and materials.

Students participating in the simulation were coached by a multi-disciplinary team of experts who provided feedback throughout the training. Chuck Strickland, outreach coordinator with EastCare, served as an instructor and provided invaluable insights into the role Emergency Medical Services (EMS) plays in a mass casualty incident. Students were educated on EMS’s initial response, patient management and treatment strategies.
“It is important for students to know the role EMS plays in initial patient triage and how we would request resources and determine patient destinations,” said Strickland. “EMS identifies the volume of patients and their acuity levels, then gets nurses, physicians and physician assistants to do on-scene care for high acuity patients. Students also learned the role of critical care transport and how those professionals would be engaged.”
Nursing students, medical students and physician assistant students shared their respective expertise while working together to promptly triage and treat patients. Both students and instructors underscored the significance of applying classroom learning to simulated real-life scenarios, highlighting the practical value of such experiences.
“Recent events in our community emphasize the unpredictability of mass casualties and just how terrifying they are,” said Lachlan Younce, first year Brody School of Medicine student. “As a medical student, I seek to understand my role as a medical professional in those situations. Participating in this mass casualty exercise exposed me to vital skills like patient triage, resource-efficient care and the importance of teamwork when working alongside my health care colleagues, including PAs and nurses. I am thankful for how this ITEAM training experience helped me develop my readiness as a medical professional.”
Health and well-being are at the very heart of creating economic vibrancy in a community. That is why Brian Floyd, chief operating officer of ECU Health and president of ECU Health Medical Center, joined a group of statewide health care leaders at the NC Chamber Health Care Conference on a panel titled “Working Together to Create Healthier Communities” on Sept. 14 in Durham.
Speaking to a packed room of health care, business, industry and government leaders from across the state, Floyd spoke about ECU Health’s unique position in eastern North Carolina as both the largest health care system and employer in the 29 county region, and the importance of maintaining high quality and high value care in rural communities.
“Thinking about the NC Chamber and what we’re here to talk about today, it’s important to remember North Carolina is the second largest rural state in the country,” said Floyd. “One-in-three people in North Carolina lives in a rural community so rural health care is a very critical and very personal endeavor. At ECU Health, we take our mission seriously to improve the health and well-being of eastern North Carolina, which is a region with some of the highest levels of poverty in the state.”

ECU Health is a leader in rural health care, Floyd said, and is constantly exploring new ways to improve access to care for rural communities. Speaking to topics such as improving mental health resources, partnering closely with schools, colleges and universities and investing in the health and well-being of team members, Floyd made it clear ECU Health’s role in the East goes far beyond just delivering health care.
“ECU Health is a health care provider, an educator and an economic engine for our 29 county region and we understand that collaboration is key to solving health care challenges,” Floyd said. “When I think about what we do, the reason we have a 974 bed hospital in a town of more than 80,000 people is because of the tremendous burden of disease in the communities we serve. Improving quality and cost is our goal and our clinical care component certainly plays a role in that, but we know that value is created by improving wellness through initiatives that tackle social determinants of health.”
Floyd was joined on the panel by Dr. Art Apolinario, board president of the N.C. Medical Society, Dr. Creagh Milford, senior vice president of retail health for CVS Health and Jennifer Sacks, associate director of the clinical operations program lead for Biogen. The panel was moderated by Gary Salamido, president and CEO of the NC Chamber.
A 2008 alumnus of the Brody School of Medicine at East Carolina University and current ECU Health physician detailed his experiences as a doctor in rural and underserved eastern North Carolina during a July 12 webinar.
ECU Health Duplin Hospitalist Director Jon Kornegay presented “Perspectives on Underserved Care: Being a Physician in Duplin County” through the ECU Global Health and Underserved Populations Program. He also serves as ECU Health Duplin vice chief of staff and Duplin County EMS medical director.
A native of Duplin County and part of a family of physicians, Kornegay has served Duplin County since 2012, creating the hospitalist group that has increased local patient volume and kept Duplin County residents closer to home for quality care. He was named one of ECU’s 2022 “40 Under Forty” honorees.

Kornegay began the talk by saying he reminds medical students and residents that practicing medicine in an underserved area is a unique experience that can enhance their views of medicine.
“It’s a good thing, at some point in your career, to spend a little bit of time in community hospitals,” he said.
Kornegay guided the audience through details of the challenges of health care delivery in a rural county, the expertise of his colleagues that blend to provide a more complete level of care to patients and how ECU Health Duplin, in Kenansville, has grown over the years. He also detailed how the Brody School of Medicine has influenced the approach to care.
Duplin County is nearly two hours from Greenville, with a population of around 50,000, making it a target area for Brody’s mission to serve rural eastern North Carolina and underserved communities.
“Brody had several mission statements when it was developed,” Kornegay said, “and one of the main mission statements was to train providers for eastern North Carolina. Primary caregivers are a really big issue, and we hope we’re addressing that somewhat.”
Kornegay said the health care landscape and its indicators — including that many providers are near or at retirement age — mean recruitment to rural communities needs to increase. Other challenges include patient insurance coverage and the geographical access to complex care facilities.
Kornegay praised ECU Health Duplin’s strong ties to the Brody School of Medicine, including current students and residents as well as seasoned physicians.
“We take kind of a plethora of Brody learners,” he said. “We have third- and fourth-year residents that come to do community rotations with us. This past year, we’ve also started taking ECU rural family medicine residents. All of our attendings have interactions with Brody learners and are kind of staying connected.”

Kornegay’s brothers, who also practice in eastern North Carolina, went to medical school or completed residencies through Brody. Chad Kornegay helped start the medical group in Duplin County in 2010.
“My dad’s been a family practitioner in the area for over 50 years,” Kornegay said, adding that his father retired a few years ago.
The family ties also help build a sense of kinship among the professionals that has resulted in a steady increase in patients served and a reputation for quality care.
In 2011, Kornegay said, there were 5,800 patient encounters through ECU Health Duplin; over the past three years, that number has stayed around 15,500.
“So we’ve almost tripled the service there in about 12 years,” Kornegay said. “We’ve grown the service quite a bit. As a pretty strong group clinically, we’ve had a lot more of a comfort level taking patients than they previously had had here.”
Kornegay shared firsthand accounts of what it was like to be a rural physician in a large, rural county. He told stories about bad car accidents, deliveries of premature babies,
and other emergencies that are made more challenging by remote locations. He also shared his experiences serving during several hurricanes that rendered many areas of Duplin County as islands.
Hurricane Matthew in 2016 presented Kornegay with an opportunity to adopt new skills for future storms.
“I grew up in Duplin County, so I’m used to kind of being around tropical storms and hurricanes,” he said. “But we had never seen anything like this in my lifetime, the amount of water that we got with Hurricane Matthew. And so that presents some challenges, some unique challenges, for us in the health care delivery at the county.”
That experience helped prepare Kornegay and other providers for unforeseen circumstances — and for continuing to live and work the mission of Brody and ECU Health to serve rural eastern North Carolina through challenges from geographical access to natural disasters.
“We really as a county had not recovered from Matthew before Florence came,” he said of the 2018 storm. “We had kind of rehearsed a little bit with Matthew, but one of the things we learned during Florence is you can try to prepare for everything, but you can’t. So you’ve got to be ready to modify and change your game plan when data changes and things change a little bit. When you get that curveball, you may have to pivot a little bit.”
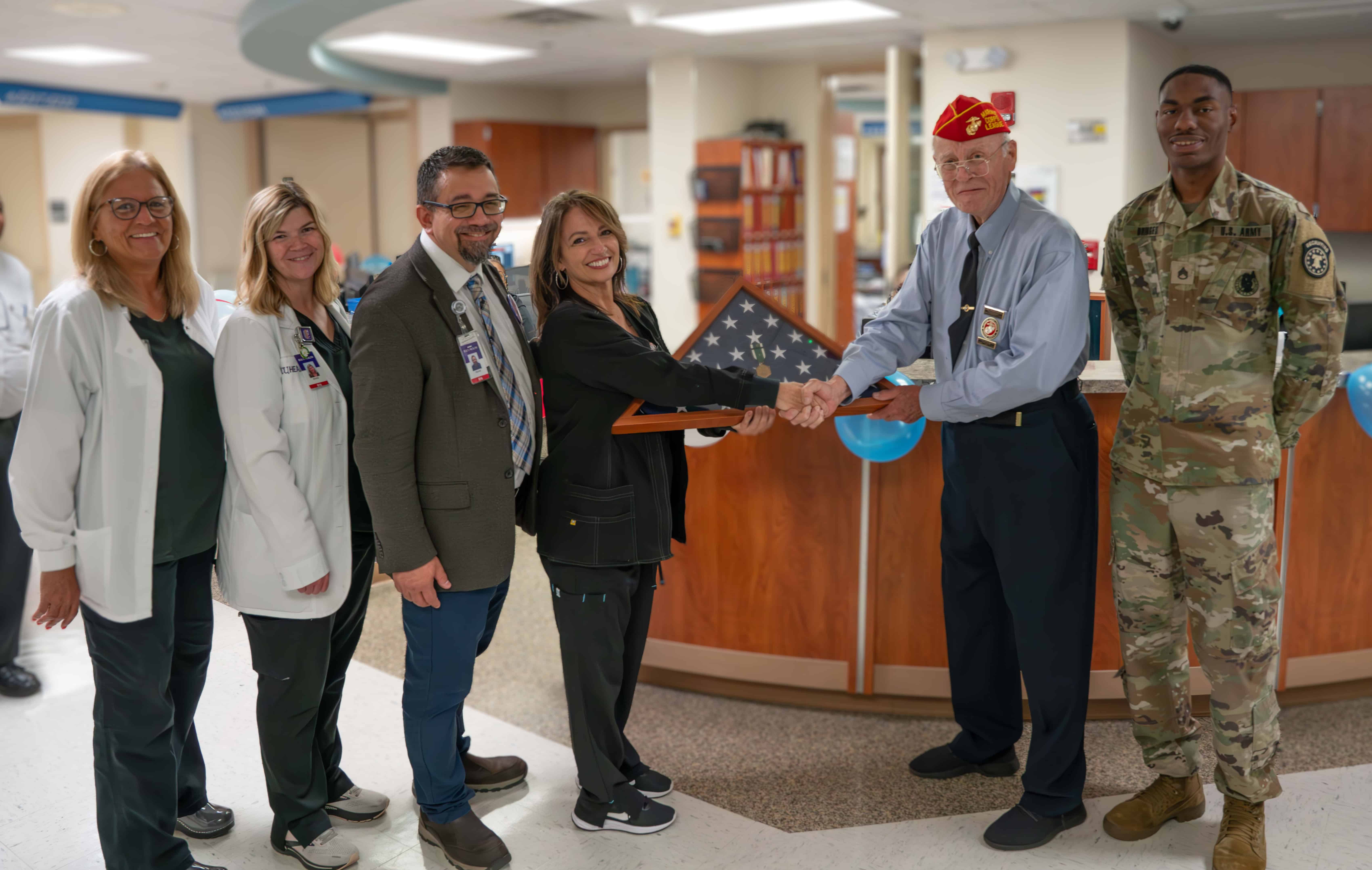
On a February morning, Vietnam veteran Lee Pascasio sat in his brother-in-law’s room on 2 East at ECU Health Medical Center. As Melissa Warren, a nurse on the unit, checked on Willis Johnston Stancill she noticed his blood pressure was spiking, and the team sprung into action.
Pascasio said he watched in silence as the team went to work saving Stancill’s life. He said he’d seen that kind of teamwork before in his time as a Marine. The experience moved Pascasio to gift his Navy Commendation Medal, earned during his service in Vietnam, to Melissa Warren and the rest of the 2 East team. Now, it hangs in the hall of the unit on top of the stars of the American Flag for all to see.
“This is such a great team,” Warren said. “It’s such a well-oiled machine, it’s like we’re dancing almost when something crazy like that happens. It’s not like you have to ask somebody to do something. We just kind of do it, that’s the team. If something happens, the troops are coming in.”
A Medal Earned
Pascasio recalled his time in Vietnam vividly. During his second tour in Vietnam, Pascasio said at 25 years old he was an old man compared to the rest of the First Battalion, Ninth Marine Unit, where he served as sergeant, specializing in explosives.
On June 30, 1969, Pascasio said he was at Vandegrift Combat Base with the Ninth Marine Unit and another platoon in Vietnam. That day, rockets and mortars began to hit the battalion without warning. A lieutenant was killed in the attack, leaving Pascasio in charge. Pascasio sent a sergeant to get a corpsman while he administered first aid to the wounded. When the medevac eventually arrived, Pascasio helped load the dead and wounded Marines so they could receive further care.
Two years later, Pascasio was presented with the Navy Commendation Medal at Camp Lejeune.
Appreciating a Care Team
In the days following his brother-in-law’s incident on 2 East, Pascasio shared his appreciation in the form of tacos, donuts, coffee, cheesecake, Cracker Jacks and other snacks.
“He’s just so appreciative,” Warren said. “I can’t give like a superhero story or anything about that night. It was what we do. It’s nice to have him, or anybody, recognize what we do. It’s a demanding job with your emotions, high energy, physically, everything. So it is nice for somebody to care that much when we’re just doing our job.”
For Pascasio, the treats weren’t enough to show his appreciation.
 “I said, ‘You know what? I want to do something nice for these people.’ They just saved my brother’s life. He got the best care in the world right here at 2 East,” Pascasio said. “I thought about Melissa and her team of crackerjacks on 2 East and I said, ‘This medal isn’t going to buy her a cup of coffee, but it’s straight from the heart.'”
“I said, ‘You know what? I want to do something nice for these people.’ They just saved my brother’s life. He got the best care in the world right here at 2 East,” Pascasio said. “I thought about Melissa and her team of crackerjacks on 2 East and I said, ‘This medal isn’t going to buy her a cup of coffee, but it’s straight from the heart.'”
“It was about their teamwork to save a life and the concern that we should all have. The nurses and teachers who have been through COVID are overlooked.”
Stancill passed away in May, but Pascasio said he still lives in his heart and in the heart of his wife, Emily Pascasio. He continues to be grateful for the care Stancill received, which Warren and her colleagues continue to find meaningful.
“This is for the whole unit,” Warren said. “I mean, you see the support of all the staff out there. They’re amazing. We are like family. When I come to work, when I walk in, we’re hugging each other. None of us could do this alone.”
ECU Health nurses from every area of expertise across the health system gathered on June 20 at the East Carolina Heart Institute for the 10th annual ECU Health Nursing Summit where they shared best practices and innovations that will help chart the future of nursing in eastern North Carolina.
Titled “Connecting with: Minds, Hearts and Purpose,” nursing leaders at ECU Health designed the summit to acknowledge what nurses have experienced over the last three years, including what the COVID pandemic taught them as professional nurses, what they have lost and what it will take to move nursing forward together, according to Trish Baise, ECU Health chief nursing executive.
“With the ever-changing health care environment, it is important for ECU Health nurses to hear from state and national colleagues,” said Baise. “We are proud to welcome experts who are making a positive difference in the field by advocating and influencing policy, as well as nurturing innovations that address the workforce, the nurse practice environment and the health and wellness of nurses.”

In total, more than 178 nurses attended the summit, which was held face-to-face for the first time since 2019. Topics included policy advocacy, building positive environments, communicating across generations, self-care and wellness. The summit featured presenters from both ECU Health team members and experts from other areas, including North Carolina State Senator Gale Adcock and keynote speaker Katie Boston-Leary, director of nursing programs for the American Nurses Association.
“The Nursing Summit gave me ideas, things to research and refreshed my mind to help navigate this different health care world that we live in,” said Paula Bush, MIU manager at ECU Health Edgecombe Hospital.
The summit also served as an opportunity for ECU Health nurses across various levels of expertise and experience to connect directly with health system leadership, fostering a sense of community among health system nurses.
“Sharing best practices from both within and outside the health system helps spark a culture of innovation within nursing,” said Daphne Brewington, ECU Health system vice president of nursing excellence. “When we harness the expertise of our nurses, we can lead improvements and create environments where nurses thrive here at ECU Health.”



