In a ceremony laced with excitement, anticipation and tradition, fourth-year medical students in the Brody School of Medicine at East Carolina University learned where they will spend the next three to seven years completing residency training.
The March 17 event marked a milestone for the Class of 2023, whose medical school journey included the historic events of learning through the COVID-19 pandemic and the integration of Brody and then-Vidant Health, which became ECU Health in 2022.
Match Day is arguably the pinnacle of medical school, when students discover their next destination surrounded by friends, family and Brody faculty and staff who have guided them over the years. Michael Waldrum, dean of the Brody School of Medicine and CEO of ECU Health, said that wherever the students are matched, they already have a reputation of being health care providers who put the individual patient at the center of their practice.

“Brody students come out of medical school knowing how to do hard work and take care of humans. It’s a very hands-on practical education. They learn how to take care of people which is what becoming a doctor is all about, and the experience they get here sets them apart,” Waldrum said.
The students were presented to the audience of family, friends and members of the Brody community with collages of photos along with music that each selected.
Kari Beasley, from Cary, wanted to use the song “Soulful Strut” from the movie “The Parent Trap” — but only if one of her mentors, Jason Higginson, agreed to learn the handshake from the movie and perform it on stage with her.
Beasley, who matched with Virginia Commonwealth University in Richmond to pursue an obstetrics and gynecology track, said that both Jason Higginson, the executive dean of Brody, and his wife Amanda Higginson, Brody’s interim associate dean for student affairs, were an important part of her medical school experience.
“Being the amazing dean that he is, he said, ‘Of course, absolutely, I’ll do the handshake with you.’ Today, we pulled it off,” Beasley said. “It made it more special that he and I got to do the handshake together because the Higginsons have been a great part of my experience here at Brody.”
While Higginson had seen the movie, he didn’t remember the handshake and dance until she showed him the clip.
“She asked me if I would do it with her and I said you’re really challenging an old man with no rhythm. We practiced it yesterday in my office and then I practiced it with my daughter all night last night,” Higginson said.
The relationships that he and fellow faculty members build with their students is unique because he didn’t have interactions with the administration when he was in medical school.
“This is probably one of the best days in the life of a medical school. This is the day where all of your dreams get realized,” Higginson said. “A lot of them are staying here, which is something we are proud of. Almost 50 percent of the class is staying in North Carolina and that’s fantastic. That’s our mission.”
The Class of 2023 is a snapshot of Brody’s mission to serve the state. The 77 members of the class represent more than 25 North Carolina counties, from Buncombe in the west to Pasquotank in the northeast.
With envelopes in hand that revealed their futures, the students took time to celebrate their accomplishments and reflect on what comes next.
‘What small change can I do?’

When there’s a problem, Merdi Lutete is busy seeking a solution.
Lutete, who was born and raised in Kinshasa, Democratic Republic of Congo, has the mindset of not standing by and expecting others to act — instead, she wants to know how she can help and how her skills and knowledge can lend to a long-term resolution.
“With a lot of issues we encounter, we see a problem and we say, ‘Well, someone else can do it,’” she said. “What’s helped me has been that mindset of, ‘Well, there’s a problem. What can I do about that? I’m probably not even going to get to the surface of the issue, but what small change can I do for this?’”
Lutete has used that formula throughout her life, including medical school. Lutete founded I Am First, an organization that partners first-generation medical students with mentors who can guide them through the medical school process.
“I think it will definitely contribute a lot,” she said. “I was able to apply it to school and I can put it to other areas too, and medicine as well.”
Lutete matched in adult neurology at Duke University Medical School in Durham. As she opened her Match Day envelope, she was surrounded by family and friends, some whose smiles shown through phone screens. Her hands shook as she revealed the folded paper printed with her next destination.
“I was nervous,” she said, laughing as those around her cheered, “but I feel good.”
Lutete studied neuroscience at ECU during her undergraduate years; she initially became interested in neurology in high school, when she took a psychology course and witnessed her father face a health challenge. His doctor was careful to include the family in medical conversations and make sure they understood the situation and options.
“That personal thing really touched me a lot,” she said. “I really wanted to do something like that with patients as well.”
Seeing her own family go through a health challenge and now having the perspective of a student doctor helped Lutete better understand the sacrifices her family and community have made to help her get where she is today. Her parents moved the family from Kinshasa to Raleigh in 2005 to pursue more opportunities. The Congolese community in Raleigh has also rallied behind Lutete and her success. Lutete worked with other students and Brody faculty and staff on an initiative to share information with the families of medical students so that they better understand the process their students will experience in the coming years. It was her way of acknowledging the village that it takes for students to succeed.
“It truly means a lot to them and a lot to me to see that,” she said of the support she’s received from those around her. “One thing about first generation that I really think is powerful is that you’re standing on the backs of many people’s sacrifices. You know that the successes you have you can’t attribute to yourself because you know every single person had a role in that. You’re literally standing on the backs of other people’s sacrifices.”
When Lutete thinks about community, she thinks about how Brody has prepared her for her next steps.
“Brody does a great job of teaching you how to care for the individual, how to care for the patient that you’re seeing in front of you,” she said. “I can give you a prescription for medication, but can you afford it? I can tell you to come back next week for an appointment, but can you afford to come back? Brody really teaches you how to think about the patient and how their story applies to the situation.”
Success found through love, teamwork

When you start off down an arduous path, it’s good to have a friend by your side. When that friend ends up being the person you fall in love with and plan to keep walking life’s paths hand in hand, all the better.
The first week of classes at the Brody School of Medicine in the fall of 2019, Bethany Laden and Caleb Oakley were out with mutual friends working through the awkwardness of meeting the classmates you’ll share the next four years with. He bought her a drink, she told him her favorite book was The Great Gatsby (from which he quoted the last line — smooth) and Bethany said, “we’ve been together ever since.”
Laden was raised in an Air Force family and lived in England and Guam, but mostly in Harrisburg, near Charlotte. She studied biology at NC State and initially intended to apply for a physician assistant program but applied to Brody after graduation. She spent a year as a medical assistant and two years of conducting urology research in Durham. Witnessing a baby being delivered set her mind to being an obstetrician and gynecologist.
“I really like working with my hands — being in the operating room and doing surgery. When I was on my women’s health rotation that’s where I found my passion — working with women, empowering them through their pregnancies and the rest of their lives,” Laden said.
Oakley is from Roxboro and knew he wanted to be a doctor since high school. A teacher showed the movie “Chernobyl Heart,” which chronicled missionaries who fixed the cardiac conditions faced by children who were affected by the Chernobyl disaster. Oakley’s family was particularly religious and did missionary work along the east coast and the film inspired him to be the same kind of doctor who helped people who needed the most help.
He worked as a medical scribe in high school, and then again during his undergraduate education at ECU, where he double majored in biology and chemistry. His first application to medical school didn’t work out, so Oakley taught as a substitute, trained to be a paramedic, worked on food trucks across eastern North Carolina and even prepped alligator meat at a seafood company in Morehead City.
Oakley’s intended career path lies at the other end of the birthing process from Laden. As a doubled-board certified doctor working in internal medicine and pediatrics, he’ll be able to treat patients across the continuum of birth to death.
“They tell you when you start medical school that you’ll find your niche. I had a really good experience out at ECU Health-Duplin which confirmed it for me,” Oakley said.
Early in their relationship they agreed that school would come first and “I’m not going to let you distract me,” Laden remembered. But before long, when she finished studying at 11 p.m., she would try to track him down in the Brody building.
Their relationship took some work, because relationships on their own are difficult Oakley said. Layering the physical, mental and emotional challenges of training to be a doctor on top of creating a new life with another person makes things even more challenging, but with great challenges come great rewards.
“I don’t say this all the time, but she’s my rock. If I feel I need to lean on somebody, I’m going to her,” Oakley said.
Laden agreed. Having someone in her corner, someone who understands the specific challenges of medical school, has been invaluable.
“There’s so much that we go through that people don’t understand,” Laden said. “Not just the logistics of how medical training works, but the terminology and the emotional work that you have to do.”
Match Day is incredibly stressful for any medical student — will you get the hospital you want? Will it be on the other side of the country? For a soon-to-be-married couple, the stressors compound — would they be assigned to hospitals close together or separated by circumstance?
Laden and Oakley interviewed at more than a dozen of the same hospitals to find a place that could support both of their training paths. When they opened their envelopes, surrounded by their families, the learned their residency would take place at ECU Health Medical Center in Greenville.
“Both of our families live in North Carolina, so we don’t have to worry about moving and we’ve already set up a good sense of community,” Oakley said. “It feels like home.”
The art of emergency medicine
Andrés Gil had graduated from Winthrop University in South Carolina when he came upon an opportunity to be a medical interpreter at a hospital near Charlotte.
The talented violinist was preparing to audition for orchestras and embark on a classical music career when another type of art caught his eye. During his experience as an interpreter, he witnessed a baby being born.
“I remember I was interpreting, the lights were down in the room, it was the early shift so the sun was a nice orange glow lighting up the whole room, and everything was going well,” Gil said. “All of sudden you just hear this cry. It was like art. Watching life come into the world was amazing.”
Gil, who was born and raised in Colombia, made his way to the Brody School of Medicine from there, after selecting the school based on its small class size and its community focus. After realizing he was on the path of his purpose, he began to immerse himself in service and making a difference in others’ lives.
“I never pictured myself as a student doctor in eastern North Carolina,” he said. “It was just never on my radar.”

Gil has flourished, becoming close with his classmates and being inducted into the Gold Humanism Honor Society, a community of medical students, physicians, and other leaders who have been selected by their peers for their compassionate care. Gil was surprised to be named to the group but wants to continue on the path that earned him the recognition.
“The people I get to share that honor with are all beautiful human beings,” he said. “I like having that in my wheelhouse for others to know that this is an opportunity to highlight your career.”
Gil matched in emergency medicine at Carolinas Medical Center in Charlotte. When he opened his Match Day envelope, tears filled his eyes and he couldn’t speak. A tight circle of family members teared up as well, cheering when he was able to reveal his next stop.
“Charlotte?!” a colleague passing by exclaimed.
“Yes, yes!” Gil nodded, overcome by a fresh burst of tears.
Emergency medicine felt like the right fit for Gil, who has learned to temper his expectations as he went through medical school, hoping for the best but understanding that contingency plans are important to have in place. The specialty also drew him in because of his overwhelming passion for helping people and healing patients who seek him out for assistance.
“Anyone who comes through those doors is not at a great point in their life,” he said, “whether they have pain, addiction, substance abuse, a car accident or things aren’t great at home. These people humble themselves enough to come and seek our help. Knowing that I have an opportunity to somehow have an impact on their lives moves me to a degree that I really can’t describe.”
As Gil prepares to leave Greenville and head west for the next chapter in his story, he hopes that what he’s learned at Brody will help add vitality to his patients’ stories as well.
“An opportunity to give someone grace, to restore their dignity, is so important to me,” he said. “It makes all the scary things about emergency medicine go away. That moment gives you an impetus to work harder to restore this person, so when they leave, they can go back to their life and complete their narrative.”
Read more from ECU News Services.
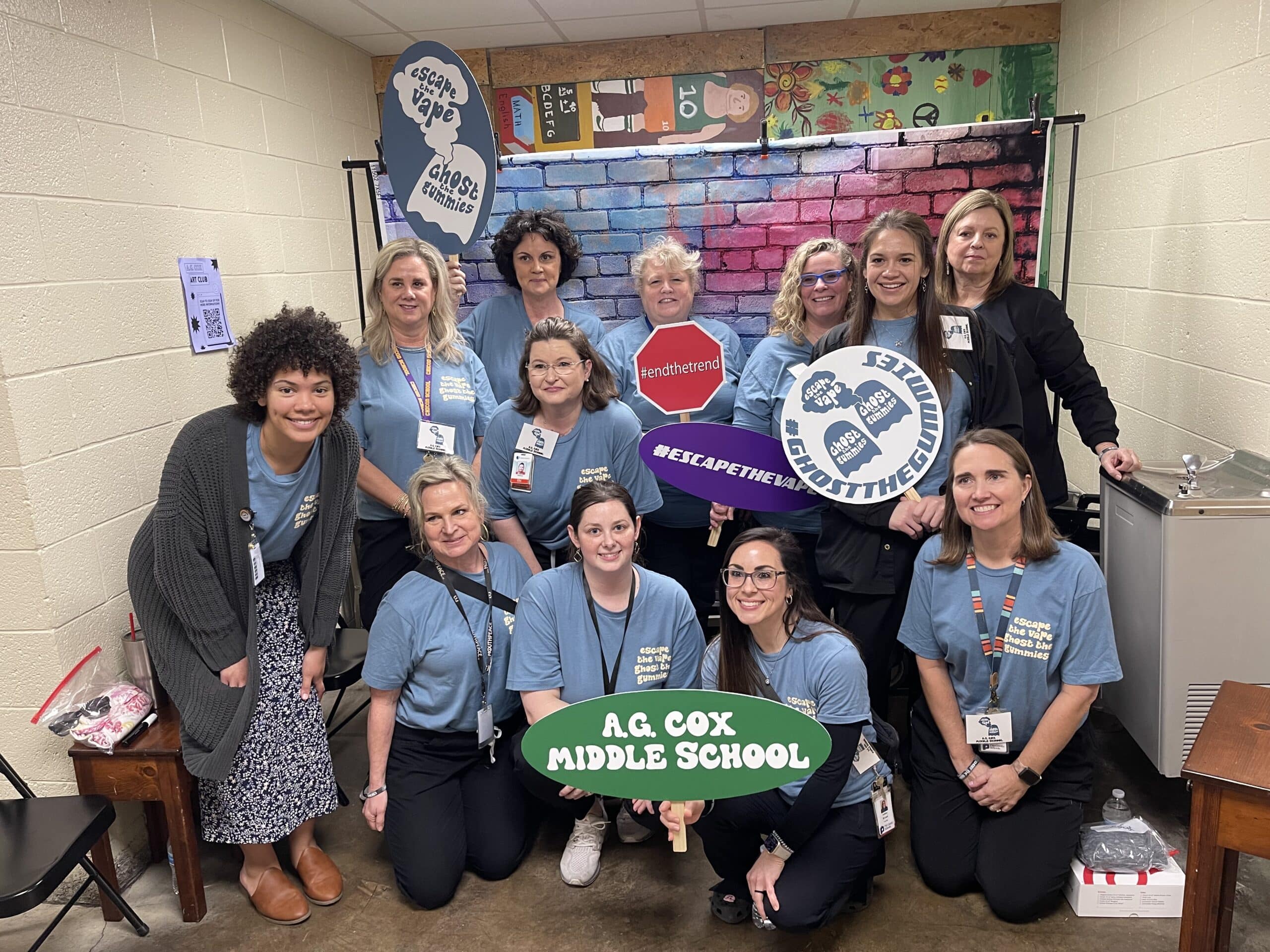
Students at A.G. Cox Middle School in Winterville learned about the dangers of vaping tobacco or other substances and drug use during an event hosted at the school on Feb. 28.
Pitt County School nurses, ECU Health team members and volunteers, and local high school students acted out two different scenarios for the A.G. Cox students, who are in grades 6-8, to show how quickly things can go wrong.
In one scenario, a student at a party takes a gummy from a friend, which turns out to be laced with drugs. The student then falls critically ill from the effects of the drugs.
In another, a student is taken to the hospital after using a vape they were told did not have tobacco in it, but instead was filled with an unknown drug.
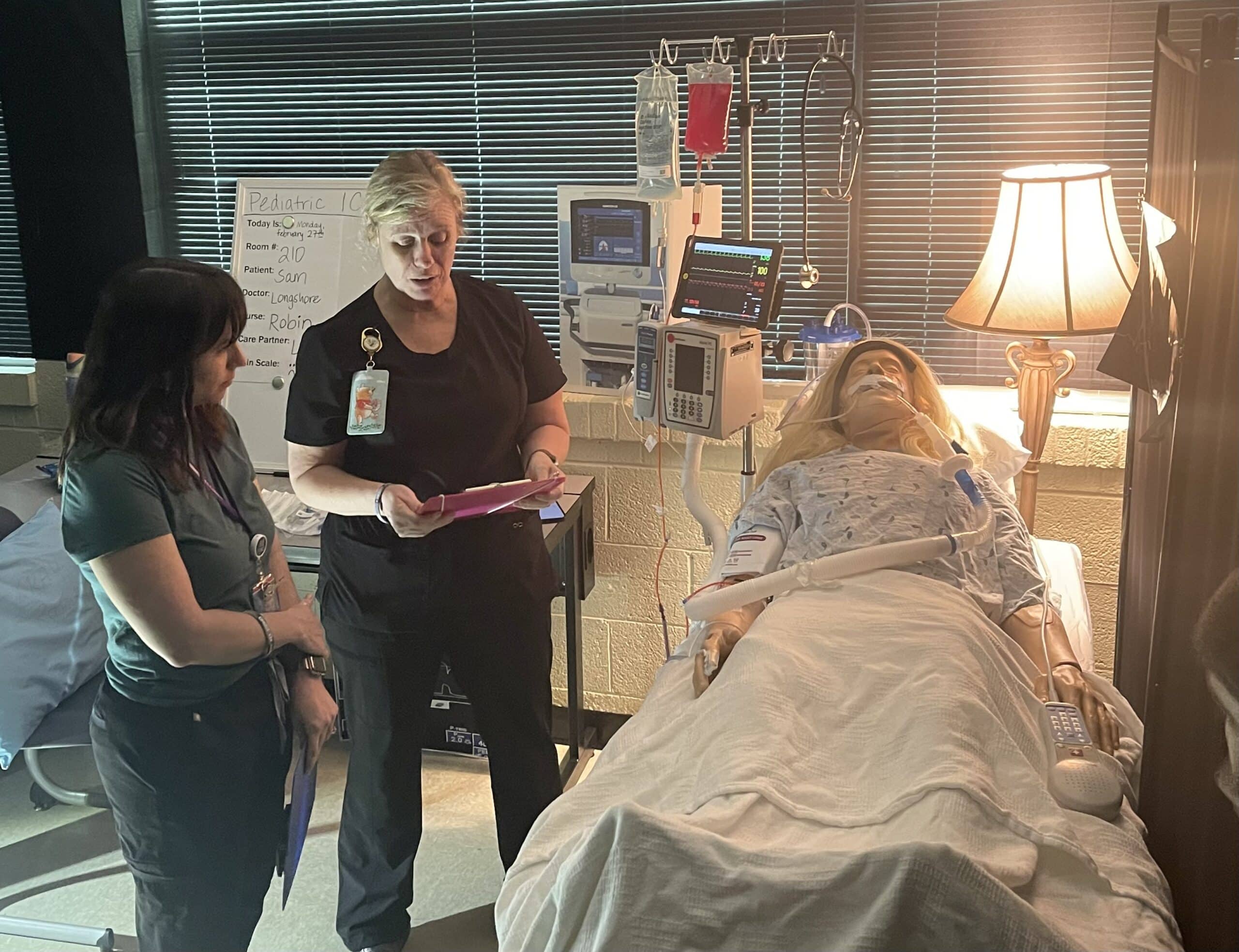
Emerson Fipps, a senior at South Central High School in Winterville, helped act out the first scenario with another student and an ECU Health volunteer. She said she’s proud to support events where she can help other young people set themselves up to make positive decisions.
“Middle school is really where everything starts to come up,” Fipps said. “Teenagers are just trying to find themselves so they’re getting into things that they shouldn’t. They’re not really fully educated about everything these destructive decisions could affect. It’s really good for them to start hearing about it young because when they’re in these situations, they’ll already have the information.”
Tiffany Thigpen, the Region 10 tobacco prevention and control coordinator for the Pitt County Health Department, said schools across the country are seeing an increase of students vaping and using gummies and other drug-infused edibles.
The National Poison Data System reported 3,054 cases of pediatric edible cannabis consumption in 2021, a large increase from 207 cases in 2017.
Thigpen said one of the most important things parents can do to keep their children safe from tobacco and drugs is talk to them.
“Talk to your children, let them know that these things are not safe,” Thigpen said. “Let them know that it is OK to say no. Talk to them about refusal skills and ways to say no to their peers. Let them know they can talk to you about what they’re experiencing. If they do use these products, share the dangers with them and ways to stop.”
Thigpen said the county is working to get as much information as they can into the hands of students about the dangers of drugs and vaping to help stop addictions before they begin.
Laurie Reed, manager of school health services at ECU Health, said partnerships make all the difference for events like the one hosted at A.G. Cox Middle School.
“Our school board and our school health advisory committee are very supportive of programs like this in our school system,” Reed said. “We just hope we’ll be able to offer more of them. It’s a great collaborative effort and it takes a lot of effort on the part of our school nurses, Injury Prevention, our health department, but it’s a great collaborative opportunity for our community.”
Children and adolescents with mental health care needs will benefit from a $3.2 million partnership between East Carolina University and the United Health Foundation.
The grant will expand the North Carolina Statewide Telepsychiatry Program (NC-STeP) within the ECU Center for Telepsychiatry and e-Behavioral Health. The investment is part of the United Health Foundation’s ongoing commitment to working with ECU to address mental health challenges in North Carolina — this time with youth.
In joining leaders to announce the three-year partnership, North Carolina Gov. Roy Cooper highlighted the critical needs surrounding children’s mental health in the state.

“Not only do we need to pay attention to our health, but our mental health as well and we’re recognizing that more than ever,” Cooper said. “That’s why I am so excited that the United Health Foundation, Dr. Sy Saeed and ECU have come together to try to get mental health treatment to young people in a more efficient and better way.”
Cooper said the NC-STeP partnership between ECU and the United Health Foundation helps advance toward his mission for the state for people to be able to live healthier lives with opportunities of purpose and abundance. Cooper said residents of rural North Carolina know how hard it is to get access to health care. Telemedicine will help bring experts to people wherever they are throughout North Carolina.
“I’m excited about this project. There are going to be people’s lives improved and people’s lives saved because of it,” Cooper said.
Through this expanded program, NC-STeP will provide access to mental health services for children in their established pediatric or primary care setting, removing the stigma sometimes associated with mental health care, said Saeed, director of the ECU Center for Telepsychiatry and founding executive director of NC-STeP. Through telemedicine, the program will offer expert consultation support for clinicians.
“In North Carolina, children experience significant challenges accessing the care needed to address their mental health. More than 70% of children in North Carolina with a mental health disorder do not receive treatment, and 92 out of 100 counties in the state are designated as mental health professional shortage areas,” Saeed said. “A growing body of literature suggests that the use of telepsychiatry to provide mental health care has the potential to mitigate the workforce shortage that directly affects access to care, especially in remote and underserved areas.”
NC-STeP was established in 2013 and has completed more than 56,000 psychiatry assessments in hospital emergency departments and has served more than 14,000 patients in its 23-community primary care settings. The expansion will provide mental health care services to underserved children and adolescents in six community-based pediatric and primary care clinics in rural and underserved parts of the state.
U.S. Reps. Greg Murphy and Don Davis, who helped guide NC-SteP in the General Assembly, have continued to support the initiative in Congress.
“It’s the people with boots on the ground, the people who are actually taking care of patients who deserve most of the praise,” Murphy said. “Sy has been a lifesaver for many individuals.”
Murphy thanked United Health Foundation for funding the initiative that will help address the unique challenges of patients in rural areas.

Davis emphasized the focus on children’s mental health as an important step in the effort to “provide every child a fighting chance to realize the American dream in eastern North Carolina. Dr. Sy has been a fearless voice in this effort,” Davis said.
“We’re honored and excited to partner with East Carolina University to address key health challenges our young people are facing,” said Anita Bachmann, CEO, UnitedHealthcare Community Plan of North Carolina, part of UnitedHealth Group. “By working together and creating an interconnected system of clinical and social services, we can continue to produce better health outcomes for North Carolinians.”
The United Health Foundation and ECU also partnered in 2020 through a $1.25 million grant to expand telepsychiatry services to address the mental health needs of expectant and new mothers. Through the Maternal Outreach Using Telehealth for Rural Sites (MOTHeRs) project, ECU developed and deployed a new obstetric care model for high-risk patients and addressed food insecurity among pregnant women.
North Carolina Health and Human Services Secretary Kody Kinsley touted the importance of access to health care — particularly mental health care services — in rural North Carolina.
“There is no health without mental health,” Kinsley said. “In particular, I think we know that mental health needs for children are more acute than ever.”
Kinsley said the investment announced today is a “win-win-win.” The project is being built on a program that has led statewide in expanded access to care.
“Truly it has been ECU driving access to telepsychiatry far before it was a fashionable thing,” Kinsley said.
Innovation is at the center of ECU’s initiatives fostering regional transformation in health care. ECU Chancellor Philip Rogers said the partnership with the university and the United Health Foundation allows many disciplines across campus to address the disparities in health care.
Rogers said the initiative would not be possible without the steadfast dedication and hard work of leaders at ECU, beginning with Saeed, who leads the team responsible for the operational aspects of the program.
“This transformative grant builds on our leadership in leveraging technology to provide care in the region and across the state,” Rogers said. “Our partnership with the United Health Foundation runs quite deep. This partnership has already made a significant impact as we prepare students to address the critical shortage of mental health professionals in our state.”
“Lucky” Xue, Robert D. Teer Distinguished Professor, Department of Management Information Systems, and students in the ECU College of Business are responsible for two components of the project — a virtual reality video game (AI) and a knowledge management system (KM). Xue said the project would have a profound impact on her research, teaching and community engagement.
“The objective of the AI-KM component is to strengthen the collaboration among mental health care professionals, family members and community partners across eastern North Carolina, and to optimize the utilization of existing mental health knowledge while uncovering innovative practices,” Xue said.
“The students from the Department of Management Information Systems in the College of Business will be given the unique opportunity to participate in the system development process. This will serve as a practical application of the knowledge they have gained through their coursework and an opportunity to make a positive impact on society. It’s an excellent chance for them to hone their skills and contribute to a meaningful cause.”
Regional disparities
In North Carolina, children experience significant challenges accessing the care needed to address their mental health. This partnership will help connect youth with mental health services in areas with provider shortages, said Dave Tayloe Jr. at Goldsboro Pediatrics.
“We have a significant shortage of mental health professionals, and often these key members of our health care workforce are not paid enough to cover their expenses when they provide mental health services for at-risk children. Most communities do not have even one child psychiatrist to help primary care providers care for the children who have the most serious mental health problems,” Tayloe said. “We have seen great benefit from providing mental health educational courses for primary care health professionals, having mental health professionals who work in the schools, the primary care practice, and the community, and having access to telepsychiatry services for the children most at risk for adverse mental health outcomes.”
The new grant program will take about six months to prepare. Saeed said that through NC-STeP, ECU is serving others as the university’s mission calls it to do.
“Mental health — including psychological, emotional and social well-being — is a vital part of our overall health. This is especially true for children when we consider that for many adults with mental disorders, symptoms were present, but often not recognized or addressed, in childhood or adolescence,” he said. “The good news is that we live in times when the care for mental disorders has never been more effective.”
Read more from ECU News Services.
Student perseverance and community and industry partnerships were highlighted in special presentations at the East Carolina University Board of Trustees’ February meeting.
The board also welcomed Brandon Frye, vice chancellor for student affairs, who officially joined ECU this week.
On Thursday, four students spoke during the University Affairs Committee meeting about their struggles and how ECU programs helped them continue to move forward. The students and the programs are: George Cherry Jr., Students’ Treasure Chest; Nellyana Cordero-Cisnero, Pirate Promise; Adam Harrison, Pirate Academic Success Center; and Iyaira Williams, Purple Pantry. Chris Stansbury, associate vice chancellor and senior operating officer for student affairs, moderated the panel.

In introducing the students, Provost Robin Coger said earning a degree requires students to persevere even when faced with challenges. ECU provides a range of support for student success. “Ultimately they come out of ECU ready for successful careers, but there are a lot of steps in between,” she said.
Cherry, who is earning three degrees and plans to attend medical school, put 24,000 miles on his car driving to class last year from his Bertie County home, where he helps take care of his younger sister. He was able to get help from the Students’ Treasure Chest when his car needed repairs. He is working to give back to the university through service and his involvement in different organizations, including the Student Government Association.
Cordero-Cisnero is a first-generation student from Raleigh who attended community college before transferring to ECU for a degree in elementary education. She said an ECU alum introduced her to Pirate Promise, which gave her a path to a four-year degree. “It opened a new door for me,” she said.
Harrison said he commuted from his home in Williamston his first year, and the connections he made at the Pirate Academic Success Center helped him become a stronger student. He now is a mentor to other students at the center.
Williams, from Raleigh, has volunteered at the Purple Pantry since her freshman year. As an ambassador, she helped the organization win a collegiate hunger challenge and $10,000, and she continues to work with the pantry to combat food insecurity. A recent partnership with the SGA has yielded almost 90 meals donated from unused meal swipes. The SGA also provided funding to purchase a freezer for the pantry to provide frozen meals.
The panel encouraged trustees to continue hearing from students and provide opportunities for conversation. They also suggested continuing to bring awareness to the resources that ECU offers.
In another committee Thursday, the trustee’s Committee on Strategy and Innovation heard an industry workforce panel discuss how partnerships can lead to innovation and economic prosperity in eastern North Carolina and beyond. Participants included representatives from ECU Health, Fly Exclusive and MrBeast. Topics ranged from the importance of building and strengthening partnerships and pathways to identifying ECU student and graduate talent to recruit to their businesses.
Panelist Julie Oehlert, chief experience and brand officer at ECU Health, said both the university and the health system can benefit from working more closely to integrate student experiences into education in a wide variety of disciplines in health care and beyond.
“We share a community, we share learners that we both love deeply, in a variety of settings,” she said. “We share the responsibility of caring for eastern North Carolina; for educating eastern North Carolina and for advancing all the people that live in eastern North Carolina in their learning and in their health. That’s why we are ECU Health now; never before has the imperative for a strong partnership been more relevant or more necessary.”
The panelists and committee discussed ways to encourage partnerships based on innovation and thinking outside the box that will push students to create real-world solutions in situations that prepare them to enter the workforce with concrete foundational experience.
The committee also adopted a resolution on freedom of expression for faculty and students, which was unanimously approved by the full board on Friday. The resolution reaffirms the Board of Trustees’ commitment to academic freedom and freedom of expression in which faculty and students can “teach, learn, seek and speak the truth” in an environment where “academic freedom flourishes” and the campus community is given “the broadest possible latitude to speak, write, listen, challenge and learn except insofar as limitations to that freedom are necessary to the function of the university.”
Trustees also received an update on refreshing the university’s strategic plan. Committee co-chair Sharon Paynter presented a list of internal and external strengths, weaknesses, threats and opportunities that impact university initiatives and ways ECU leadership, faculty, staff and students continue to navigate them.
Read more from ECU News Services
East Carolina University’s postgraduate program in cardiac psychology creates professionals who are ready to help patients cope as they adapt to life-saving heart devices.
On the heels of marking its 15th year, ECU’s nationally unique program in clinical health psychology continues to gain momentum through positive patient outcomes — and national recognition.
The program is a collaboration between ECU’s departments of psychology and cardiovascular sciences that has yielded a nationally unique blend of academics and research. The model integrates training psychology doctoral students and cardiology fellows in cardiac clinics, a strategy that the program’s founder calls the best of both worlds.

“This is a success story from eastern North Carolina,” said Samuel Sears, program director and professor in the departments of psychology and cardiovascular sciences. “From a national landscape, this is an extremely unique program. Only at East Carolina do you have this kind of synergized, integrated, one-for-one engagement in the training of cardiologists and the training of psychologists. Our program is intending to lead the country in this.”
Sears established the training program in 2007 and collaborates with Rajasekhar Nekkanti, associate professor and director of the cardiology fellowship program at ECU and ECU Health, to offer ECU students an integrated program experience that spans clinical care, research and training.
“Dr. Sears and his colleagues have been able to accomplish what others have only talked about,” said Alan Christensen, professor and chair of the ECU Department of Psychology. “Their seamless integration of clinical psychology into a cardiovascular medicine setting is really a pioneering effort in implementing what I believe will prove to be a more effective approach to training, research, and caring for patients.”
The growing field of cardiac psychology focuses on providing psychological care that is an interdisciplinary, comprehensive care approach to cardiac arrhythmia patients and their families.
Depression and anxiety are common occurrences after cardiac events and can occur in as many as one-third of all patients. These conditions interfere with all aspects of recovery from daily rehabilitative planning, medication adherence, and the pursuit of quality of life.
“Cardiac psychologists help by validating the emotional experience of having a heart problem, and helping patients take the next steps in their recovery emotionally and behaviorally,” Sears said. “ECU Cardiology and Cardiovascular Surgery continue to innovate, and that allows our patients to survive. Here at East Carolina, we have the vision and program to address the patient experience and recovery process fully from a psychological and behavioral perspective. We integrate all the aspects of recovery and prepare trainees for the future of cardiac care.”
The program was highlighted in a 2022 edition of Health Psychology, a journal of the American Psychological Association. The article, “Cardiac Psychology Training in a Rural Health Care Setting: East Carolina Heart Institute,” was led by author Kayla Sall, a 2023 graduate of ECU’s clinical health psychology program. Doctoral students Ashley Griffith, Emily Midgette, Andrea Winters and Connor Tripp also co-authored the article with Sears and Nekkanti.
“We are very proud to publish in our field’s top journal,” said Sall, who begins a psychology internship at Brown University this fall. “The publication goes to show how unique our training experience is. It’s very rare to find cardiac psychologists that are located in cardiology.”
The Health Psychology article covers not only the program’s unique nature of intertwining science with practice, but also its ability to adapt to the COVID-19 pandemic by transitioning to using telehealth to serve patients in rural North Carolina. It also explores the health disparities in eastern North Carolina that impact cardiac patient care and progress.
“Cardiovascular health is one of the leading causes of death in the U.S.,” Sall said, “so being able to take that lens and apply it to the social determinants of health has been amazing, and it’s how we’ve been able to do what we do.”
Greenville native and ECU graduate Scarlett Anthony didn’t have to go far to find a program that offers world-class education and preparation that will help her make a difference in her home region and beyond.
“I chose ECU’s program because of the focus on health psychology and the intersection between psychology and medicine. We train alongside psychologists who are embedded in medicine, and our program provides us with exceptional training among various health care settings,” said Anthony, a doctoral student in clinical health psychology. “I chose ECU’s program because of the dedication to serving diverse populations of eastern North Carolina, and I am passionate about providing care to those who may not have access to health psychology services otherwise.”
Standards of practice

Sall led the writing team in detailing the ECU training program and its strong collaborations in cardiology. The article presents ECU’s program as a national model for ideal collaboration between cardiology and psychology training that enhances the clinical and research expertise of both groups.
The ECU cardiac psychology program is part of the APA accredited clinical health psychology program. This program has achieved national rankings over its 15-year existence and annually has an approximately 5% acceptance. Rob Carels serves as the director of clinical training for the clinical health program.
“The article confirmed that the ECU program is not only one of a kind, but it remains the model as programs and universities try to create this similar-type experience,” Sears said. “The reason it’s so hard to create the ECU experience is that it requires both physicians and psychologists accommodating very different mindsets and contributions with the shared goal of patient success first. Physicians can quickly implant a cardiac device. Psychologists can quickly assess and treat psychological concerns. But when these two sets of problems merge, we need shared expertise.”
The article also highlights the setting of ECU’s health psychology program, a rural area where the social determinants of health — including environment, economic stability, community context, education and health access — impact health and wellness on a greater scale.
“Being in eastern North Carolina, we have a very unique setting with our patient population in a rural area,” Sall said.
That context allows psychologists to better understand the behavioral and mental health of cardiac patients. Many patients seen by cardiac psychologists at the East Carolina Heart Institute include those who suffer depression after a heart attack or other cardiac event, those with atrial fibrillation (a-fib) and those who have recently been fitted with implantable cardioverter defibrillators (ICD) — devices similar to pacemakers that correct heart arrhythmias with a high energy shock that can feel like being kicked by a horse.
“I think that is what is so scary for patients; they agree to have this device implanted, they know it’s life-saving, but you don’t know when the shock is going to go off,” Sall said. “You may go the whole rest of your life without receiving a shock, so that’s where part of the anxiety and fearfulness comes in.”
In the program’s scientist-practitioner approach, providers on each side have a thorough understanding of the opposite discipline.
“I think that’s what’s cool about cardiac psychology — here we are with people presenting with medical conditions or health issues and we’re evaluating, diagnosing, treating emotional behavioral disorders within the context of health and medicine,” Sall said. “We’re not doing just one or the other, we’re doing these together.”
World expert in action
Sears is a highly productive researcher examining quality of life and psychological adjustment in patients with heart rhythm disorders and ICDs. He has published more than 200 articles in the medicine and psychology research literatures and has well over 11,000 citations. In 2021, Expertscape.com named Sears one of the top 50 experts and most prolific authors in the world on ICDs over the last 10 years, amongst the 27,847 authors on the topic.
“I’m involved in both the training of psychologists as well as the training of cardiologists, so we’re trying to make cardiologists better at patient psychology and psychologists better at understanding the cardiology, so it’s synergistic,” Sears said.
Sears travels the world presenting his research and lending his expertise to patient, family and physician groups.
In 2013, the UNC Board of Governors presented Sears with the O. Max Gardner Award, the highest honor bestowed to a faculty member in the UNC system for contributions to mankind.
“The O. Max Gardner Award changed me because I stopped looking for external validation about our achievements. I desperately wanted to make an impact on our patients, our students, our university, our state and beyond,” he said. “The award confirmed some of these marks, so I used my energies more efficiently on the work at hand. I am proud of the health psychology program and the cardiac psychology program that my colleagues and students have created. In terms of work, I am so pleased that many of our ideas about helping cardiac patients are broadly employed across many sectors in cardiology, not just where we started.”
The article in Health Psychology signals consistent success and upward momentum for the program, said Sears, adding that Yale University’s health psychology program is the only other such program mentioned in that edition of the journal.
“This is a 15-year-old program. We’ve established success,” he said. “This is not a great idea that’s going away. Great ideas happen all the time, but they’re not sustainable. This is a sustainable solution that has true outcomes.”
When it comes to patient outcomes, Sears is optimistic that the growing field of cardiac psychology will continue to yield hope and healing.
“We can’t fix all the health inequalities, but what we can do is help our patients make small steps to have better awareness of where there are a lot of possibilities and decision points, and connect them to other resources,” Sears said. “Yes, this is a hard mountain to climb. Let’s do this together.”
Doctoral student Zachary Force said students begin the program learning what clinical health psychology can offer the world — and how ECU is leading the way.
“ECU has always done things differently, and other institutions are starting to take notice. ECU’s cardiac psychology service has received national recognition as the only place in the country to receive specialized training in an area with increasing need,” he said. “ECU’s fighting spirit imbues its doctoral students with the resiliency needed to advocate for psychology within the medical field.”
Read more from ECU News Services
Halifax, N.C. – ECU Health proudly joined community officials and business and health leaders at a Medicaid expansion roundtable hosted by U.S. Congressman Don Davis at the Halifax County Health Department Friday, Jan. 20, 2023, followed by a tour of ECU Health North Hospital.
Jay Briley, president of ECU Health community hospitals, and Jason Harrell, president of ECU Health North Hospital, attended the roundtable to offer insights on health issues impacting Halifax County and eastern North Carolina. Officials urged the need for Medicaid expansion, and community leaders offered perspective and insight on how to best advocate for expansion in North Carolina, which would provide invaluable health and economic benefits to communities across the region. With Medicaid expansion, more than 600,000 North Carolinians – 100,000 of whom live in eastern North Carolina – would have access to the affordable health care coverage they need.

“ECU Health is grateful for the opportunity to meet with Congressman Davis and other community leaders to discuss Medicaid expansion and other important health care needs for Halifax County and the region we so proudly serve,” said Briley. “Medicaid expansion is a crucial initiative that would provide numerous benefits for the state, and especially here in rural eastern North Carolina, where we see high rates of chronic diseases and high rates of uninsured patients. Simply put, Medicaid expansion would make an important difference in the lives of so many, and we are committed to advocating for this important measure.”
Following the roundtable, Briley and Harrell welcomed Congressman Davis to ECU Health North Hospital for a tour of the hospital, including the oncology unit and women and children’s unit. During the tour, the leaders discussed how Medicaid expansion and the Healthcare Access and Stabilization Program would help provide much-needed relief for rural hospitals across the state, ensuring that rural North Carolinians have access to high-quality health care.
“Rural hospitals like ECU Health North play a critical role in the communities they serve,” said Harrell. “Our hospital is not only a hub for high-quality care, but it is also the largest employer in the county. Medicaid expansion should be a top priority for the state, and we appreciate Congressman Davis’s efforts to advocate for the health and well-being of eastern North Carolina.”
Resources
“It was very nerve wracking coming here,” said Denique Barnett, a pediatric rehab nurse at the James and Connie Maynard Children’s Hospital and international nurse at ECU Health. “I’m an only child, so leaving my family in Jamaica was very hard.”
For Barnett, pursuing her passion has been a journey of more than a 1,000 miles.
“The welcome that I received was a good one,” Barnett said.
The warm reception Denique received is one ECU Health offers nurses from around the world as part of the International Nurses Program.
“My passion is pediatrics, but specifically neonatal nursing,” Barnett said. “Back home there is no degree program for neonatology. So I decided that, you know, to further my studies and to self-actualize, I would need to come to the United States.”
Not only does the program foster additional growth and training for participants, it also fills an important recruiting need for the health system.
“We bring international nurses from all over the globe to come to our organization to spend about two years in a clinical environment,” said Charlene Wilson, chief people officer of ECU Health.
Launched in November 2019, 175 nurses from 21 countries have since spent time at ECU Health.
“Even though these are nurses that are seasoned nurses, they have to go through our NCLEX,” Wilson said. “They then go through the immigration process. They then begin to understand the culture of the various hospitals that have openings for international nurses. One of the things that is very different about their practice here versus their practice in their home countries is the technology.”
“At first, you know, getting used to just how things are done here using technology for me, that was a bit of a challenge,” Barnett said.
“I’m always told by the clinicians, including the doctors, that one of the things that is fascinating about what they bring is their analytical skills, because they don’t have the technology that we have here in the United States,” Wilson said.
It’s a unique perspective put to work for a common goal, improving the health and well-being of the region these nurses now call home.
“As an international nurse, making the leap is the best decision that you will make. There is a lot of opportunities for growth,” Barnett said. “There are a lot of benefits to being here at ECU Health, you know, just make the leap, come, you won’t be disappointed.”
Greenville, N.C. – ECU Health, the premier health system serving eastern North Carolina, experienced a transformational year highlighted by the introduction of a new brand, announcement of a new behavioral health hospital, recognition of multiple team members on the state and national levels and realization of clinical achievements and innovations that enhance the care for the 1.4 million people the organization proudly serves.
“As we reflect on the historic year that was and celebrate our achievements, I want to take a moment to extend my heartfelt gratitude to the team members who make ECU Health what it is: a premier rural academic health system dedicated to serving the people who call eastern North Carolina home,” said Dr. Michael Waldrum, ECU Health CEO and Dean of the Brody School of Medicine. “As one year comes to a close and another begins, I know the next chapter of our shared story will be just as important. Our efforts in 2022 helped position us to navigate the complex challenges we face moving forward by bringing clinical, education and research innovations, but we still have work to do in the upcoming year and beyond to ensure our communities have access to the high-quality care they deserve.”

The following highlights are only a few of the many achievements across ECU Health in 2022. For a more comprehensive review of the year, please visit: ECUHealth.org/YearinReview2022
Evolving to ECU Health
The re-brand to ECU Health is a visual reminder of how transformative the year has been. The ECU Health logo is a symbol of the commitment to transforming and elevating health care for millions, training the providers of tomorrow, collaborating with community partners to solve complex issues and bringing clinical innovations that improve the lives of those who call this region home.
The Brody School of Medicine at East Carolina University and the health system began a joint operating agreement on Jan. 1, 2022. In April, the two organizations hosted a press conference and shared the new logo for ECU Health and announced the brand launch that would begin in May.
In the months since, there have been visual changes across the health system from signage around hospitals and clinics to websites and social media channels. More importantly, the creation of ECU Health has opened the door for the system to improve access to care across eastern North Carolina while training health care professionals through Brody.
Expanding access to behavioral health care in eastern North Carolina
Access to behavioral health care is crucial across the country, but especially in rural areas like eastern North Carolina. In June, ECU Health and Acadia Healthcare announced plans to build a state-of-the-art, 144-bed behavioral health hospital in the medical district of Greenville, less than a mile from ECU Health Medical Center.
Slated to open in spring 2025, the hospital will operate through a joint venture between ECU Health and Acadia, the largest standalone provider of behavioral health care services across the United States. Together, the organizations will invest approximately $65 million in expanding behavioral health resources in eastern North Carolina.
The hospital will include 24 inpatient beds specifically for children and adolescents with mental health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
Twenty-two ECU Health nurses recognized among Great 100 Nurses of North Carolina
This year, 22 ECU Health nurses were selected to the 2022 NC Great 100. This is the largest number of ECU Health nurses to receive this recognition. The honorees were celebrated at a gala hosted by The North Carolina Great 100, Inc. in Greenville in October.
Since 1989, The North Carolina Great 100, Inc. has recognized and honored nurses around the state for their commitment to excellence and to promote a positive image of the nursing profession. Out of thousands of nominations that are submitted annually, 100 recipients are selected based on their outstanding professional abilities and contributions made to improving health care services to their communities.
ECU Health Beaufort Hospital designated as primary stroke center by The Joint Commission
In July, ECU Health Beaufort Hospital – a campus of ECU Health Medical Center was designated as a primary stroke center by The Joint Commission and the American Heart/Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients. Stroke is one of the leading causes of death in the state, resulting in more serious long-term disabilities than any other disease.
With ECU Health Beaufort’s designation, all ECU Health’s hospitals are stroke certified by The Joint Commission.
The holiday season brings so much joy, especially for young children and their families that get to see them light up as they unwrap presents.
While picking out toys that young ones will love, it is also important to consider the safety of the toy, Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center, said.
In 2021, there were more than 152,000 toy-related, emergency department-treated injuries to children under the age of 15, according to the Consumer Product Safety Commission.
“I think the thing is, because of COVID and supply chain issues, a lot of parents have a lot of pressure on that perfect gift,” Walston said. “But you don’t need to sacrifice safety.”

Walston noted toys with many pieces and stuffed animals with poorly sewn features as choking hazards for small children. A good test, she said, would be to use a toilet tissue roll to see what kinds of items might be a choking hazard for a child. If it could get stuck in a toilet tissue roll, it could be ingested and become a choking hazard.
She said often older children and younger children in the same home can play with different toys that may be safer for the older child than the younger child. It is important to remind older children to put away toys when they are done using them to make sure younger children cannot get hurt using that toy or ingesting pieces.
A key concern each year, though, is button batteries, Walston said. Button batteries can be found in many objects around a home, including car key fobs, thermometers, scales and some remotes. These can also be found in books that play music and many singing cards. Walston said if a child gets to these batteries, it can be very dangerous — not only as a choking hazard, but also the possibility for chemical burns from the battery.
Last, Walston reminded anyone purchasing a bike for a child to not forget a helmet and bell or another item that makes noise.
Walston said it all comes down to making educated choices and supervising young children while they play to keep them safe and avoiding an emergency.
“Please make sure that you’re paying attention to labels,” Walston said. “If a toy says ‘not recommended for a child under three years of age,’ you have to take those warnings seriously. Also, supervision is critical and just making sure that children are safe when they’re playing.”
Keeping children safe with their toys helps ensure a happy holiday season for all.
Resources
ECU Health Beaufort Hospital, a campus of ECU Health Medical Center, hosted free community health screenings, produce giveaways and educational information at its first fall harvest event at the new community garden and outdoor classroom on Nov. 18.
The community garden and outdoor classroom, located next to the ECU Health Wellness Center in Washington was made possible — in part — by a grant from the Robert Wood Johnson Foundation and the garden was developed by the ECU Health Patient Education team in collaboration with ECU Health Beaufort Hospital. Internal partners include the ECU Health Beaufort Hospital Food & Nutrition Services team, Community Health Improvement team, Volunteer Services, the Wellness Center, and Facilities & Properties.
“It has been wonderful working with such an innovative team,” said Tammy Thompson, director of Experience Engagement, Education and Design at ECU Health. “They have been true partners throughout entire process.”

Sowing the seeds for health and well-being
Over the summer, the garden started to take shape, resulting in 10 raised beds for vegetables, two large metal planters for herbs, fencing, a shed and space for community members to come together and learn outdoors. The hospital planted the first crops in September for the first harvest event.
Pam Shadle, director of Marketing, Community Outreach and Development at ECU Health Beaufort Hospital, said the opportunity to come together as a team and create something that will benefit the community has been a great experience.
“It’s been a labor of love since the creation of the idea,” Shadle said. “So many of our team members from various departments came together to make this happen, so it’s been a great opportunity for our folks to get involved and I really appreciate that.”
Shadle said the community garden and outdoor classroom is an integral addition to their community health improvement plan for Beaufort and Hyde county residents. While they already feel the great impact of existing programs on community health, the garden will help create new opportunities and help improve those established programs, Shadle said.
Beyond the harvest
The ECU Health Food and Nutrition Services team joined the event and shared easy-to-make recipes inspired by the garden’s produce — which includes vegetables and herbs like broccoli, collards, kale, lettuce, rosemary and thyme. Along with the opportunity to take home fresh, free produce, clinical teams were on hand to offer health screenings for community members, and the Wellness Center team shared information about lifestyle medicine and other services to support community wellness.
“It’s just a great complement to include these offerings because what we’re trying to do is not solely about food,” Dr. Thompson said. “We call these living-learning labs because of the interactive engagement to support healthy lifestyles. This is an opportunity for community members to receive a variety of information and resources for better health.”
ECU Health Chief Experience Officer Julie Oehlert, DNP, RN, said the garden is an important step in the community health work in eastern North Carolina.

“We’re so proud of the teams that made this garden a reality,” Dr. Oehlert said. “It’s going to benefit community members, team members and patients in the hospital and I think it’s really special for us to connect with the communities we serve in this way. We’re excited to offer something unique for Washington and Beaufort County and I know we’re going to learn so much from this project.”
Planning your visit
The garden will be open to community members from 9 a.m. to noon each Wednesday and Friday where any produce ready to be harvested will be distributed and other educational materials will be shared.
