Scott Alford, the manager for grounds and guest parking at ECU Health Medical Center, generally considered himself to be healthy. Then, in 2023, Alford received some surprising news: his A1C, a blood test that measures the average blood sugar level over the last two-to-three months, was 10.9. For reference, a normal A1C level is less than 5.7. Prediabetes is 5.7 – 6.4, and diabetes is 6.5 and higher. “I was clearly in the diabetic category,” Scott said. “I asked the doctor what I should do. He gave me two medications and told me we’d revisit the issue at my next appointment.”
That solution didn’t sit well with Scott, so he made a decision. “I knew about ECU Health’s Lifestyle Medicine clinic because I knew some co-workers had used it,” he said. “I called them up and told them my story. They wanted to get me in right away. By the end of that call, I had an appointment with the nutritionist and a lifestyle coach for the very next week.”
Lifestyle Medicine is an evidence-based approach to preventing, treating and reversing diseases through healthy behaviors, and the ECU Health Lifestyle Medicine clinics offer many individual, group and virtual services to help community and team members meet their personal health goals.

“Our team of professionals includes providers, registered dieticians, lifestyle coaches, exercise physiologists, nurses and chefs who recognize the importance of including the six pillars of lifestyle medicine into the individualized care plans for our patients and team members,” said Brenda Leigh, the director of Lifestyle Medicine at ECU Health. The six pillars include increasing the consumption of whole, plant-based food, increasing aerobic activity, getting enough sleep, decreasing unhealthy substances (like tobacco or alcohol), maintaining healthy relationships and managing stress.
Scott first met with Lindsay Luschwitz, clinical dietitian III, to begin his Lifestyle Medicine journey. “I don’t drink and I don’t smoke, but I did drink between five and seven big soft drinks or sweet teas a day,” Scott shared. “I was also in the habit of stopping at McDonald’s every morning for breakfast and going out for lunch every day.”
When Scott shared this information with Lindsay, she didn’t shame him as he expected. Instead, she gave him different strategies and choices to try. “When we first met, Scott told me he wasn’t going to bring his lunch to work,” Lindsay recalled. But after working with Lindsay for more than a year, Scott said he now brings his lunch to work most days of the week. “She never said it was something I had to do,” Scott said. “It was always my decision. She’d suggest options and sometimes I liked them and sometimes I didn’t.”
Now, Scott drinks water or Sprite Zero instead of regular sodas and sweet tea, and he eats smaller portions while making better choices. “I eat more fruit now than I ever have in my life,” he said. Lindsay also suggested he use an app, Yuka, on his phone to track the nutritional value of the foods he ate so he could make informed decisions. “I love ice cream,” Scott said. “And I used the app to find an ice cream I could eat. I took the options to Lindsay and she pointed me to a Greek yogurt brand that I really like.”
The work paid off. In 2024, at his next doctor’s appointment, Scott was pleased to find that he was down 25 pounds and his A1C was a 5, well within the normal blood sugar guidelines. He is now off all his daily meds and only takes a once weekly medication to help. “I am practicing the strategies Lifestyle Medicine gave me. I’ve improved my diet, and I’ve increased my exercise. And I can see the difference in the mirror. I’m down a size in my pants and shirt. My joints don’t hurt so much when I stand up from a chair, and my vision, which I thought was an issue with my contact lenses but was actually due to high blood sugar, has improved. I just feel better.”
Scott’s co-workers also noticed changes, and some approached him about what he was doing. “They initially noticed I wasn’t going out to eat for lunch as often, so I talked with them about what I was doing.”
Scott has been doing more than just sharing information; he’s also been a key player in encouraging his team to get healthier. “Lindsay shared during one of our bimonthly meetings that they had a teaching kitchen in the Lifestyle Medicine Clinic within the Wellness Center and they wanted to have people come out and learn recipes and information about healthier meal options. I told her I’d bring my team, and that’s what I did.” Scott brought members of his grounds and parking team to the Wellness Center for an hour-long session with Lindsay, Dr. David Michael and Dr. Susan Houston, where they cooked, ate and talked about how the Lifestyle Medicine clinic can help.
“This is our Dining with a Doc series,” Lindsay explained. “Dr. Houston and I are culinary trained chefs, so she or I prepare a meal, and Dr. Michael is there, and we talk about the meal we’re making and nutrition. And then we go through Lifestyle Medicine and what we do.” The Lifestyle Medicine clinic offers the monthly Dining with a Doc program free for community members through a grant from Pitt Partners for health. As a result, Alford said other members of his team are now making positive changes and some are visiting the Lifestyle Medicine clinic.
While it hasn’t always been easy to make these lifestyle changes, Scott said they’ve been worth it. “It’s tough sometimes. Life is busy, and sometimes you just have to decide to get more steps or stand up rather than sit at your desk. But the clinic has made things easier because they give me information that’s proven to help.” And, he emphasized, seeing and feeling the difference has been key. “At first it was that 10.9 A1C that made me want to change,” Alford said. “That number really shocked me. But now I can also see and feel a difference and that’s why I want to keep doing this. It’s a conscious decision every day to make the best choices.”
Lindsay emphasized that a person knowing their “why” is very important. “We are here to support you and give you education and resources, but when you’re not here, the choice is up to you. If you know your ‘why,’ you won’t revert to old habits,” she said. Scott agreed, saying that he plans to continue practicing the new skills he’s learned the past year. “I intend to keep using these strategies,” he said. “Doing better isn’t that hard; all I had to do was ask for that support. Lifestyle Medicine has a great program, and you just have to reach out to them and take that first step.”
Both Scott and Lindsay want more people to also take that first step to learn more about the Lifestyle Medicine clinic and the services it offers. “It was incredibly easy to get started,” Alford said. “I called them and there was no excess stuff to do, no preapproval, no paperwork. It’s an easy in and out, and if you can’t make it in person, they’ll do telehealth visits.” Supporting team members in this way is very important, Lindsay said. “We want to target our team members because it benefits everyone,” she said. “Healthier team members are more productive, have fewer sick days and are generally happier. We want to expand our reach and make it more approachable.” Lindsay noted that they take various forms of insurance, and for ECU Health team members on the medical plan, they are eligible for up to six free visits with a dietitian, among other free services. “Our message is that many chronic issues like diabetes, obesity and high cholesterol can be improved by lifestyle changes and nutrition. Even if you’re not ready to make a huge change, we’re ready to meet you where you’re at.”
To learn more about the Lifestyle Medicine clinic, Leigh encourages community and team members to visit their website here or call at 252-847-5590 for more information.
Amidst the relentless demands of health care, three exceptional nurse leaders are making significant strides as leaders at ECU Health and as district representatives for the North Carolina Organization for Nurse Leaders (NCONL). Laura Respess, nurse manager of Patient Care Services, Renal Dialysis Unit at ECU Health Medical Center, Dawn Tetterton, vice president of Inpatient Nursing at ECU Health Medical Center and Jenny Parnell, manager of Patient Care Services, ICU at ECU Health Duplin Hospital, exemplify a bold, collective commitment to elevating patient care and advocating for the nursing profession statewide.
NCONL is a state-level affiliate of the American Organization for Nursing Leadership. NCONL transforms patient care and serves as a voice for North Carolina nurse leaders, aiming to shape health care through innovative and expert nurse leadership.

The organization strengthens nursing leadership through professional development, facilitates nursing research to advance practice and influences health care policy regarding the value of the nursing profession.
Laura Respess & Dawn Tetterton
Having recently concluded her term as a district representative, Respess was responsible for member communication to district VI, one of the largest districts in North Carolina. She organized quarterly meetings and planned educational sessions. She coordinated contributions for events like the annual conferences and drove the request for abstracts and Quality Initiative work from members in the region to share at the NCONL conference.
“One of the things we’ve always advocated for at ECU Health is having nurses on boards,” Respess said. “Being a representative comes with the benefits of staying informed about statewide developments and sharing best practices. As a NCONL representative, you gain a good understanding of legislative matters from the perspective of nursing, and how our profession is being represented in the legislature.”
“Through NCONL, members can showcase the excellent work being done at ECU Health,” said Tetterton, who recently stepped in to fill Respess’ role. “We submit several posters and abstracts annually and have had winners chosen for podium presentations to share nursing best practices they have developed.”
“Laura has done an amazing job,” Tetterton said, “and truly was part of the reason I felt like I needed to step forward. She has worked tirelessly the past six years, exemplifying leadership at this level.”
Respess also praised Tetterton for her leadership and is confident she will be amazing in her Regional NCONL Representative role.
“My challenge for Dawn is to drive our district’s diversification, which is one of our strategic goals,” said Respess. “We primarily focus on acute care, but we recognize the need to reach out to nursing leaders in ambulatory care and health departments across the state. It’s important to involve these sectors because they play a significant role in our overall mission.”
Jenny Parnell

Jenny Parnell was inspired to join NCONL many years ago by a nurse leader at ECU Health.
“A past nurse leader encouraged many of us to join, and throughout my time as a leader with ECU Health, it has been incredibly beneficial,” said Parnell. “I attended numerous conferences and met many leaders. In the last several years post-COVID, the organization has really come back strong.”
When a district representative position opened up, Jenny was serving on the practice committee, which focused on evidence-based practice. She wanted to take on a larger role and self-nominated for the district representative role.
“My hope is to help others grow and share things I’ve learned through the years,” she said. “Laura and I worked together many years ago on CIU as young nurses, so we’ve kind of grown up together. Even if you’re not the district representative, there are other committees that you can serve on. There are many ways to serve within the NCONL, Laura will continue to serve on the board in another role and be close by to help in our region. That’s what NCONL is all about, those nursing connections.”
Learn more about nursing at ECU Health by visiting ECUHealth.org/Nursing.
High school students from Health Sciences Academy in Duplin and Pitt counties recently had the opportunity to explore the medical field firsthand at the “Chat With a Doc” event. ECU Health physicians from various specialties engaged in candid conversations about their careers, educational paths and the realities of medical careers.
Students heard from specialties including pediatric, pathology, emergency medicine, cardiology, obstetrics and gynecology, surgery, palliative care, trauma and internal medicine. The event not only highlighted the different specialties within medicine but also underscored the commitment and dedication required to pursue a career in health care. From years of education and training to the challenges of balancing patient care with personal life, the physicians provided an honest and engaging perspective for students considering the field.
Dr. Yaolin Zhou, a pathologist at ECU Health, spoke to students about the importance of having a passion for taking care of patients when going into the medical field.

“Whatever you do within health care, you want to do what’s right for your patients, for the community, and make a difference and make your little corner of the world a better place,” said Dr. Zhou.
Dr. Zhou also described the critical role of pathology in diagnosing diseases, including cancer.
“Pathologists are trained physicians who specialize in diagnosing diseases,” Dr. Zhou said. “I examine samples from the human body to determine what’s going on.”
Dr. Nicole Toney, an emergency medicine physician, provided students with a glimpse into her field, emphasizing the fast-paced and unpredictable nature of emergency care.
“Emergency medicine is exciting because you never know what’s coming next,” Dr. Toney said. “You might see someone having a heart attack, a trauma patient, or something entirely unexpected. It’s all about problem-solving and acting quickly.”
Students in attendance found the event inspiring and informative. Kennedy Jones, a student from Duplin County, came to explore different medical career paths.
“I used to have a big interest in obstetrics, then that changed to pediatrics,” Jones said. “Hearing from a pediatrician today and learning about how they take care of the whole family when a kid gets sick was really interesting and gave me more insight into what’s ahead and helped me think more about my future.”
With the demand for health care professionals on the rise, events like “Chat With a Doc” play a crucial role in inspiring the next generation of medical professionals and helping students navigate career paths in medicine.
Despite declining cancer death rates overall, new findings from the 2025 American Cancer Society Cancer Facts and Figures reveal a troubling increase in cancer incidence among women, particularly in two key age groups: younger than 50 and 50–64. These findings highlight the importance of proactive lifestyle changes and regular screenings in mitigating cancer risks.
For women under 50, the risk of developing cancer is now 82 percent higher than their male counterparts, up from 51 percent in 2002. According to the study, contributing factors include lifestyle changes among women born after the 1950s, such as increased smoking rates, obesity and sedentary habits.

“This increase in cancer diagnoses among women younger than 50 years old is largely breast and thyroid cancers,” said Dr. Mahvish Muzaffar, a hematologist/oncologist at ECU Health. “This reinforces the critical need for routine mammograms and awareness of risk factors in this demographic. Advances in diagnostic technologies, like incidental findings during scans, have contributed to the rise in finding thyroid cancer cases.”
While lung cancer rates are declining overall, the decrease has been more significant for men than for women. In 2021 among adults younger than 65, more women were diagnosed with lung cancer than men.
“Men adopted smoking earlier but also quit sooner and more aggressively, resulting in a three percent annual decrease in lung cancer cases compared to a 1.4 percent decrease among women,” said Dr. Muzaffar. “Smoking cessation remains a crucial intervention, particularly for women who began smoking later and have been slower to quit.”
Advancements in cancer screenings and awareness campaigns have played a significant role in reducing cancer rates for some types. Prostate cancer cases among men, for instance, have declined due to more judicious use of PSA screenings. Similarly, HPV vaccination and cervical cancer screening have decreased rates of HPV-related cancers. However, some groups, particularly women aged 30–44, have seen an increase in cervical cancer incidence, potentially due to under-screening.
Dr. Muzaffar emphasized the role of lifestyle factors and screening in addressing these trends.
“The three most common cancers—breast, lung, and colorectal—all have effective screening methods,” said Dr. Muzaffar. “It’s crucial for women, and everyone, to prioritize their health, get routine mammograms and undergo screenings for these common cancers if they meet the criteria.”
As researchers continue to analyze cancer trends, further studies will be needed to explore the impact of factors like vaping, dietary habits and environmental exposures, Dr. Muzaffar noted. She also said ECU Health has observed an increasing number of younger patients with advanced cancer diagnoses.
“We haven’t conducted a formal study to compare our regional trends to national data, but anecdotally, we are seeing more young patients with cancer,” she said. “This could be an area for further research.”
The increase in cancer rates among women underscores the need for continued public health efforts focused on prevention, early detection, and lifestyle modifications. Women, particularly those over 30, should remain vigilant about their health and take advantage of available screening options to catch cancer early when it is most treatable. For more information about cancer screenings and treatment options, please visit ECUHealth.org/Cancer.
Achieving and maintaining a healthy weight can be a challenging journey, but ECU Health has resources to help with a comprehensive range of weight loss and lifestyle medicine services tailored to individual needs. Whether someone is starting their weight loss journey or seeking support to maintain progress, ECU Health offers personalized, evidence-based solutions to help people succeed.
Dr. Hannah Florida, a board-certified physician in obesity medicine at the ECU Health Lifestyle Medicine Clinic, emphasized the importance of addressing obesity holistically.
“Excess body weight is multifactorial, often influenced by unhealthy nutrition, lack of physical activity, poor sleep, unmanaged stress, a lack of support systems and substance dependence – whether that be caffeine, sugar or another substance,” Dr. Florida said. “Our approach is to meet patients where they are, assess what changes they are ready to make and guide them with the tools and accountability they need to succeed.”
ECU Health Lifestyle Medicine provides a multidisciplinary team of experts, including board-certified obesity physicians, registered dietitian nutritionists, lifestyle coaches and exercise physiologists. Together, they offer comprehensive care to address every aspect of weight management, ensuring patients receive the support they need at every step.

No two weight loss journeys are the same, which is why ECU Health offers customizable programs to fit a variety of needs:
- Medically Supervised Weight Loss: Tailored treatment plans, including lifestyle modifications and medications, prescribed by board-certified obesity physicians.
- Medical Nutrition Therapy: Personalized assessments and eating plans from licensed dietitians to support sustainable weight loss and address conditions like diabetes and high cholesterol.
- Meal Replacement Programs: Supervised liquid meal replacement plans to jumpstart progress.
- Culinary Medicine: Individual and group sessions teaching participants how to prepare plant-based meals that align with their goals.
- Pre-Surgery Optimization: Dietitian-guided programs to optimize nutritional health before bariatric or orthopedic surgery for improved outcomes.
Dr. Florida uses anti-obesity medications when appropriate to jump start patients in making lifestyle changes. These healthy lifestyle changes are the key factors to achieve sustainable long term weight loss, according to Dr. Florida.
“Medications, for example, can temporarily suppress appetite, but lasting results require adopting healthier habits,” she said.
Lifestyle coaches at ECU Health help patients set and achieve specific goals, such as improving sleep, managing stress, or incorporating regular exercise.
“For instance, if someone struggles with getting enough sleep, the coach might help them set small, actionable goals like limiting screen time before bed,” Dr. Florida said.
Exercise physiologists at ECU Health further support patients by creating personalized exercise plans. These programs often begin with one-on-one guidance and transition patients to sustainable fitness routines, whether through gym memberships or at-home activities.
Addressing obesity not only improves physical well-being but can also alleviate related chronic conditions such as diabetes, hypertension, chronic pain, and kidney disease.
“When we treat obesity, we often see significant improvements—or even reversal—in these chronic conditions,” said Dr. Florida.
ECU Health’s Lifestyle Medicine Clinic offers flexible options for individual appointments, group-based education, and cutting-edge culinary medicine.

“Our goal is to meet patients where they are and empower them to make sustainable changes,” says Dr. Florida.
For some individuals struggling with weight-related health issues such as diabetes, heart disease, high blood pressure, arthritis and sleep apnea, bariatric surgery may be the most effective solution.
ECU Health Medical Center offers advanced surgical options, including:
- Gastric Bypass: Reduces the amount of food you can eat and the calories you absorb by creating a small stomach pouch that connects to the small intestine. This helps you feel full faster and absorb fewer calories.
- Sleeve Gastrectomy: Removes up to 85% of the stomach, creating a sleeve-like structure that holds less food and reduces hunger hormones.
Bariatric surgery often results in greater weight loss compared to medical treatments alone and can significantly improve chronic conditions linked to obesity. While surgery is highly effective, it is not without risks, including bleeding, infection and nutritional deficiencies. Speak with your primary care provider to learn if this option is right for you.
Ready to Begin Your Journey? Take the first step toward a healthier you with ECU Health. To learn more about ECU Health’s weight loss services at the ECU Health Lifestyle Medicine Clinic or to schedule an appointment, visit the ECUHealth.org/LifestyleMedicine or call 252-847-9908.
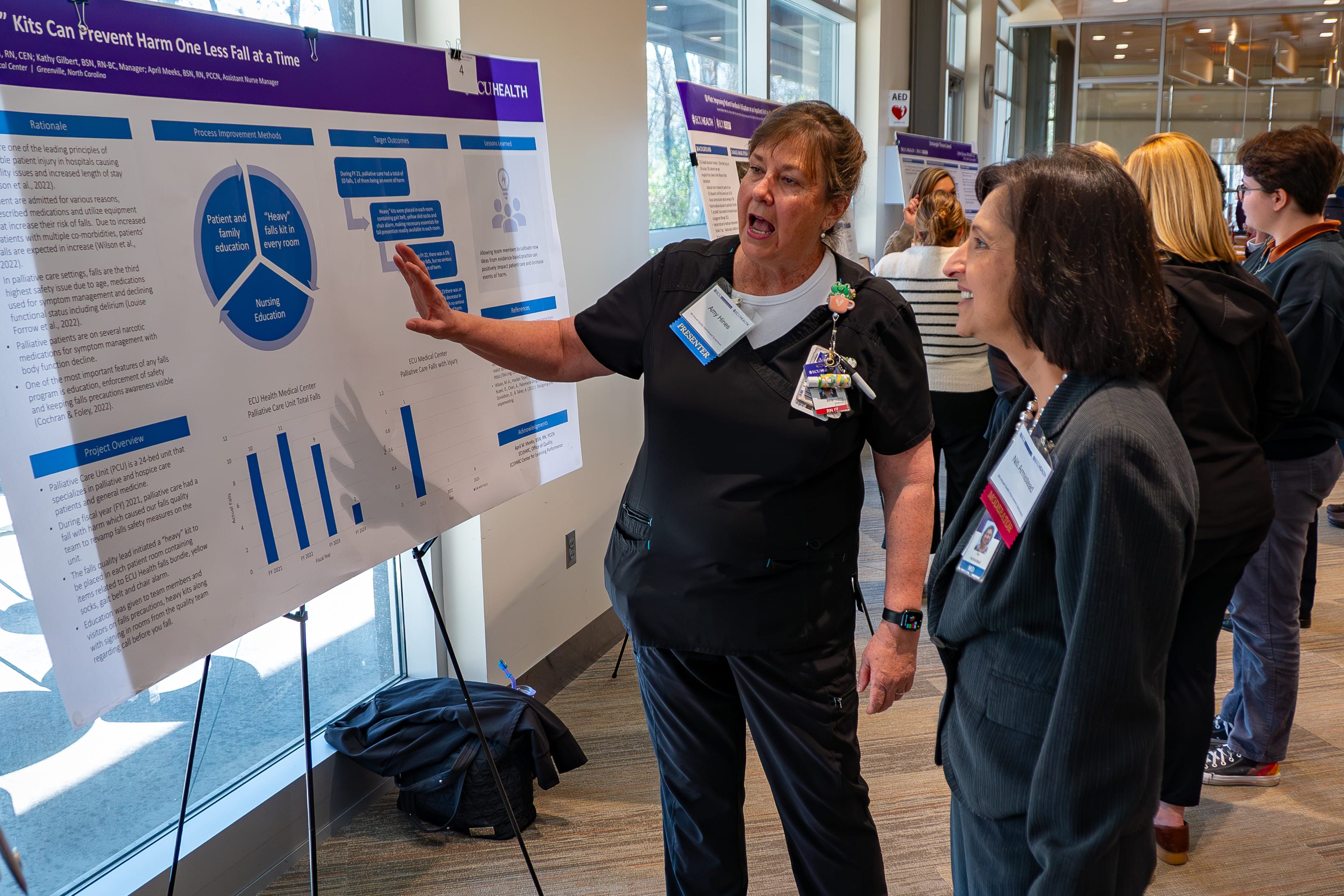
A multidisciplinary group of physicians, health professionals, care teams, residents, fellows and students came together Wednesday for the 9th annual ECU Health Quality Improvement Symposium at Eastern AHEC. With educational sessions, a keynote speaker, podium presentations and a poster session, the day was jam packed with quality improvement initiatives and ideas from across ECU Health and East Carolina University’s Health Sciences Campus.
Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine, provided opening remarks at the symposium and reflected on his personal journey in quality improvement, which began 35 years ago and continues today.
“And in that 35 years, so much has changed, but really so much hasn’t changed. The essence of collaboration and caring and love is the essence of quality,” said Dr. Waldrum.

“The fact that you all care about your environments and each other and the patients we serve is what inspired me 35 years ago. Now, with changing technologies like artificial intelligence and other impacts to the care environment, the essence of quality, caring, taking care of each other and loving each other has never been more important. Thank you for doing that and carrying that message out for our organization, working in your units every day and living our values. That is who we are at ECU Health as we create the model for rural health care and educate the future health care professionals.”
Dr. David Tillman, chair of the Department of Public Health at Campbell University, provided keynote remarks to the group of 143 in-person and 63 virtual attendees. His presentation, “Rooted in Rural: Enhancing Patient Care and Quality Improvement by Valuing the Rural Context,” focused on understanding how engagement with rural communities provides essential insights for effective and empathetic health care.
“I’m based at Campbell and get to work closely with the communities in eastern North Carolina as do so many of the attendees here, and so often the rural context is forgotten in the broader quality improvement context,” said Dr. Tillman. “Having this topic as the keynote puts ‘rural’ at the center of quality improvement efforts. You can’t just replicate quality improvement efforts in rural communities. Instead, you have to think deeply about how it applies.”
The symposium showcased more than 40 projects related to system improvement, practice redesign and other methods for improving quality within health care and here in eastern North Carolina. The projects, categorized into podium presentations, poster presentations and works-in-progress presentations, offer a snapshot of ECU Health and the Brody School of Medicine’s commitment to driving continuous quality improvement across the health enterprise.
Awards for the top podium and poster presentations were announced following the showcase.
Podium Presentation:
Outstanding Podium Presentation: Michelle Ball, MSN, RN, CCRN-K, CIC, Infection Prevention, ECU Health Medical Center – “Standardization of Skin Antisepsis for Hip Replacement Surgery
Honorable Mention Podium Presentation: Dr. Nusiebeh Redpath, Perinatal-Neonatal Medicine, ECU Health Medical Center – “Increasing Parenting Activities in the NICU by Parents with Very Preterm Neonates”
Quick shot podium presentation:
Outstanding Quick Shot Podium Presentation: Alissa Meyerhoffer, MS2, LINC Scholar, Brody School of Medicine, ECU – “Improving Patient Throughput at the ECU Health Pediatric Specialty Clinic”
Honorable Mention Quick Shot Podium Presentation: Pankti Sheth, MS4 LINC Scholar, Brody School of Medicine, ECU – “Timely Extubation in Low-Birth Weight Preterm Infants Using a Standardized Protocol”
Honorable Mention Quick Shot Podium Presentation: Dr. Greeshma Sheri, Department of Internal Medicine, Brody School of Medicine, ECU – “Improving Inpatient Sleep Quality”
Poster presentation:
First Place Poster Presentation: Mariam Tariq Awana, MD, Internal Medicine and Pediatrics, Brody School of Medicine, ECU – “Enhancing HIV PrEP Prescription Adherence through Physician Education and Assessment”
Second Place Poster Presentation: Aimee Dunn, BSN, RN, CCRN, SCRN, Neurosciences Intensive Care Unit, ECU Health Medical Center – “Targeted Interventions for CAUTI Prevention: A Success Story in Reducing Infection Rates in the NSICU”
Third Place Poster Presentation: Missy Barrow, MA, LSSGB, Internal Medicine Community, ECU Health Medical Center – “Communication Between Hospital Allied Health and Primary Care Practitioners: A Collaborative Approach to Improving Hospital Discharge Summaries”
Dr. Jennifer Sutter serves as the current physician director of the Quality Improvement Symposium, helping presenters with their projects and supporting the judges as they review each body of work. But it wasn’t long ago that she herself was standing at the podium presenting her quality improvement work. The experience, she said, can benefit health care professionals in powerful ways.
“As a presenter, it can be nerve wracking to put yourself out there, but you get so much great feedback that can help you move your project forward,” Dr. Sutter said. “From my standpoint now, it’s great to create this environment where that learning and growth can happen. It takes a team to do quality improvement, and we have people here from across the health system who are collaborating to do just that. There’s nothing better.”
The day closed with two educational sessions designed to help those in attendance take the day’s learning and apply it to their mission-driven work.
Erika Taylor, clinical faculty member and instructor in the Division of Behavioral Medicine in the Department of Family Medicine at the Brody School of Medicine, and Patricia Huerta, clinical assistant professor in the Department of Family Medicine at the Brody School of Medicine, hosted “Dialectical Behavior Therapy Skills for Medical Providers” to encourage health care providers to engage with a variety of coping skills to support their mental health and the mental health of their patients.
Randy Cobb, director of Talent Development at ECU Health, led a session called “Leading Change: Two Success Factors” where participants explored the importance of leading people through change by crafting a change plan via an interactive experience.
To learn more about the symposium and view a list of presentations, please click here.
Dr. Jonathan Hamilton, chief of urology at ECU Health, was recognized with the Patriot Award, an honor presented by the Employer Support of the Guard and Reserve (ESGR) that underscores Dr. Hamilton’s exceptional support for military personnel and their families.
This award reflects the vital role Dr. Hamilton has played in fostering a supportive environment for team members who serve in the National Guard and Reserve, as well as their loved ones. The award highlights efforts such as granting time off prior to and after deployment, accommodating flexible work arrangements, providing leaves of absence as needed and assistance to military families.
“I am truly honored to receive this award,” said Dr. Hamilton. “As someone deeply patriotic, with both of my grandfathers having served in World War II, I’ve always believed that service takes many forms.

While my path has been different, I feel it’s my duty to support those who serve our country. Dr. Hugh Mallory Reeves is not only a great friend and colleague, but also a true patriot who has made tremendous sacrifices for this nation. It’s a privilege to support him as he fulfills his duty to our country.”
Dr. Hugh Mallory Reeves, a urologist at ECU Health who also serves as a lieutenant colonel in the Army Reserves, nominated Dr. Hamilton for the Patriot Award in recognition of direct and meaningful support. Dr. Reeves, one of only a few urologists serving in the Army Reserves, has balanced his dual careers since 2003 with significant support from Dr. Hamilton and ECU Health.
“ECU Health supports veterans and appreciates their service,” said Dr. Reeves. “If it weren’t for an entity like this and people like Dr. Hamilton, we wouldn’t be able to be here with long careers as physicians and military service.”
Retired Navy Cmdr. Ken Oppenheim, a representative from the ESGR, alongside Dr. Reeves, formally presented the award to Dr. Hamilton, providing an opportunity to celebrate his impactful contributions and recognize the ways he has supported service members and their families.
“ECU Health has always been a strong advocate for serving veterans and supporting our military,” said Dr. Jason Foltz, chief medical officer at ECU Health Physicians. “Dr. Hamilton’s commitment to accommodating physicians currently serving in the military is integral to who we are.”
Anthony Bartholomew, vice president of operations for ECU Health Physicians, echoed these sentiments.
“Dr. Hamilton is a remarkable leader who supports all of his team members – military and non-military – in every way possible,” said Bartholomew. “It’s an honor and a privilege to have someone so dedicated to eastern North Carolina and our patients as part of our team.”
Dr. Hamilton’s nomination was reviewed and approved by the ESGR state committee. The North Carolina ESGR is a Department of Defense office led and operated by volunteers who aim to foster supportive work environments for members of the National Guard and Reserve.
An ordinary day in Greenville, North Carolina, became unforgettable when a health care worker and a cardiac arrest survivor were brought together by a twist of fate. Years after Vicky Greco performed CPR on Tony Parker when he collapsed from cardiac arrest during a race, the two were finally reunited and reflected on that fateful day.
In 2021, Greco and her daughter found themselves at Town Common in Greenville, a location they did not typically visit. As her daughter played on the playground, a commotion near the finish line of a local 5K race caught her attention.
“We usually go to Peppermint Park,” Greco recalled. “But for some reason, we decided to go to Town Common that day.”
As Greco’s daughter played on the playground, she noticed a commotion.

“She said, ‘I think someone needs help, Mom,’” Greco said.
That someone was Tony, who had collapsed suddenly in cardiac arrest. His wife, Delia Parker, a trained dental assistant with CPR certification, had already started chest compressions when Greco arrived.
Without hesitation, she stepped in to assist. As manager of the Pediatric Day Medical Unit at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center, Greco had experience performing CPR. Together, they worked tirelessly until emergency responders arrived.
“It was a miracle to be there, to have the training and to have the outcome we did,” Greco said. “It’s something I’ll never forget.”
A previous ECU Health News story shared Tony’s inspiring story and his recovery experience with ECU Health Heart and Vascular Care. At the time, Tony and Delia did not know who the person was that stepped in to perform chest compressions. They called the unidentified person their “angel.” After seeing the story, Greco reached out to identify herself.
Over three years later, Tony and Greco were finally able to meet under much happier circumstances. The reunion was deeply emotional, with Tony expressing heartfelt gratitude for Greco.
“Today, God revealed our angel,” said Tony. “If it weren’t for Vicky and Delia, I wouldn’t be here today. It’s amazing how everything aligned.”
For Greco, the encounter affirmed her faith in being at the right place at the right time.
“I’m thankful that God put me there that day,” she said. “The outcome was nothing short of amazing.”
Motivated by their experience, Tony and Delia Parker have since joined forces with organizations like Greenville Fire and Rescue and the Compress and Shock Foundation to promote bystander CPR training. Together, they visit local churches, community centers and underserved areas across eastern North Carolina to emphasize how simple actions can save lives.
“We teach people that you don’t need to be certified to make a difference,” Delia explained. “It’s about empowering others to act.”
The Parkers continue to share their story, inspiring communities to act in moments of crisis.
“Nearly 90 percent of out-of-hospital cardiac arrest victims do not survive,” Tony said. “Even with help, survival is only about 30 percent, but without it, it’s almost zero. Every second counts, and timely intervention can significantly increase survival rates.”
According to the American Heart Association, if performed immediately, CPR can double or triple the chance of survival from an out-of-hospital cardiac arrest.
Tony has also become an advocate for greater access to automated external defibrillators (AEDs) and the use of road identifications for athletes.
“I encourage everyone in my running and biking groups to wear one,” he said. “It can be a lifesaver.”
Following his recovery, Tony has embraced life with renewed purpose.
“Life is good,” he shared. “Even with a cardiac issue, you can still enjoy life. This experience taught me that every moment matters.”
Their story stands as a testament that heroes often emerge in unexpected moments, and that simple acts of courage and compassion can change lives forever. Their journey continues to inspire others to learn, act and save lives.
To be a health care provider is to answer a calling. For some, the journey to health care is a straight line; for others, the road is winding. This series features stories from ECU Health team members who took the winding road, but found the destination to be worth the effort.
When Deborah Rice, a staff nurse III on the palliative care unit at ECU Health Medical Center, was 13, her father died; this changed the trajectory of her adult life. “As a young girl, I knew I wanted to be a nurse,” Deborah shared. “But when my father was killed, I didn’t feel like I could put the financial burden on my mother, or leave her home alone with my younger brother, so when it was time for me to go to college, I didn’t go.”
Deborah got married and had children, and for 20 years she worked at a bank as a database analyst.
Then she learned her department was being let go, and she found herself at a crossroads. “My husband asked me if I still wanted to be a nurse, and I said yes.”
Around the same time, Deborah found herself dealing with the illness and death of several family members. “In 2008, my stepfather died from bone cancer, and from that point on for the next two to three years, we lost about five or six others in my family,” she said. “I had a hand in taking care of them when they were in their last days, and it just solidified for me that nursing was where I needed to be.”
With the support of her husband, children and mother, Deborah made the decision to pursue her dream of becoming a nurse. She first earned? her certified nursing assistant (CNA) and applied to nursing school at Edgecombe Community College, and at age 48, she graduated with her associate degree in nursing (ADN). She then went on to East Carolina University to get her bachelor of science in nursing (BSN). After graduation, Deborah knew exactly where she wanted to work. “When I was in nursing school, they were getting ready to build the Cancer Center, and I always said that was where I wanted to work.”
It took some time, but Deborah landed her dream job and now works in the palliative care unit. “It’s a special group that I work with,” she said. “It’s about helping a patient die with dignity and respect. Not everyone has a family, so we are there with those who are alone as well as those with lots of family. And we take care of the patient and their family, helping them get through this difficult time.”
The work is rewarding, but Deborah acknowledged it’s not for everyone. “It takes a special kind of person, somebody with compassion and empathy, because it’s not easy taking care of people who die and their families. But we talk with them and spend time with them, helping them accept what’s going on. You’ve got to love what you do, and our team does.” Not only do they love what they do, but the team supports each other when things get tough. “If we need to go into a room and cry, we go cry. We cry with each other, and we laugh and joke. We have to do all these things to survive.” That level of support is important to Deborah. “My team is very supportive. I wouldn’t work anywhere that didn’t have good teamwork, because that’s what gets you through the day. It encourages us to go forward and do and learn more.”
It’s equally gratifying to make connections with the patients and their families. “I tend to bond with my patients. I keep in touch with some of the family members. They’ll reach out to me from time to time to ask how I’m doing. It’s so great to build those relationships and help people through those times,” Deborah shared.
It’s clear when you talk with her that Deborah loves her work. “It’s been an experience of a lifetime, and it’s one I continue to learn and grow in. There’s never a dull moment. I love oncology and palliative or hospice care, and I keep learning and encourage everyone to keep learning. Love what you do and learn every chance you get.” She also was recently recognized as a Great 100 Nurse of North Carolina, yet another signifier that she is exactly where she should be.
To anyone thinking about starting their nursing career later in life, Deborah quickly offers reassurance. “I’m glad I did it. Even at 48 years old, I wouldn’t change a thing. I try to instill in everyone I meet that you’re never too old to go to nursing school. Even if school is challenging, I say keep going. And if you don’t succeed the first time, but it’s what you really want to do, don’t ever stop,” she said. “I hear people say they would go back to school but they’re 36 and will be 40 when they’re done. I say, you’re still going to be 40; you might as well put that time to good use.”
And Deborah has certainly put her time to good use. “Being a nurse has been the biggest blessing of my life,” she said. “My husband and my mom were my biggest fans. I wouldn’t be who I am today without my mom because she raised me from the time my father was killed. And if my dad was alive, he would be very proud of me. I did it for him as well because I knew he would want me to do it. It was not an easy thing to wait until I was 48, but it was well worth it.”
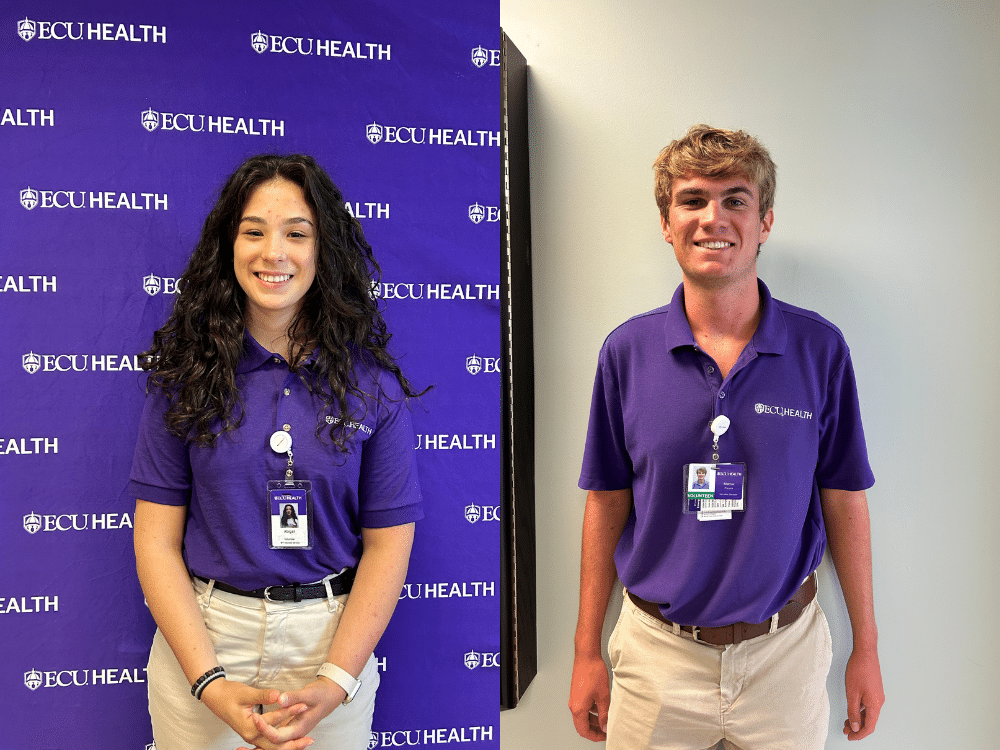
The ECU Health Volunteen Summer Program is designed to teach students ages 15 to 17 the value of community service and to provide experiences that foster growth and maturity. The program also provides an opportunity for the students to learn about and explore health care careers. Mattox Piscorik, a senior this year at D. H. Conley High School in Greenville, and Abigail Williford, a junior at the North Carolina School of Science and Mathematics in Durham, have both served as Volunteens at ECU Health Beaufort Hospital, a place where they enjoyed working in a small, family-like community.
Mattox Piscorik
For Mattox Piscorik, ECU Health is a family affair. His entire family works in health care in some way, making it natural for him to also choose a career path in the field.

“My mom’s a nurse at ECU Health, my sister-in-law is a cardiovascular sonographer, my brother is an ECU dental school student, and my other brother is in pharmaceuticals,” he laughed. “I even recruited my grandmother to be a NICU volunteer. I grew up in health care and I love it.”
His brothers also both served in the ECU Health Volunteens program, which sparked Mattox’s interest in volunteering at the hospital when he got old enough to do so. He began at the ECU Health Medical Center, but this past summer he spent time at ECU Health Beaufort Hospital. That’s where he got the idea to pursue a career as a hospital administrator. “I thought I wanted to be an emergency department (ED) doctor,” Mattox explained. “But after starting the Volunteens program and talking to Dr. [Dennis] Campbell (president of ECU Health Beaufort Hospital) this past summer, I fell in love right then and there with health care administration. I want to work at ECU Health and give back to the families in need in eastern North Carolina.”
While Mattox enjoyed his experience volunteering at the ECU Health Medical Center, which offered many opportunities to learn, he said he especially enjoyed the small community setting at Beaufort. “Everyone knows everyone, and you get to know the patients and their families. I wanted to make a strong connection and impact that community,” he said.
While at Beaufort, Mattox said he worked in the ambulatory surgery unit (ASU) taking patients to pre-op and then back to their cars after surgery. He also worked in the hospital lobby greeting patients and families and helping them find where they needed to go. “I also shadowed an ED doctor, and it was so awesome to see exactly what nurses, physician assistants, doctors and the others do in that setting,” he said.
This type of work is extremely gratifying, said Mattox, especially considering he’s seen the hospital from a patient’s family member perspective. “My dad had a couple of cardiac events and was in the hospital,” he said. “I got to see things from that side, and it showed me that these families need someone to show them compassion.”
That patient and family interaction is what Mattox enjoys the most. “You don’t know what they’re going through, and just being able to put a smile on their face and give them someone to lean on means a lot. Everyone comes together at the Medical Center and Beaufort, and it’s a team effort to provide care for eastern North Carolina. This includes the volunteers, and it means I can make an impact.”
Abigail Williford
Abigail Williford is a Chocowinity native who plans to attend medical school. She’s known for much of her life that she wanted to work in health care, in part because of her own experience as a patient at the ECU Health Medical Center. “I was born 10 weeks early and was in the NICU,” she shared. “Every year we go to Greenville and take the NICU a cake and a card to show our appreciation for them and what they do.” Her specific area of interest has evolved over time, from a neonatologist to a surgeon; but whatever she chooses, Abigail said it’s always medicine and she wants to give back.
That’s why being a Volunteen at ECU Health Beaufort Hospital made sense. “My mom heard about the program and she told me about it. I thought it sounded interesting and have been doing it for two years now.” Abigail opted to serve at Beaufort Hospital. “It’s smaller and that was better for me starting out,” she said. “Starting in a smaller community lets you get your bearings, and I plan to go back next year.”
Abigail said it’s the people that keep her coming back. “Everyone is so nice. You’re welcomed there, and everyone is willing to give you opportunities to help and learn.” Some of the services Abigail has provided include taking phone calls, delivering meals and flowers, working the front desk and signing people in, running wheelchairs to various parts of the hospital, helping in the ASU and directing people to where they need to go. “It’s cool to hear the patients and families tell their stories. I try to bring joy to their lives and it’s great to see their happy faces.” She also had the chance to observe a few surgical procedures, and some of her time volunteering in cardiac rehabilitation gave her the chance to see patients work hard to recover.
This experience has taught her that you never know what people are going through. “You might look at someone and wonder why they are so upset, but then you realize they have something serious going on. You have a choice to be a light in their day.”
Angelina Brittle, the manager of volunteer services at ECU Health Beaufort Hospital, sees the Volunteen program as a great way for teens to connect with their community while gaining valuable skills. “The Volunteen program provides a meaningful opportunity for students to experience the health care environment firsthand,” she said. “At ECU Health Beaufort, we see incredible value in offering these experiences, not only to help teens explore potential career paths, but also to foster personal growth, teamwork and a spirit of giving back. Volunteering in a health care setting allows them to connect with their community in a unique way, leaving a lasting impact on both the teens and those they serve.”
The process to apply to be a Volunteen is easy, and both Mattox and Abigail encourage any students interested in working in a hospital setting to apply. Applications for the 2025 program, which runs from mid-June to the beginning of August, open in January 2025, and students can volunteer at ECU Health Medical Center, Beaufort, Duplin or Edgecombe. Due to an increased interest in the program, applicants are encouraged to apply as soon as the application opens. To learn more about the Volunteen program and to apply online in January 2025, visit ecuhealth.org/volunteers/#Beaufort or email Angelina Brittle at [email protected].