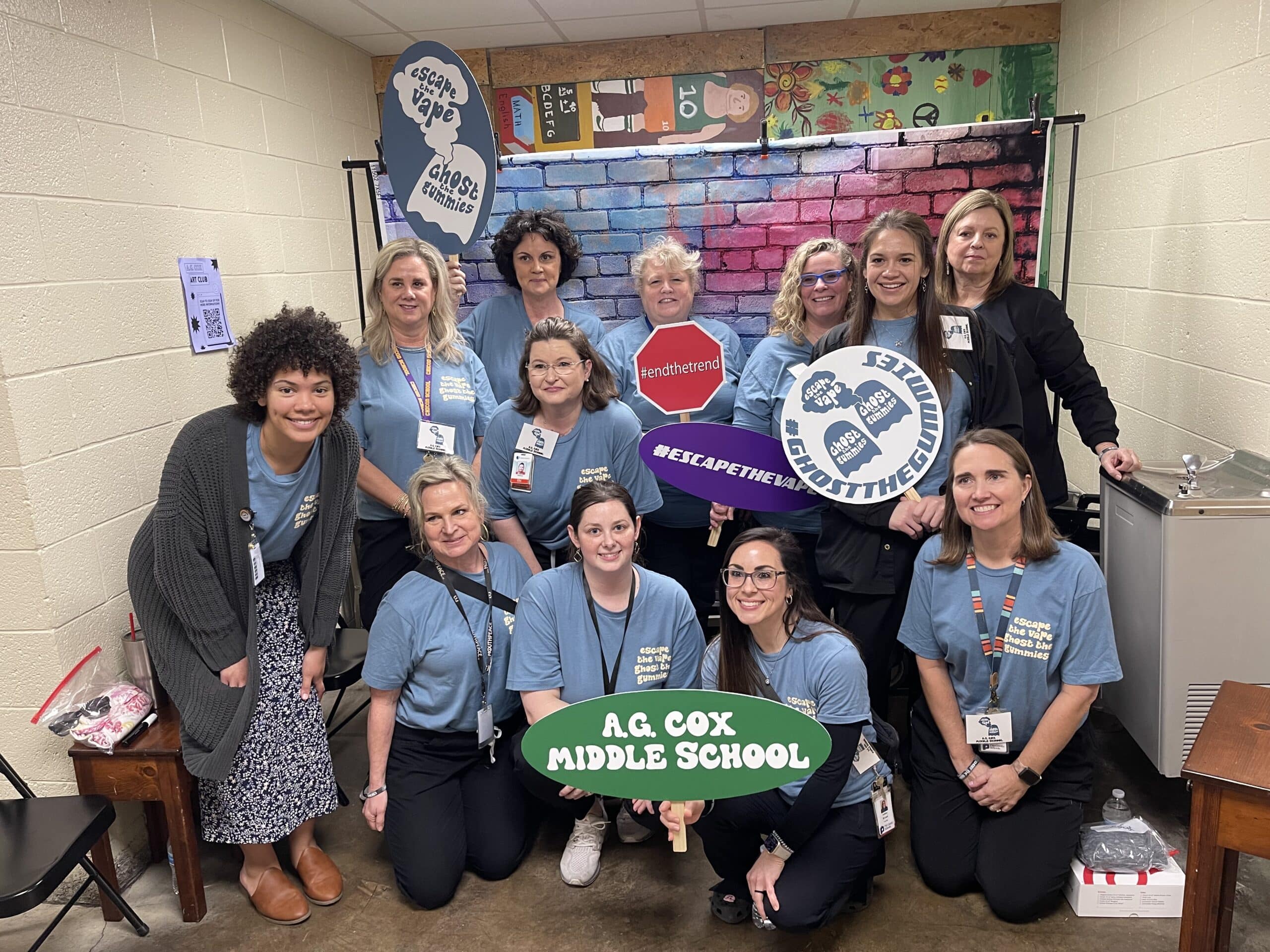
Students at A.G. Cox Middle School in Winterville learned about the dangers of vaping tobacco or other substances and drug use during an event hosted at the school on Feb. 28.
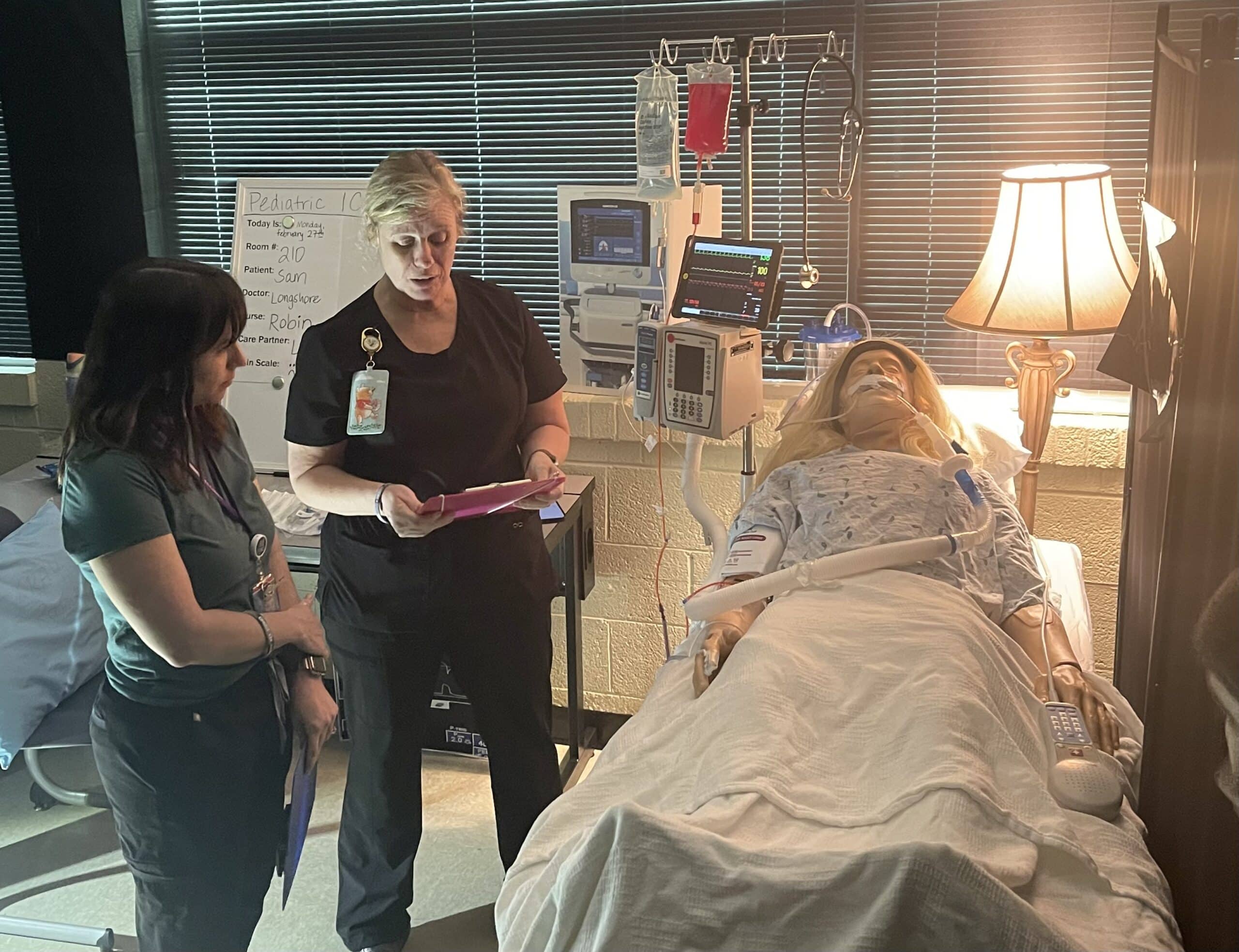
Pitt County School nurses, ECU Health team members and volunteers, and local high school students acted out two different scenarios for the A.G. Cox students, who are in grades 6-8, to show how quickly things can go wrong.
In one scenario, a student at a party takes a gummy from a friend, which turns out to be laced with drugs. The student then falls critically ill from the effects of the drugs.
In another, a student is taken to the hospital after using a vape they were told did not have tobacco in it, but instead was filled with an unknown drug.
Emerson Fipps, a senior at South Central High School in Winterville, helped act out the first scenario with another student and an ECU Health volunteer. She said she’s proud to support events where she can help other young people set themselves up to make positive decisions.
“Middle school is really where everything starts to come up,” Fipps said. “Teenagers are just trying to find themselves so they’re getting into things that they shouldn’t. They’re not really fully educated about everything these destructive decisions could affect. It’s really good for them to start hearing about it young because when they’re in these situations, they’ll already have the information.”
Tiffany Thigpen, the Region 10 tobacco prevention and control coordinator for the Pitt County Health Department, said schools across the country are seeing an increase of students vaping and using gummies and other drug-infused edibles.
The National Poison Data System reported 3,054 cases of pediatric edible cannabis consumption in 2021, a large increase from 207 cases in 2017.
Thigpen said one of the most important things parents can do to keep their children safe from tobacco and drugs is talk to them.
“Talk to your children, let them know that these things are not safe,” Thigpen said. “Let them know that it is OK to say no. Talk to them about refusal skills and ways to say no to their peers. Let them know they can talk to you about what they’re experiencing. If they do use these products, share the dangers with them and ways to stop.”
Thigpen said the county is working to get as much information as they can into the hands of students about the dangers of drugs and vaping to help stop addictions before they begin.
Laurie Reed, manager of school health services at ECU Health, said partnerships make all the difference for events like the one hosted at A.G. Cox Middle School.
“Our school board and our school health advisory committee are very supportive of programs like this in our school system,” Reed said. “We just hope we’ll be able to offer more of them. It’s a great collaborative effort and it takes a lot of effort on the part of our school nurses, Injury Prevention, our health department, but it’s a great collaborative opportunity for our community.”
Student perseverance and community and industry partnerships were highlighted in special presentations at the East Carolina University Board of Trustees’ February meeting.
The board also welcomed Brandon Frye, vice chancellor for student affairs, who officially joined ECU this week.
On Thursday, four students spoke during the University Affairs Committee meeting about their struggles and how ECU programs helped them continue to move forward. The students and the programs are: George Cherry Jr., Students’ Treasure Chest; Nellyana Cordero-Cisnero, Pirate Promise; Adam Harrison, Pirate Academic Success Center; and Iyaira Williams, Purple Pantry. Chris Stansbury, associate vice chancellor and senior operating officer for student affairs, moderated the panel.

In introducing the students, Provost Robin Coger said earning a degree requires students to persevere even when faced with challenges. ECU provides a range of support for student success. “Ultimately they come out of ECU ready for successful careers, but there are a lot of steps in between,” she said.
Cherry, who is earning three degrees and plans to attend medical school, put 24,000 miles on his car driving to class last year from his Bertie County home, where he helps take care of his younger sister. He was able to get help from the Students’ Treasure Chest when his car needed repairs. He is working to give back to the university through service and his involvement in different organizations, including the Student Government Association.
Cordero-Cisnero is a first-generation student from Raleigh who attended community college before transferring to ECU for a degree in elementary education. She said an ECU alum introduced her to Pirate Promise, which gave her a path to a four-year degree. “It opened a new door for me,” she said.
Harrison said he commuted from his home in Williamston his first year, and the connections he made at the Pirate Academic Success Center helped him become a stronger student. He now is a mentor to other students at the center.
Williams, from Raleigh, has volunteered at the Purple Pantry since her freshman year. As an ambassador, she helped the organization win a collegiate hunger challenge and $10,000, and she continues to work with the pantry to combat food insecurity. A recent partnership with the SGA has yielded almost 90 meals donated from unused meal swipes. The SGA also provided funding to purchase a freezer for the pantry to provide frozen meals.
The panel encouraged trustees to continue hearing from students and provide opportunities for conversation. They also suggested continuing to bring awareness to the resources that ECU offers.
In another committee Thursday, the trustee’s Committee on Strategy and Innovation heard an industry workforce panel discuss how partnerships can lead to innovation and economic prosperity in eastern North Carolina and beyond. Participants included representatives from ECU Health, Fly Exclusive and MrBeast. Topics ranged from the importance of building and strengthening partnerships and pathways to identifying ECU student and graduate talent to recruit to their businesses.
Panelist Julie Oehlert, chief experience and brand officer at ECU Health, said both the university and the health system can benefit from working more closely to integrate student experiences into education in a wide variety of disciplines in health care and beyond.
“We share a community, we share learners that we both love deeply, in a variety of settings,” she said. “We share the responsibility of caring for eastern North Carolina; for educating eastern North Carolina and for advancing all the people that live in eastern North Carolina in their learning and in their health. That’s why we are ECU Health now; never before has the imperative for a strong partnership been more relevant or more necessary.”
The panelists and committee discussed ways to encourage partnerships based on innovation and thinking outside the box that will push students to create real-world solutions in situations that prepare them to enter the workforce with concrete foundational experience.
The committee also adopted a resolution on freedom of expression for faculty and students, which was unanimously approved by the full board on Friday. The resolution reaffirms the Board of Trustees’ commitment to academic freedom and freedom of expression in which faculty and students can “teach, learn, seek and speak the truth” in an environment where “academic freedom flourishes” and the campus community is given “the broadest possible latitude to speak, write, listen, challenge and learn except insofar as limitations to that freedom are necessary to the function of the university.”
Trustees also received an update on refreshing the university’s strategic plan. Committee co-chair Sharon Paynter presented a list of internal and external strengths, weaknesses, threats and opportunities that impact university initiatives and ways ECU leadership, faculty, staff and students continue to navigate them.
Read more from ECU News Services
Support, action and investment are needed in the East to solve what community members and experts alike are calling a mental health crisis across the region and state. That was the common theme at the Mental Health Town Hall in Greenville hosted by North Carolina Department of Health and Human Services (NCDHHS) Secretary Kody H. Kinsley and local legislators Feb. 9.
The bipartisan panel for the town hall featured Rep. Gloristine Brown, Sen. Jim Burgin, House Majority Leader John Bell, Rep. Dr. Tim Reeder and Sen. Kandie Smith, all of whom represent districts that fall within ECU Health’s 29-county service area. With more than 150 people in attendance, community members and representatives for local organizations shared their perspectives on mental health with the panel.
Kinsley said town halls are crucial to help him and other state officials understand the unique challenges in each area of the state.

“We are having mental health challenges all across the state, but every community is different because every community’s resources are different and their needs are different,” Kinsley said. “It’s really important to me as we set statewide policy that we’re doing it in a way that is informed by boots on the ground, and we heard a lot of that tonight, and we know we have a lot of work to do, and I’ve appreciated this conversation.”
Dr. Michael Lang, chair of the Department of Psychiatry & Behavioral Health at ECU Health and the Brody School of Medicine said the town hall was a positive step to help share with leaders what he and others are seeing locally. He said it was symbolic to bring the event to Greenville where he and his team see a disproportionate number of patients daily needing mental health resources at the ECU Health Medical Center Emergency Department.
“This was a great event for us overall,” Dr. Lang said. “We had a chance to meet our leadership from Raleigh and let them know about the issues and challenges we’re facing, not only here in eastern North Carolina but across the state. I can tell you firsthand we feel the impact of the mental health crisis here in the region and here in Greenville at the medical center. The challenges we’re talking about, such as a lack of access to resources and a dependence on emergency department visits for those suffering from mental health crises, are felt every day at hospitals across the region. That’s why it is important to focus on improving outpatient behavioral health resources to crate stable environments and prevent hospitalization.”
Officials noted there are at least 350 mental health patients in emergency departments across the state waiting for bed placement on any given day. The lack of access to care and resources are more magnified in rural areas such as eastern North Carolina where there is a disproportionate number of under or uninsured individuals. The bipartisan panel all agreed Medicaid expansion in North Carolina would help provide necessary resources towards solving the crisis and Sen. Burgin noted that Medicaid expansion would allow the state to spend more than $1 billion on improving access to behavioral health resources.
 “ECU Health is grateful for our local legislators who are committed to having these difficult but necessary conversations while at the same time pursuing common-sense solutions like Medicaid expansion,” said Brian Floyd, chief operating officer, ECU Health. “Medicaid expansion would help provide needed health coverage to 100,000 people in our region and improve the way we as a state deliver behavioral health resources.”
“ECU Health is grateful for our local legislators who are committed to having these difficult but necessary conversations while at the same time pursuing common-sense solutions like Medicaid expansion,” said Brian Floyd, chief operating officer, ECU Health. “Medicaid expansion would help provide needed health coverage to 100,000 people in our region and improve the way we as a state deliver behavioral health resources.”
At ECU Health, the system announced a partnership with Acadia Healthcare to build a state-of-the-art, 144-bed behavioral health hospital in the medical district of Greenville, less than a mile from ECU Health Medical Center.
The hospital, slated to open in 2025, will provide important access to behavioral health services for adults and pediatric patients, with 24 inpatient beds specifically for children and adolescents with mental health needs.
“I’m incredibly grateful for health systems that have been investing in building more behavioral health beds,” Kinsley said. “This is important but I have a job to do on this, too. We have got to increase [reimbursement] rates to help make those beds sustainable and used.”
Resources
East Carolina University’s postgraduate program in cardiac psychology creates professionals who are ready to help patients cope as they adapt to life-saving heart devices.
On the heels of marking its 15th year, ECU’s nationally unique program in clinical health psychology continues to gain momentum through positive patient outcomes — and national recognition.
The program is a collaboration between ECU’s departments of psychology and cardiovascular sciences that has yielded a nationally unique blend of academics and research. The model integrates training psychology doctoral students and cardiology fellows in cardiac clinics, a strategy that the program’s founder calls the best of both worlds.

“This is a success story from eastern North Carolina,” said Samuel Sears, program director and professor in the departments of psychology and cardiovascular sciences. “From a national landscape, this is an extremely unique program. Only at East Carolina do you have this kind of synergized, integrated, one-for-one engagement in the training of cardiologists and the training of psychologists. Our program is intending to lead the country in this.”
Sears established the training program in 2007 and collaborates with Rajasekhar Nekkanti, associate professor and director of the cardiology fellowship program at ECU and ECU Health, to offer ECU students an integrated program experience that spans clinical care, research and training.
“Dr. Sears and his colleagues have been able to accomplish what others have only talked about,” said Alan Christensen, professor and chair of the ECU Department of Psychology. “Their seamless integration of clinical psychology into a cardiovascular medicine setting is really a pioneering effort in implementing what I believe will prove to be a more effective approach to training, research, and caring for patients.”
The growing field of cardiac psychology focuses on providing psychological care that is an interdisciplinary, comprehensive care approach to cardiac arrhythmia patients and their families.
Depression and anxiety are common occurrences after cardiac events and can occur in as many as one-third of all patients. These conditions interfere with all aspects of recovery from daily rehabilitative planning, medication adherence, and the pursuit of quality of life.
“Cardiac psychologists help by validating the emotional experience of having a heart problem, and helping patients take the next steps in their recovery emotionally and behaviorally,” Sears said. “ECU Cardiology and Cardiovascular Surgery continue to innovate, and that allows our patients to survive. Here at East Carolina, we have the vision and program to address the patient experience and recovery process fully from a psychological and behavioral perspective. We integrate all the aspects of recovery and prepare trainees for the future of cardiac care.”
The program was highlighted in a 2022 edition of Health Psychology, a journal of the American Psychological Association. The article, “Cardiac Psychology Training in a Rural Health Care Setting: East Carolina Heart Institute,” was led by author Kayla Sall, a 2023 graduate of ECU’s clinical health psychology program. Doctoral students Ashley Griffith, Emily Midgette, Andrea Winters and Connor Tripp also co-authored the article with Sears and Nekkanti.
“We are very proud to publish in our field’s top journal,” said Sall, who begins a psychology internship at Brown University this fall. “The publication goes to show how unique our training experience is. It’s very rare to find cardiac psychologists that are located in cardiology.”
The Health Psychology article covers not only the program’s unique nature of intertwining science with practice, but also its ability to adapt to the COVID-19 pandemic by transitioning to using telehealth to serve patients in rural North Carolina. It also explores the health disparities in eastern North Carolina that impact cardiac patient care and progress.
“Cardiovascular health is one of the leading causes of death in the U.S.,” Sall said, “so being able to take that lens and apply it to the social determinants of health has been amazing, and it’s how we’ve been able to do what we do.”
Greenville native and ECU graduate Scarlett Anthony didn’t have to go far to find a program that offers world-class education and preparation that will help her make a difference in her home region and beyond.
“I chose ECU’s program because of the focus on health psychology and the intersection between psychology and medicine. We train alongside psychologists who are embedded in medicine, and our program provides us with exceptional training among various health care settings,” said Anthony, a doctoral student in clinical health psychology. “I chose ECU’s program because of the dedication to serving diverse populations of eastern North Carolina, and I am passionate about providing care to those who may not have access to health psychology services otherwise.”
Standards of practice

Sall led the writing team in detailing the ECU training program and its strong collaborations in cardiology. The article presents ECU’s program as a national model for ideal collaboration between cardiology and psychology training that enhances the clinical and research expertise of both groups.
The ECU cardiac psychology program is part of the APA accredited clinical health psychology program. This program has achieved national rankings over its 15-year existence and annually has an approximately 5% acceptance. Rob Carels serves as the director of clinical training for the clinical health program.
“The article confirmed that the ECU program is not only one of a kind, but it remains the model as programs and universities try to create this similar-type experience,” Sears said. “The reason it’s so hard to create the ECU experience is that it requires both physicians and psychologists accommodating very different mindsets and contributions with the shared goal of patient success first. Physicians can quickly implant a cardiac device. Psychologists can quickly assess and treat psychological concerns. But when these two sets of problems merge, we need shared expertise.”
The article also highlights the setting of ECU’s health psychology program, a rural area where the social determinants of health — including environment, economic stability, community context, education and health access — impact health and wellness on a greater scale.
“Being in eastern North Carolina, we have a very unique setting with our patient population in a rural area,” Sall said.
That context allows psychologists to better understand the behavioral and mental health of cardiac patients. Many patients seen by cardiac psychologists at the East Carolina Heart Institute include those who suffer depression after a heart attack or other cardiac event, those with atrial fibrillation (a-fib) and those who have recently been fitted with implantable cardioverter defibrillators (ICD) — devices similar to pacemakers that correct heart arrhythmias with a high energy shock that can feel like being kicked by a horse.
“I think that is what is so scary for patients; they agree to have this device implanted, they know it’s life-saving, but you don’t know when the shock is going to go off,” Sall said. “You may go the whole rest of your life without receiving a shock, so that’s where part of the anxiety and fearfulness comes in.”
In the program’s scientist-practitioner approach, providers on each side have a thorough understanding of the opposite discipline.
“I think that’s what’s cool about cardiac psychology — here we are with people presenting with medical conditions or health issues and we’re evaluating, diagnosing, treating emotional behavioral disorders within the context of health and medicine,” Sall said. “We’re not doing just one or the other, we’re doing these together.”
World expert in action
Sears is a highly productive researcher examining quality of life and psychological adjustment in patients with heart rhythm disorders and ICDs. He has published more than 200 articles in the medicine and psychology research literatures and has well over 11,000 citations. In 2021, Expertscape.com named Sears one of the top 50 experts and most prolific authors in the world on ICDs over the last 10 years, amongst the 27,847 authors on the topic.
“I’m involved in both the training of psychologists as well as the training of cardiologists, so we’re trying to make cardiologists better at patient psychology and psychologists better at understanding the cardiology, so it’s synergistic,” Sears said.
Sears travels the world presenting his research and lending his expertise to patient, family and physician groups.
In 2013, the UNC Board of Governors presented Sears with the O. Max Gardner Award, the highest honor bestowed to a faculty member in the UNC system for contributions to mankind.
“The O. Max Gardner Award changed me because I stopped looking for external validation about our achievements. I desperately wanted to make an impact on our patients, our students, our university, our state and beyond,” he said. “The award confirmed some of these marks, so I used my energies more efficiently on the work at hand. I am proud of the health psychology program and the cardiac psychology program that my colleagues and students have created. In terms of work, I am so pleased that many of our ideas about helping cardiac patients are broadly employed across many sectors in cardiology, not just where we started.”
The article in Health Psychology signals consistent success and upward momentum for the program, said Sears, adding that Yale University’s health psychology program is the only other such program mentioned in that edition of the journal.
“This is a 15-year-old program. We’ve established success,” he said. “This is not a great idea that’s going away. Great ideas happen all the time, but they’re not sustainable. This is a sustainable solution that has true outcomes.”
When it comes to patient outcomes, Sears is optimistic that the growing field of cardiac psychology will continue to yield hope and healing.
“We can’t fix all the health inequalities, but what we can do is help our patients make small steps to have better awareness of where there are a lot of possibilities and decision points, and connect them to other resources,” Sears said. “Yes, this is a hard mountain to climb. Let’s do this together.”
Doctoral student Zachary Force said students begin the program learning what clinical health psychology can offer the world — and how ECU is leading the way.
“ECU has always done things differently, and other institutions are starting to take notice. ECU’s cardiac psychology service has received national recognition as the only place in the country to receive specialized training in an area with increasing need,” he said. “ECU’s fighting spirit imbues its doctoral students with the resiliency needed to advocate for psychology within the medical field.”
Read more from ECU News Services
“It was very nerve wracking coming here,” said Denique Barnett, a pediatric rehab nurse at the James and Connie Maynard Children’s Hospital and international nurse at ECU Health. “I’m an only child, so leaving my family in Jamaica was very hard.”
For Barnett, pursuing her passion has been a journey of more than a 1,000 miles.
“The welcome that I received was a good one,” Barnett said.
The warm reception Denique received is one ECU Health offers nurses from around the world as part of the International Nurses Program.
“My passion is pediatrics, but specifically neonatal nursing,” Barnett said. “Back home there is no degree program for neonatology. So I decided that, you know, to further my studies and to self-actualize, I would need to come to the United States.”
Not only does the program foster additional growth and training for participants, it also fills an important recruiting need for the health system.
“We bring international nurses from all over the globe to come to our organization to spend about two years in a clinical environment,” said Charlene Wilson, chief people officer of ECU Health.
Launched in November 2019, 175 nurses from 21 countries have since spent time at ECU Health.
“Even though these are nurses that are seasoned nurses, they have to go through our NCLEX,” Wilson said. “They then go through the immigration process. They then begin to understand the culture of the various hospitals that have openings for international nurses. One of the things that is very different about their practice here versus their practice in their home countries is the technology.”
“At first, you know, getting used to just how things are done here using technology for me, that was a bit of a challenge,” Barnett said.
“I’m always told by the clinicians, including the doctors, that one of the things that is fascinating about what they bring is their analytical skills, because they don’t have the technology that we have here in the United States,” Wilson said.
It’s a unique perspective put to work for a common goal, improving the health and well-being of the region these nurses now call home.
“As an international nurse, making the leap is the best decision that you will make. There is a lot of opportunities for growth,” Barnett said. “There are a lot of benefits to being here at ECU Health, you know, just make the leap, come, you won’t be disappointed.”
Leaders of Pitt County’s Health Sciences Academy are working hard to give students the real-life skills needed to succeed in the work world—thus fueling the talent pipeline for our state’s employers.
While labor shortages have been prevalent across all industry sectors in recent years, it has been particularly acute in the health care industry and even more so in our state’s more rural communities. However, for Pitt County, this program has brought a tangible solution for training the next generation of health care talent in the Greenville area.
The Health Sciences Academy is a curriculum program, which was created to expose and prepare Pitt County high schoolers who wish to pursue a health care-related career after graduation.

During high school, students participating in the program complete a minimum of six courses that prepare them for various health careers. As part of their program experience, students can participate in job shadowing, mentoring, internships, medical research opportunities, career exploration, and volunteering at ECU Health. In addition to ECU Health, the school system works in tandem with East Carolina University Division of Health Sciences, Brody School of Medicine, the ECU Dental School of Medicine, Pitt Community College, Eastern Area Health Education Center, and the Greenville-Pitt County Chamber of Commerce.
“When people think of health care, they think of doctors and nurses,” said Reed Potts, Health Sciences Academy Coordinator. “Doctors and nurses only make up 30% of the health care workforce, so there are many more jobs out there that the kids do not know about.”
The program, which began in 2000, currently has approximately 1,000 student enrollees, and works with high school students exploring all pathways including two- and four-year colleges, trade school, the military, and others. Potts expressed pride that 30 members of the program’s current cohort will be first-generation college students.
“Seeing a career firsthand — you’ll know whether or not it’s for you,” said Lisa Lassiter, director of workforce development at ECU Health. “We had a student who was set on being a labor and delivery nurse, but after a firsthand experience through Health Sciences Academy, she adamantly decided it was not for her anymore. That’s valuable too, because if she hadn’t had that opportunity, she never would have known until her junior year of college during clinicals.”
Potts said that standalone career nights are extremely beneficial to recruiting future students into the program because they can touch, see, and feel medical equipment and talk to staff about potential careers firsthand. They are also now starting recruitment efforts even earlier among middle schoolers.
To participate in the Health Sciences Academy, students must maintain a 3.0 GPA, have a clean disciplinary record and complete 25 hours of volunteer hours per year. There are also two dedicated counselors that work directly with Health Sciences Academy students and travel to all of Pitt County high schools.
In this program, students learn many soft or durable skills, including leadership, critical thinking, accountability, and communication, and they also get other important training such as etiquette lessons, resume building, and ACT and SAT workshops.
Potts stated that there has been a major return on investment as this program expands the talent pipeline in the Greenville area. “Roughly 50% of the students who go through the Health Sciences Academy stay in the area and go to East Carolina University,” he said. “And we anticipate seeing that number go up even more.”
He also attested that every single student who goes through the program goes to a two- to four-year college, trade school or the military.
When asked what recommendations they would make to other counties looking to implement similar programs, both Potts and Lassiter discussed the importance of constant two-way dialogue between the health system and school system, to ensure the needs of both parties are being met.
“Having direct communication with the school system has been extremely beneficial because we can discuss what’s going great and how to mitigate certain challenges,” said Lassiter. “As a result, we have this very well-trained future pipeline.”
She also stated that many people may be turned off by the cost of a similar program but suggested that other schools and health systems can start small by using time as a resource or having exposure activities that do not cost money.
Read more on NCChamber.com.
Windsor, N.C. – ECU Health is pleased to announce ECU Health Bertie Hospital has been named a 2022 Human Experience (HX) Guardian of Excellence Award® winner for physician engagement by Press Ganey, the global leader in health care experience solutions and services. This award is part of Press Ganey’s annual ranking of the top hospitals and health systems in the country, according to performance in physician engagement.
“It is an honor to receive this award on behalf of the dedicated team members who make ECU Health Bertie a top performing hospital for physician engagement,” said ECU Health Bertie Hospital President Brian Harvill. “It takes a dedicated group of individuals working together to care for a community. I could not be more proud of the ECU Health Bertie doctors, nurses and support staff who work tirelessly to provide excellent patient-centered care to those we are honored to serve.”

As a winner of the Press Ganey HX Guardian of Excellence Award®, ECU Health Bertie is in the top 5% of health care providers in physician engagement in the last year. Press Ganey works with more than 41,000 health care facilities in its mission to reduce patient suffering and enhance caregiver resilience to improve the overall safety, quality and experience of care.
“By putting their patients and workforce first each and every day, ECU Health Bertie Hospital is demonstrating their unwavering commitment to their employees and to the communities they serve,” said Patrick T. Ryan, chairman and chief executive officer, Press Ganey. “The caregivers at ECU Health Bertie have inspired us with the compassion, empathy and human connection they bring to the clinical healthcare setting. We are honored to partner with them as we celebrate their achievement.”
Team member engagement is central to how ECU Health creates positive experiences and delivers upon its mission to improve the health and well-being of eastern North Carolina. Per fiscal year data, ECU Health Bertie providers rated their engagement better than the national average in all five key engagement performance indicators: engagement, alignment, safety, resilience and diversity.
“As an organization dedicated to providing rural health care, ECU Health understands that exceptional patient experiences are created by compassionate, energized and engaged teams,” said ECU Health Chief Experience Officer Dr. Julie Oehlert. “This award from a globally recognized health care leader like Press Ganey is a testament to our whole team which goes above and beyond to overcome the challenges we face and ensure communities across our region have access to high-quality compassionate care they deserve.”
To learn more about ECU Health Bertie Hospital, visit ECUHealth.org/Bertie
Greenville, N.C. – The National Accreditation Program for Breast Centers (NAPBC), a quality program administered by the American College of Surgeons, has granted accredited status to ECU Health Medical Center for the ninth year. Patients receiving care at a NAPBC-accredited center have access to information on clinical trials and new treatment options, genetic counseling, and patient-centered services including psychosocial support, rehabilitation services and survivorship care.
“ECU Health serves a vast rural region burdened by high prevalence of chronic diseases including cancer,” said Brian Floyd, chief operating officer of ECU Health and president of ECU Health Medical Center. “Our partnership with the Brody School of Medicine at East Carolina University allows us to provide research and clinical trials for patients, as well as recruit high-quality cancer care providers, both of which largely contribute to our accreditation. Bringing standardized, quality care close to home for the 1.4 million people we serve helps us meet our mission of improving the health and well-being of eastern North Carolina.”

Breast cancer is the second leading cause of cancer deaths for women in North Carolina, according to the North Carolina Department of Health and Human Services. The even higher prevalence of cancers in eastern North Carolina highlights the importance of having an accredited cancer care center in the region. Access to preventative screenings and early detection allows for less invasive treatments, a greater variety of options and a greater potential to prevent the spread of breast cancer.
“ECU Health is committed to maintaining excellence in the delivery of comprehensive, compassionate, patient-centered, high-quality care for patients with all types of cancer,” said Dr. Emmanuel Zervos, executive director of cancer services at ECU Health, and professor at the Brody School of Medicine at ECU. “Patients with breast cancer at ECU Health benefit from a robust team of disease site specialists in surgery, oncology and radiotherapy who are committed to working together to provide the type of care this important designation represents. I am grateful to our ECU Health team members and new breast cancer program leader, Dr. Karinn Chambers, for not only adhering to these standards but surpassing them.”
Accreditation by NAPBC is granted to programs proven to provide the best possible care to patients with breast cancer. To achieve voluntary NAPBC accreditation, a breast center demonstrates compliance with the NAPBC standards that address a center’s leadership, clinical services, research, community outreach, professional education and quality improvement for patients. Breast centers seeking NAPBC accreditation undergo a site visit every three years.
To learn more about breast cancer screenings and treatment options near you, please visit ECUHealth.org/breast-cancer.
Greenville, N.C. – ECU Health, the premier health system serving eastern North Carolina, experienced a transformational year highlighted by the introduction of a new brand, announcement of a new behavioral health hospital, recognition of multiple team members on the state and national levels and realization of clinical achievements and innovations that enhance the care for the 1.4 million people the organization proudly serves.
“As we reflect on the historic year that was and celebrate our achievements, I want to take a moment to extend my heartfelt gratitude to the team members who make ECU Health what it is: a premier rural academic health system dedicated to serving the people who call eastern North Carolina home,” said Dr. Michael Waldrum, ECU Health CEO and Dean of the Brody School of Medicine. “As one year comes to a close and another begins, I know the next chapter of our shared story will be just as important. Our efforts in 2022 helped position us to navigate the complex challenges we face moving forward by bringing clinical, education and research innovations, but we still have work to do in the upcoming year and beyond to ensure our communities have access to the high-quality care they deserve.”

The following highlights are only a few of the many achievements across ECU Health in 2022. For a more comprehensive review of the year, please visit: ECUHealth.org/YearinReview2022
Evolving to ECU Health
The re-brand to ECU Health is a visual reminder of how transformative the year has been. The ECU Health logo is a symbol of the commitment to transforming and elevating health care for millions, training the providers of tomorrow, collaborating with community partners to solve complex issues and bringing clinical innovations that improve the lives of those who call this region home.
The Brody School of Medicine at East Carolina University and the health system began a joint operating agreement on Jan. 1, 2022. In April, the two organizations hosted a press conference and shared the new logo for ECU Health and announced the brand launch that would begin in May.
In the months since, there have been visual changes across the health system from signage around hospitals and clinics to websites and social media channels. More importantly, the creation of ECU Health has opened the door for the system to improve access to care across eastern North Carolina while training health care professionals through Brody.
Expanding access to behavioral health care in eastern North Carolina
Access to behavioral health care is crucial across the country, but especially in rural areas like eastern North Carolina. In June, ECU Health and Acadia Healthcare announced plans to build a state-of-the-art, 144-bed behavioral health hospital in the medical district of Greenville, less than a mile from ECU Health Medical Center.
Slated to open in spring 2025, the hospital will operate through a joint venture between ECU Health and Acadia, the largest standalone provider of behavioral health care services across the United States. Together, the organizations will invest approximately $65 million in expanding behavioral health resources in eastern North Carolina.
The hospital will include 24 inpatient beds specifically for children and adolescents with mental health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
Twenty-two ECU Health nurses recognized among Great 100 Nurses of North Carolina
This year, 22 ECU Health nurses were selected to the 2022 NC Great 100. This is the largest number of ECU Health nurses to receive this recognition. The honorees were celebrated at a gala hosted by The North Carolina Great 100, Inc. in Greenville in October.
Since 1989, The North Carolina Great 100, Inc. has recognized and honored nurses around the state for their commitment to excellence and to promote a positive image of the nursing profession. Out of thousands of nominations that are submitted annually, 100 recipients are selected based on their outstanding professional abilities and contributions made to improving health care services to their communities.
ECU Health Beaufort Hospital designated as primary stroke center by The Joint Commission
In July, ECU Health Beaufort Hospital – a campus of ECU Health Medical Center was designated as a primary stroke center by The Joint Commission and the American Heart/Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients. Stroke is one of the leading causes of death in the state, resulting in more serious long-term disabilities than any other disease.
With ECU Health Beaufort’s designation, all ECU Health’s hospitals are stroke certified by The Joint Commission.
Greenville, N.C. – ECU Health’s EastCare team was awarded MedEvac Transport of the Year by the Association of Air Medical Services (AAMS) for their initial transport of East Carolina University freshman Parker Byrd and subsequent transports throughout his recovery. The EastCare air medical team, Steve Bonn, pilot, Henry Gerber, EMT, Milando Stancill, EMT, Leigh Ann Creech, communication technician, Jessica Rispoli, flight RN and John vonRosenberg, flight paramedic, accepted the award on Oct. 26 for their efforts rendering life-saving care to Byrd.
On July 23, 2022, Byrd, an incoming freshman and baseball player at ECU, was boating in a remote creek when his legs were cut by the propeller, resulting in severe trauma. A friend and teammate was able to pull him back in the boat and immediately applied a makeshift tourniquet. First responders on the scene recognized the severity of his injuries and requested air medical transport. The EastCare air medical team jumped into action, rendering life-saving trauma care on the flight to ECU Health Medical Center, the only Level 1 Trauma Center east of Raleigh.

“EastCare team members dedicate themselves to ensuring the people of eastern North Carolina who live in vast, rural areas have access to timely and life-saving care,” said Trey Labreque, director of EastCare. “Thanks to the quick actions of everyone involved, including Beaufort County EMS for their initial response and clear communications with the flight crew, the transition of care was quick and efficient, and the patient made it to the trauma center stabilized, which is our objective as a flight team. This award is testament to all EastCare team members who live the ECU Health mission.”
Quick actions by the flight crew dramatically improved Byrd’s vital signs prior to arriving at ECU Health Medical Center. Flight nurses administered plasma, blood products and treatment for traumatic hemorrhagic shock during the air transport. In the following weeks, due to the severity of injury, the EastCare team provided Byrd transportation to the wound care center twice daily, multiple times per week to receive specialized care and hyperbaric treatments at ECU Health’s Wound Healing Center.
“The EastCare team has been nothing but phenomenal to me,” said Byrd. “From day one, they were doing their job to the best of their ability. I want to thank each and every person on the EastCare team for what they have done for me.”
Byrd was discharged in mid-August, nearly one month after his injury. After 22 surgeries and a partial leg amputation, Byrd continues to undergo outpatient care and rehabilitation in his recovery process. Byrd plans to continue classes at ECU and practice with the baseball team while he undergoes rehabilitation.
Please join ECU Health in recognizing the EastCare team for their rescue of Byrd and their efforts to render emergency care to all patients across eastern North Carolina.
