For the Eastern Carolina Healthcare Preparedness Coalition (EHCPC), being ready is part of the job.
“What we have here is our field communications support truck,” said Matt McMahon, disaster services specialist with EHCPC. “This is essentially the heartbeat of our mobile field hospital.”
From trucks that double as mobile hospitals to coordinating evacuations or the deployment of medical supplies, the coalition remains on standby for when emergencies strike or networks go down.
“So, if a hospital loses communication, whether it be phone, radio or internet, we can come and support them,” McMahon said.
The coalition provides a critical line of support, whenever and wherever it’s needed most. As they prepare for hurricane season, they want you to do the same.
“We want people to be prepared, and starting a hurricane kit is the first step in doing so,” said Chris Starbuck, health care preparedness coordinator for EHCPC.
A basic kit includes important items, like water, food and other supplies to last several days. Ready.gov is a federal government website with helpful information about how to properly prepare for a hurricane. Creating a plan that meets the specific needs of your household and building an emergency kit that contains at least 72 hours’ worth of supplies can help you stay adequately prepared for a natural disaster like a hurricane.
“Put all your important documents together – marriage certificates, birth certificates, wills,” Starbuck said.
Another item for your hurricane prep checklist – help others plan, too.
“Work with your neighbors, your communities, churches, because if we can prepare them, we can make a more resilient community overall,” Starbuck said.
Resources
Hurricanes can form quickly. Take the time now, before a hurricane impacts our region, to educate yourself on how to prepare and respond. Below are helpful links for federal and state websites:
- Ready.gov – Hurricane Information
- Ready.gov – Make a Plan
- Ready.gov – Build a Kit
- ReadyNC.org
- ReadyNC.org – Emergency Alerts
- ReadyNC.org – Evacuation Routes
- ReadyNC.org – Know Your Zone
Watch more ECU Health News videos
While skin cancer is less common in African Americans, experts say death rates from melanoma are much higher in the African American community. Melanoma, which often presents as an irregular mole, can spread much quicker and easier than most other skin cancers and can produce worse outcomes. Melanoma is often found in later stages in African Americans when treatment can require more intensive surgery or even radiation or chemotherapy. Knowing the signs and symptoms can help catch melanoma early, when the cancer can be cured.
African Americans are up to four times more likely to be diagnosed with advanced melanoma and 1.5 times more likely to die from melanoma, according to the Melanoma Research Alliance. This is alarming, considering African Americans account for a small portion of melanoma diagnoses.
Skin cancer is the most common type of cancer. The three major types of skin cancer are basal cell carcinoma, squamous cell carcinoma and melanoma. Basal cell carcinoma and squamous cell carcinoma can present as pink or scaly lesions that are not healing or spots that are bleeding, itchy or painful. These forms of cancer are largely treatable and less severe than melanoma, which presents as an irregular mole.
UV rays from the sun and tanning beds are responsible for most cases of skin cancer. While sun exposure from UV rays may contribute to some degree of skin cancer in African Americans, the genetic makeup plays the largest part in melanoma diagnoses.
“Melanoma shows up in areas that typically are not exposed to the sun, like the toes, tips of the finger or under fingernails and toenails,” said Dr. Tiffany Alexander, dermatologist, ECU Health. “When identified and treated early, most melanoma cases are curable.”
However, melanoma can spread quickly into the blood and to other organs if not found early, and can even be deadly. Knowing that African Americans are more likely to be impacted by advanced melanoma, Dr. Alexander recommends learning the signs and symptoms and taking early action to detect and treat melanoma in its earliest stages.
“African Americans typically present in a more advanced stage because there is not a lot of awareness of melanoma occurring in African Americans, and the perceived risk of melanoma among African Americans is typically low,” said Dr. Alexander. “Many people also neglect to check areas that are not typically exposed to the sun frequently.”
Completing regular self-exams of areas both exposed to the sun and areas not exposed, like fingers and toes can help catch irregularities early. The ABCDEs of melanoma can help in identifying odd or suspicious moles that may need a second look by a dermatologist.
- A: Asymmetric, irregular shape
- B: Borders that are irregular and not round
- C: Color – a mole that is differently colored than other moles
- D: Diameter more than 6 mm in size
- E: Evolving, growing rapidly, a mole that becomes symptomatic
One of the most common misconceptions is that people with darker skin do not get sunburned, according to Dr. Alexander.
“A common myth I hear from my patients is that people with darker skin do not get sunburned,” said Dr. Alexander. “While those with more melanin in their skin have more protection against the sun, I encourage everyone to wear sunscreen with a minimum 30 SPF, no matter skin color.”
Most importantly, Dr. Alexander says, pay attention to your body.
“Get out of the sun if you feel yourself burning,” said Dr. Alexander. “If there is a mole that fits in the ABCDEs of melanoma or a lesion that is not healing or spots that are bleeding, itchy or painful, see a dermatologist.”
Dermatologists provide professional and thorough skin checks and can identify potentially cancerous areas early, when treatment options are great and the cancer is curable. To find a dermatologist near you, please visit ECUHealth.org/dermatology.
ECU Health is proud to announce that the North Carolina Healthcare Association (NCHA) awarded Melanie Porter, administrator of hospital operations, and DeAnna Edwards, manager of hospital operations, the Healthier Communities award for their work in the Statewide Patient Movement Coordination Team. This award recognizes collaborative work by NCHA member organizations to promote health and well-being by addressing an identified community need.
COVID-19 has put a strain on health care systems across the globe and here in North Carolina. Throughout the pandemic, hospitals and health systems have worked tirelessly to advance new approaches to promoting more equitable health outcomes for patients, families and communities. Among these innovations, the Statewide Patient Movement Coordination Team emerged.

The Statewide Patient Movement Coordination Team is a group of individuals at transfer centers across North Carolina who have worked tirelessly during the pandemic to ensure critical patients needing higher levels of care were transferred or those facilities given additional clinical support.
As part of this team, Melanie and DeAnna are both dedicated to living the ECU Health mission of improving the health and well-being of eastern North Carolina. Through their work, they ensure patients have quality care and are connected to the level of care and resources needed.
The Statewide Patient Movement Coordination Team assisted 35 facilities not formally connected with the 13 transfer centers across the state who had critical patients needing higher levels of care.
In total, this team reviewed 765 patient movement requests during the Delta and Omicron surges of COVID-19.
Please join us in recognizing Melanie and DeAnna for representing ECU Health and making a difference in the lives of those we serve.
Leaving a child, senior or pet behind in a car can pose serious danger, even if it’s just for a few minutes.
That was the message of the hot car safety event hosted by Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center, along with the Pitt County Health Department and the Martin-Pitt Partnership for Children.
Walston said it’s dangerous for anyone to be left alone in a vehicle because of how quickly they can heat up, but especially for children.

“Children’s bodies heat three to five times more quickly than adults,” Walston said. “They all have a smaller amount of body surface so they can’t cool themselves very quickly. A small child, like the families we’re serving today, they can’t verbalize when they’re thirsty if they’re under a certain age. You really have to be very careful. The message is never leave a child alone in a car, not even for a minute.”
The team had a demonstration with temperature gauges and s’mores roasting in a vehicle on an 80-degree day, one of the coolest days in recent weeks in eastern North Carolina. Despite the cooler than normal temperatures, the interior of the van rose to 90 degrees within 15 minutes, over 100 degrees after an hour, and approached 120 degrees in an hour and a half.
The s’mores demonstration showed how quickly things can literally cook inside of a car when left alone.
“As you see we have this temperature gauge here and just in the last 15 minutes, it’s already gone up 10 degrees,” Walston said. “This is a white car with light interior, and with a dark car and dark interior it can heat the car more quickly.”
Walston noted that there have already been 10 deaths across the country this year from children left alone in cars. In North Carolina, we have seen one this year and another in neighboring Virginia.
She said more than 50 percent of child deaths from hot cars are from children that have been forgotten in vehicles. She said children can be forgotten when routines are broken and leaving something like keys, your cellphone or a briefcase in the backseat next to the child is a safe way to ensure the child is not left alone.
According to Walston, about 17 percent of hot car fatalities are children that are intentionally left behind. She said no amount of time is safe for a child to be left alone, even with windows cracked.
“Many times folks think that, I’m just going into the store for a few minutes, but anything could happen inside, you could become distracted and forget the child,” Walston said. “There is a misnomer that if you crack a window and that will offer some less heat, but that really is a myth. It doesn’t affect the temperature of the car.”
As a rural health care organization, we know there are many challenges to fostering a healthy community. That doesn’t stop ECU Health team members from finding creative solutions to bring health care outside the walls of our hospitals and clinics in eastern North Carolina and into the communities we serve.
KaSheta Jackson, DNP, RN, vice president of Health Equity and Social Impact at ECU Health, and her team developed Community Pop-Ups: A Rural Approach, an innovative health care delivery model implemented as community-based pop-up clinics across eastern North Carolina to address social and economic health care barriers.
This program makes health care both more accessible and approachable by directly providing preventative services, improving health care equity, and offering resources within communities with the greatest need.
Jackson was recognized earlier this year by the American Nurses Association (ANA) and the American Nurses Foundation (the Foundation) as the recipient of the 2022 ANA Innovation Award. The ANA Innovation Awards highlight, recognize and celebrate exemplary nurse-led innovations that improve patient safety and health outcomes. The innovation award also generated a $25,000 grant, which will fund future community health events.
Jackson said nurses are on the leading edge of connecting their fellow community members to health care and should feel empowered to innovate in that space.
“Our innovation has empowered many nurses to think and behave differently with regards to changing health care delivery and where care is delivered,” Jackson said. “By aligning the community and the health care system, we are addressing social, economic, equity, and population health, allowing us to meet our mission of improving the health and well-being of eastern North Carolina.”
Through partnerships with community leaders and other ECU Health team members, these clinics have evolved from solely offering health care screenings to providing COVID-19 testing, vaccinations, mental health resources, access to fresh produce and employment opportunities.
In 2021 alone, Community Pop-Ups provided care to more than 400 community members, identified acute diseases, provided numerous jobs, gave away 500 produce boxes, and delivered 500 health passports in rural locations across eastern North Carolina.
“We are following the model of doing health care on the outside to make health care better on the inside,” Jackson said during a July 2021 community health event in Farmville. “We’re working to address the social determinants of health, offering employment, trying to take care of the need for vaccines, taking health care into communities versus having people come to us – we’re taking services to those that need them.”
As these pop-up events evolve and grow, Jackson hopes they will help create a healthier eastern North Carolina, strengthen ties between community organizations and improve relationships between community members and health care providers.
“I am so excited to see our innovation become reality,” Jackson said. “The advice I would give to any nurse who wants to take their innovations from just an idea to action: be inquisitive, be nosey, ask questions, listen and it will be easy to make it happen.”
This is just one example of how Jackson and her team break down barriers to bring health care to the communities we serve. ECU Health also hosts a myriad of community events including: a foot clinic with Joy Soup Kitchen and Access East, which gives free foot care supplies to diabetic patients who visit the event, over-the-counter medication giveaways and Kids Eat Free with Sodexo, which provides free lunches and afternoon snacks for kids and teens up to age 18.
For more information, visit the Pop-Up Community Health Events page on our website.
Health care workers are well-versed in serving their community, even if that community happens to be an ocean away.
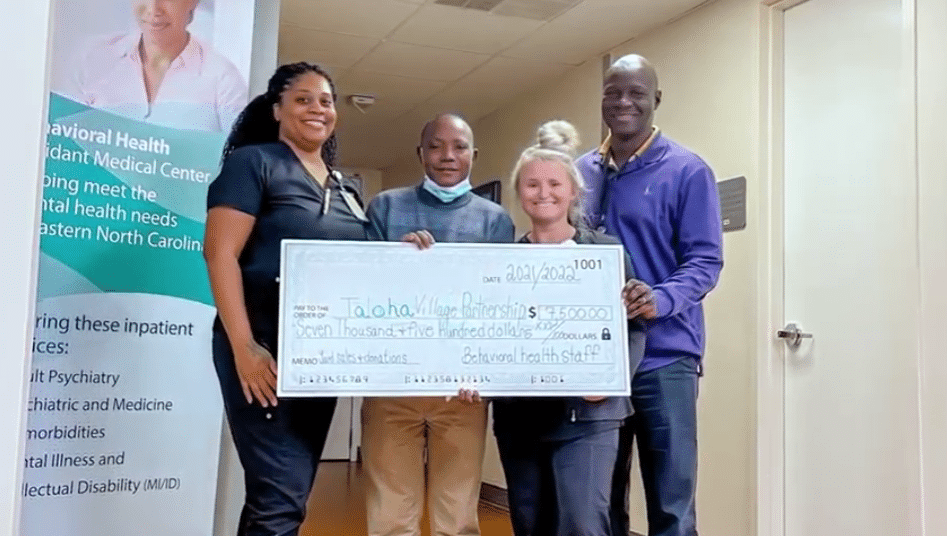
“I’m from Tanzania, east Africa. In a rural village called Taloha,” said Daniel Makoko, behavioral health team member at ECU Health.
After settling in eastern North Carolina, Makoko continued to help improve living conditions in his home village.
“The village has one primary school,” Makoko said. “So these kids use like four classrooms but there are like 270 kids. They share the classroom because it’s not enough. But also the main problem was that the room was leaking when it’s raining.”
So Makoko set about raising money through donations and events like yard sales to put a new roof on the primary school.
“They asked me, ‘What can we do?’ So I told them that if we can get a roof for them, It will be much transformation for the school,” said Makoko.
A transformation in more ways than one, made possible with the help of friends, family and colleagues.
“He’s a great inspiration to me just to see all the things that he has accomplished”, said Tony Dixon, a behavioral health team member at ECU Health. “Between four yard sales and donations from behavioral health services, we were able to raise the four-thousand dollars to get the roof done.”
“I was able to go there and implement the project and we finished the roof and the kids were so happy,” said Makoko.
It’s joy no roof can contain and an example of ECU Health values making a difference half a world away.
“This shows the greatness of the people here and how they are able to respond to the needs of other people across the world,” said Makoko. “I really appreciate it so much.”
Resources
Watch more ECU Health News videos
ECU Health CEO and Brody School of Medicine Dean Dr. Mike Waldrum named to AAMC’s Board of Directors
Dr. Michael Waldrum, dean of East Carolina University’s Brody School of Medicine and chief executive officer of ECU Health, has been named to the board of directors of the Association of American Medical Colleges (AAMC). He joins 18 other medical school and health care leaders from across the nation and Canada named to the board, including representatives from Yale School of Medicine, Georgetown’s School of Medicine and Harvard Medical School.
“It is an honor to be named to the AAMC Board and to work with my colleagues in academic organizations across the national landscape to chart a healthier future for our communities and region,” Waldrum said. “Academic health care drives innovation, produces clinical excellence, and creates a teaching environment that helps train the providers of tomorrow. I look forward to continuing to collaborate alongside national leaders and focusing on how we can best support our students, faculty and academic rural health care.”

The AAMC leads and serves America’s medical schools and teaching hospitals and individuals employed across academic medicine, including more than 191,000 full-time faculty members, 95,000 medical students, 149,000 resident physicians, and 60,000 graduate students and postdoctoral researchers in the biomedical sciences. This year, the Association of Academic Health Centers and the Association of Academic Health Centers International merged into the AAMC, broadening the AAMC’s U.S. membership and expanding its reach to international academic health centers.
Dr. Waldrum, who was first appointed to the AAMC Board of Directors in November 2020, will begin his new term Nov. 15 and will also serve as chair of the AAMC’s Council of Teaching Hospitals and Health Systems.
“This is such an important time in our industry and as chair of COTH, I look forward to bringing premier academic health systems together to define solutions that strengthen our health care workforce, support our students, advance research and address disparities, specifically in rural communities,” Waldrum said.
The AAMC is a nonprofit association dedicated to improving the health of people everywhere through medical education, health care, medical research and community collaborations. Its members comprise all 155 accredited U.S. and 16 accredited Canadian medical schools; approximately 400 teaching hospitals and health systems, including Department of Veterans Affairs medical centers; and more than 70 academic societies.
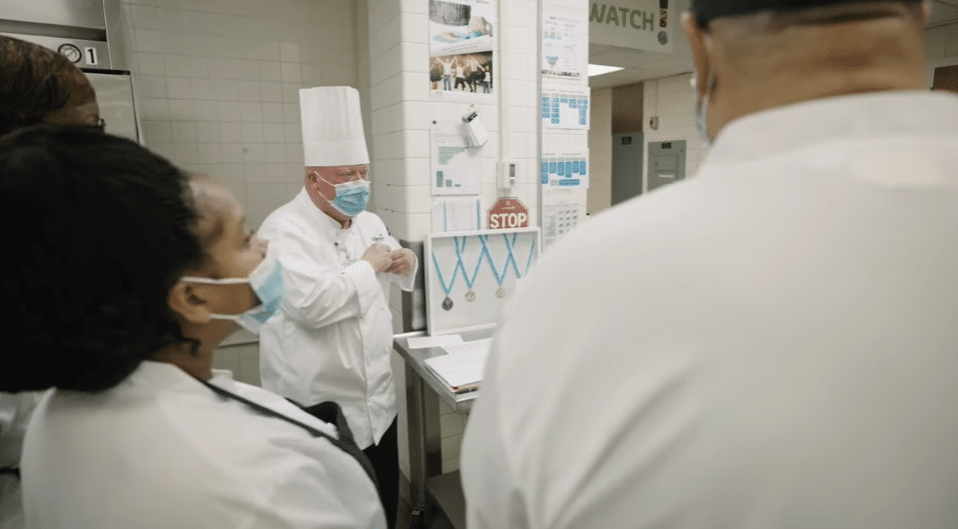
ECU Health Beaufort Hospital – a Campus of ECU Health Medical Center – is featured in a new documentary from the BBC. Produced by BBC StoryWorks Commercial Productions for The World Wide Fund for Nature (WWF), this documentary follows the Sodexo/ECU Health partnership, which shares a common goal to improve the health and well-being of the people and communities we serve.
Nearly one-third of food produced around the world ends up as food waste. Sodexo implements its WasteWatch program across all ECU Health hospitals to reduce food waste, drive cost efficiency and positively impact the environment. WasteWatch is Sodexo’s key initiative to achieve its objective of reducing 50 percent of food waste within its operations, covering 85 percent of its raw material costs. ECU Health Beaufort Hospital hosts one of the most efficient, highly successful Sodexo WasteWatch programs, producing very low amounts of food waste, which saves money and drives positive impacts on the environment.
The Beaufort team has been using the WasteWatch powered LeanPath program since August 2020, and they use the data and insights to put in place specific actions that have positive impacts for the environment. Team members tailor portions cooked each day based on data collected to reduce excess food, which helps preserve resources and reduce food waste.
“Taking care of our community and environment by doing our part to help reduce waste are values that our partnership with Sodexo helps us meet,” said Lou Montana-Rhodes, vice president of experience at ECU Health. “We are proud to recognize our food and nutrition team members at ECU Health Beaufort Hospital and all across eastern North Carolina for their commitment to leading the way in reducing food waste and bringing quality care to those we serve.”
ECU Health is proud to collaborate with Sodexo to bring high quality food and compassionate care to our patients.
With our continued focus on the imperatives of quality, experience and finance, ECU Health’s transplant program at ECU Health Medical Center has consolidated their treatment and office spaces into the newly renovated 3 South. The area is now known as the 3 South Transplant Clinic.
The transplant program performs an average of 80 to 100 living and deceased donor kidney and pancreas transplants per year. Patients that are seen in the clinic include pre-transplant (patients being evaluated for transplant), living donors and post-transplant. This program and the services offered have continued to grow over time, but have been limited by clinic space. To enhance patient and team member experience, the pre- and post-transplant clinics have now consolidated into one, centrally-designed space on 3 South, as they have been operating in separate clinics at the Cancer Center and ECU Physicians.
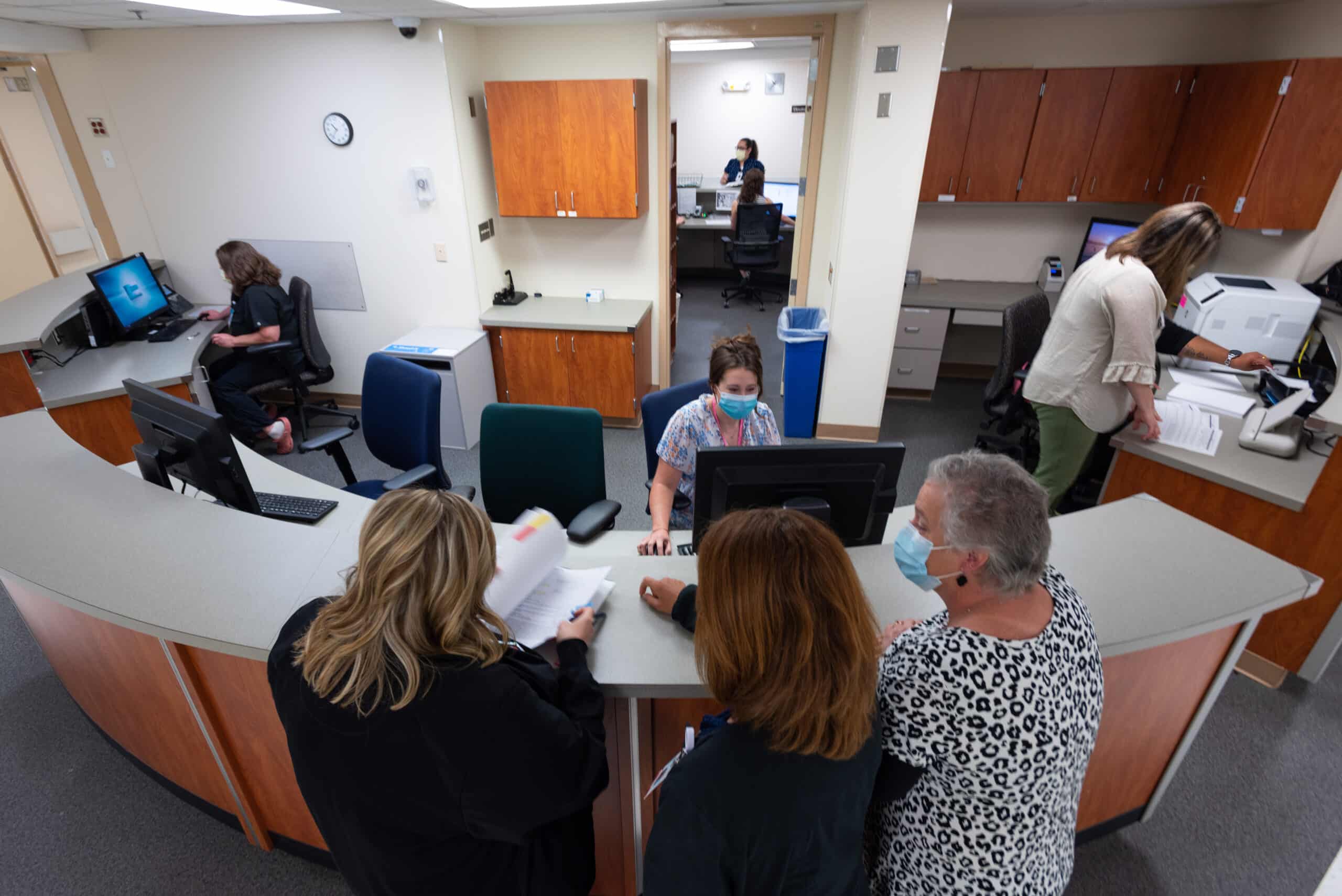
Previously, the transplant team worked in separate clinics, sometimes limited to three rooms. 3 South Transplant offers 18 patient exam rooms, which in addition to consolidating space for patients, will also help to shorten wait times for new referrals and follow up appointments.
Another benefit of 3 South is the accessibility of team members such as dieticians, social workers, pharmacists, nurses and physicians, which provides patients the accessible support of various teams of health care workers critical to patients’ transplant journeys.
Lastly, this consolidation allows for expansion of potential future services such as phlebotomy, expanded pharmacy services, infusion services and vascular access.
In 2022, as we build the future of ECU Health, the exceptional care and services we provide have a positive impact on the communities of eastern North Carolina that we serve through our considerations of patient quality and experience.
For more information on transplant services at ECU Health, visit the transplant section of our website.
The Brody School of Medicine at East Carolina University has experienced recent success in recruiting a diverse group of patients to participate in clinical trials for new medications and treatments.
Data shows that from March 2019 to March 2020, 202 patients participated in oncology clinical trials in ECU’s Division of Hematology and Oncology; 50 percent of them represented races other than white. The following year, 419 participants were accrued, and 56 percent represented races other than white. That year, 50 percent of clinical trials participants were Black or African American.
“Our patient population, as well as Brody’s mission, has led to our success,” said Susan Eubanks, clinical trials nurse specialist in Brody’s Division of Hematology and Oncology. “Part of our core values is to cultivate a clinical environment of robust learning, innovation and discovery. There have been trials with participants here in eastern North Carolina that have led to new treatments in diseases and in some cases where there were few options.”

Now, researchers and providers hope to build on that momentum for future clinical trials studies.
Providers and researchers in the school continue to seek minority participants in clinical trials for new and potential pharmaceuticals — and to collect invaluable information on how some treatments impact patients of various races.
Doctors want to ensure that the drugs they are studying match the demographics for all the patients who could rely on those medicines in the future — by including people from a wide variety of backgrounds and races in the studies.
“We all agree that as much as possible, the drugs we give should be approved through clinical trials that match the demographics they will be prescribed to,” Eubanks said. “There has been chemotherapy that has shown promising results in one country but doesn’t carry the day in another. So, overcoming this disparity — whatever the cause — is essential.”
One of the latest innovations in oncology is the use of immunotherapy, the treatment of disease by activating or suppressing the immune system. Data that reviewed participation in those trials showed that less than 4 percent of participants in key immune therapy trials were African American.
“This is a problem,” Eubanks said. “Given the low representation we can’t predict if there will be a differences in outcomes related to differences in response from tumor biology. It is not highly understood why we see differences in drug efficacy and toxicities among different ethnicities, but it drives the point home, we need to do all we can to include the best representation of our population when bring new therapies to market.”
Dr. Darla Liles, professor and division chief of ECU’s Division of Hematology and Oncology, said diseases like prostate cancer and colorectal carcinoma see more African Americans impacted than other races, and the diseases begin earlier in those patients as well.
“Also, the distribution of the DNA mutations are different across races,” she said. “We might have a drug that works wonderfully well in Caucasians but not so well in African Americans or Hispanic individuals because of these different DNA changes. But we only know that if enough minorities participate.”
Recruiting challenges
Even with the critical need for data that better illustrates potential patient outcomes, recruiting minority participants in clinical trials can be difficult.
“Accruing to clinical trials in general is difficult, but minorities are typically underrepresented in clinical trials,” Eubanks said. “This can be an access issue, a reluctance issue and, at times, both.”
There can be many reasons recruiting minority participants to clinical trials can be a challenge, Liles said, but keeping those reasons in mind and understanding that they vary from person to person help build trust.
Brody’s mission draws heavily on a theme of access for all: to a medical education, to health care, and to resources that can sustain health and wellness. That’s one reason access to clinical trials in the medical school is vital to the study and approval of novel treatments.
“Part of our commitment to the health care of all eastern North Carolinians is ensuring the pharmaceuticals and treatments that we study are safe and effective for every patient who may need them in the future,” said Dr. Michael Waldrum, Brody’s dean and CEO of ECU Health. “Our efforts to widen the participant base in our clinical trials programs reflects the importance of thorough and inclusive studies that yield results that we are confident meet our mission.”
Liles said that people are more likely to trust providers and those running clinical trials if they feel they share common bonds with them.
“Several times when I presented a trial to a patient, afterwards the CRA has told me that they went to high school with the patient or knew them from church,” she said. “Being able to relate to the people who are treating you is essential.”
Education is key as well, Liles said.
“When I offer a trial to a patient, I often understand this is starting a conversation over several visits to ensure patients know about and understand what they are signing up for,” she said. “The consent forms for clinical trials are jam-packed with important information about the treatments, and sometimes people use that as a starting point for knowing what to ask about their treatment. I never regret giving a patient a consent form and talking to them about a trial. Even if they eventually decide not to do it ,they are better informed by participating in the process.”
Eubanks said the COVID-19 pandemic and reluctance by some to take the vaccine are a reminder of how to approach building trust in clinical trials.
“We must think beyond just education in the office,” she said. “We must reach people where they are.”
One way Brody is working to reach many different patients is having trials open for a variety of specialty care areas.
“The biggest step is understanding your population and having trials open for the specialty areas you see,” Eubanks said. “Brody has trials open with many specialties. In adult hematology/oncology we use databases and the tumor registry when approached about upcoming trials to help us determine if a trial is potentially feasible in our area. We also have the benefit of having local resources such are the University and Medical Center Institutional Review Board (UMCIRB) and leaders such as our associate dean for research and graduate studies, Dr. Russ Price, that provide expertise and infrastructure needed to offer clinical trials.”
Liles uses word of mouth to share clinical trial opportunities to patients.
“I often tell my patients about new and innovative trials that are on the horizon, even if they do not fit the criteria for the trial,” she said. “I think it is important for patients to understand that there are new things being developed all the time. Education is our best way to ensure patients know about and participate in trials.”
Liles also believes the combination of specialties and resources in the creation of the ECU Health brand will have a positive impact on the clinical trials program. With close to 1.4 million people in the system’s service area, there is promising potential to reach people through improved infrastructure for research opportunities.
Read more from ECU News Services.