Joshua Thomas, a lively and spirited seven-year-old, has never let his severe form of Osteogenesis Imperfecta (OI), commonly known as brittle bone disease, dampen his spirit or excitement for life.
“Joshua is full of life,” said his mother, Shakeema Thomas. “Even with everything he’s been through, he’s very active.”
Brittle bone disease is rare, impacting about 25,000 to 50,000 people in the United States, according to the National Institute of Health. The genetic disorder means Joshua’s bones are fragile and prone to frequent fractures. Over the years, Joshua has experienced a series of challenges, including approximately ten femur fractures, often from falling or seemingly harmless movements like repositioning in bed.
According to Shakeema, Joshua has broken the same femur bone about ten times. When Joshua sustained yet another displaced femur fracture, his family turned to Dr. Michael Firtha, a pediatric orthopedic surgeon at ECU Health who has treated both Joshua and his fifteen-year-old brother—who also has OI—for multiple fractures over the years.
“Displaced femur fractures in kids with osteogenesis imperfecta are difficult problems with limited options,” said Dr. Firtha. “You have to consider fixing the bone, allowing continued growth and preventing future fractures in the same area.”

In the past, Joshua’s treatment included body and leg casts, but these approaches didn’t prevent recurring injuries. Determined to find a solution that worked better for Joshua, Dr. Firtha surgically implanted a telescoping metal rod, a procedure that was first-of-its-kind at ECU Health.
This innovative implant stabilizes the fractured bone while allowing it to grow naturally. As Joshua’s femur lengthens, the rod telescopes along with it, providing long-term protection without hindering development.

“This technology is a game-changer,” Dr. Firtha said. “It lets us fix the bone, promote healing and ensure Joshua’s growth isn’t compromised. I’m fortunate to work in a health system that prioritizes patient outcomes and embraces advanced technologies.”
The results have been transformative. Since the surgery, Joshua has had a few minor falls that would have previously resulted in fractures but did not this time. For Shakeema, the change is nothing short of remarkable.
“We’re so grateful for the care Joshua has received, and Dr. Firtha is so amazing,” Shakeema shared. “He’s doing well so far, and he’s completing physical therapy now every day to get stronger.”
Joshua’s story is a testament to the importance of advanced techniques and technologies that improve the quality of life to patients with rare and challenging conditions. To learn more about ECU Health Orthopedics, please visit ECUHealth.org/ortho.
It’s been a year since the state of North Carolina passed Medicaid Expansion, bringing with it much-needed coverage and financial reprieve for the communities ECU Health serves.
North Carolina’s former governor, Roy Cooper says “One year of Medicaid expansion in North Carolina,” said Dr. Michael Waldrum, ECU Health CEO and Brody School of Medicine’s dean. “As we celebrate this moment. We’re proud to say we’re building the national model for rural health care right here in eastern North Carolina.”
That model depends on Medicaid Expansion and affordable access to care.
“It is a comprehensive health benefit where you can go see a primary care provider, have it covered,” said Kody Kinsley, secretary of the North Carolina Department of Health and Human Services. “Where you can have pharmacy, vision and dental and a copay that is never more than four dollars.”
Cost-effective health care is an important component, but it’s not the only one. ECU Health’s Dr. Karen Coward states “This is the power of Medicaid expansion. It’s not just about providing coverage, it’s about dignity.”
And peace of mind for the patients who need it most. Medicaid Expansion beneficiary and ECU Health patient, Darcy Guill spoke during the event.
“Sixteen years ago, I found myself unable to work and I lost my health insurance,” Guill said. “For the next 15 years, I was either uninsured or under insured.”
Her inconsistent coverage hit home in a different way following a car accident.
“I was hospitalized for two months right here at ECU Health,” Guill said. “I knew I was going to be uninsured again and I didn’t know what to do and I was terrified.”
That panic subsided when she realized share now had another option.
“It didn’t dawn on me at first that it was going to include me but it did,” she said. “Medicaid is literally saving my life. I am the person that benefitted from it and I am no different than all the other people that could benefit.”
Greenville, N.C. – ECU Health, the health system serving eastern North Carolina, marked a year of clinical advancements, record recruitment, expanded access to care, academic growth and national recognition in 2024. The health system’s progress demonstrates its unwavering commitment to improving health outcomes for the region’s rural communities.
“At ECU Health, 2024 was a successful year marked by groundbreaking innovations, impactful collaborations and significant achievements that solidify our position as a national model for rural health care,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University.

“From advancing academic excellence and clinical innovation to expanding access to care, these milestones reflect the unwavering dedication and hard work of our exceptional team members. As an exciting new year begins, we remain committed to building on this momentum to address the unique health care needs of our communities with a focus on meeting our mission of improving the health and well-being of eastern North Carolina.”
A few key highlights from 2024 include: celebrating the first graduating class of its Rural Family Medicine Residency Program and also expanding class sizes moving forward, investing in research with the Brody School of Medicine, introducing innovative technologies such as the BEAR® Implant, FARAPULSE™ and EluPro® BioEnvelope to enhance patient outcomes and offer state-of-the-art treatment options, and the system earning several prestigious recognitions, including becoming the only Level I Pediatric Trauma Center in eastern North Carolina and one of four in the state, Electrophysiology Lab accreditation and Magnet® designation for nursing excellence, and hosting the one year anniversary celebration of Medicaid expansion, highlighting the number of eastern North Carolinians who now have access to health insurance.
More 2024 highlights include:
- ECU Health Medical Center received The Joint Commission’s Gold Seal of Approval® for brain tumor care.
- ECU Health strengthened its network with the opening of the Outer Banks Health Cancer Center, groundbreaking for Outer Banks Health Family Medicine in Manteo, the launch of the JOY Clinic and the ECU Health and Pitt County Health Department’s vaccine and health assessment clinic for local kids.
- ECU Health achieved record recruitment of physicians and nurses committed to the ECU Health mission.
- ECU Health expanded access to primary care access by adding 198 new primary care providers and opening more than 900 new primary care appointments per week.
- ECU Health celebrated the first graduating class of its Rural Family Medicine Residency Program and expanded the class size.
- ECU Health started fellowships in Electrophysiology and American Sign Language.
- The Brody School of Medicine broke ground on its new Center for Medical Education, a step toward increasing its class size from 86 to over 120 students, addressing the growing need for physicians in the region.
- ECU and ECU Health’s NC-STeP program received a national achievement award by the American Psychiatric Association.
To explore more milestones and highlights from 2024, visit ECUHealth.org/YearInReview2024.
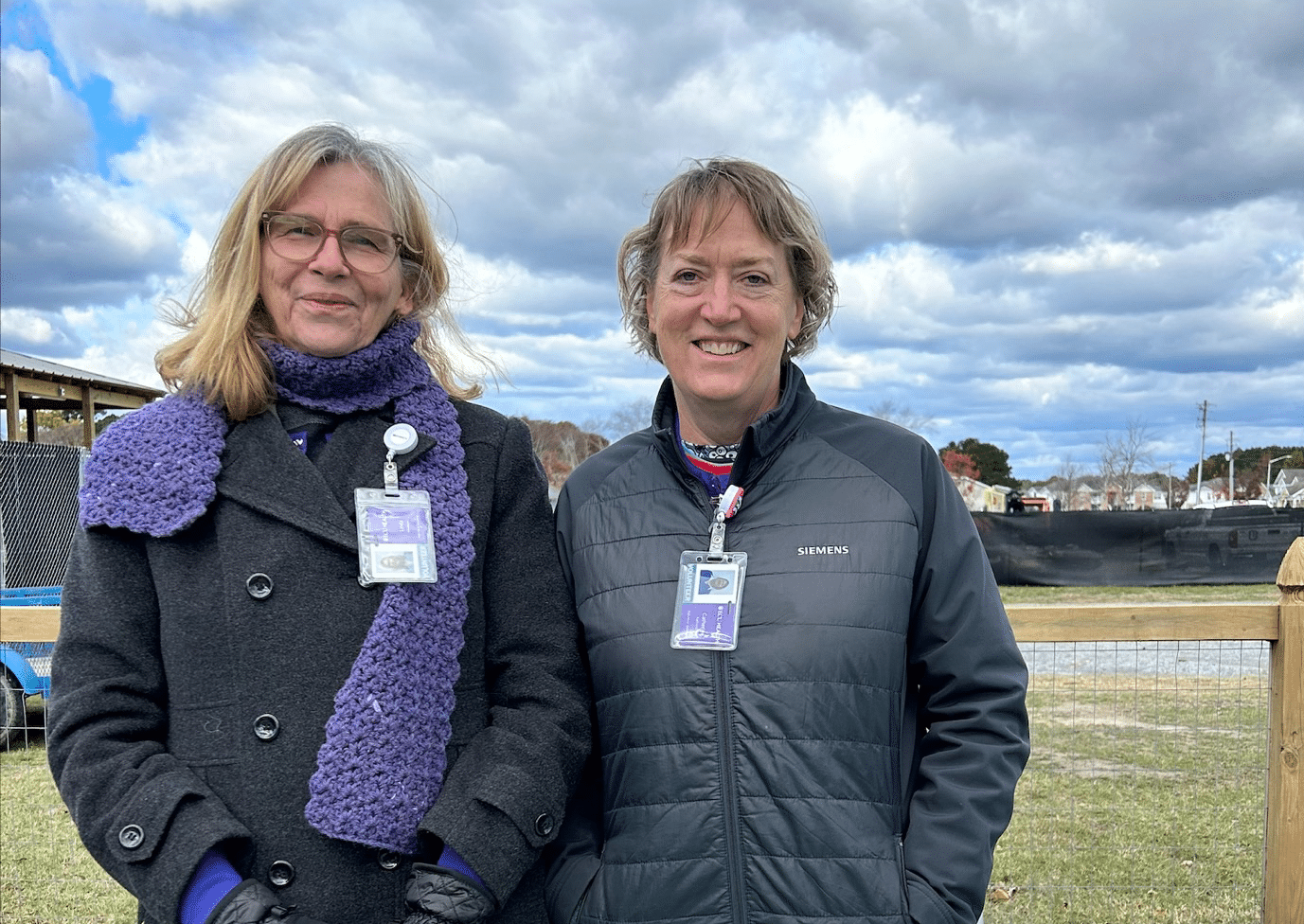
Nurses and Child Life staff from ECU Health brought the Teddy Bear Hospital to Northwest Elementary School in Pitt County on Tuesday, Dec. 17, as part of the Pitt County Health Sciences Academy. Nearly 130 kindergarten and first-grade students participated in the event, designed to introduce young children to health care professionals in a welcoming and interactive setting.
Dressed in scrubs and personal protective equipment (PPE), the students acted as caregivers for their favorite stuffed animals. They guided their “patients” through the health care process, starting with check-in and triage. ECU Health nurses examined the stuffed animals, provided a diagnosis, and directed the children to one of three stations: Sutures & Bandages, Operating Room, or Clinic. Afterward, the students and their stuffed animals visited the recovery area, where each received a certificate of bravery.
“This event offers a unique and playful way to familiarize children with health care professionals,” said Nancy Turner, workforce development consultant at ECU Health. “By engaging with the students in a hands-on setting, we’re helping to make health care less intimidating while sparking curiosity about health-related careers.”
Turner emphasized the impact of early exposure to health care.
“When kids see the process in a fun and supportive environment, it not only eases fears about doctor’s visits but also shows them that health care is approachable and full of possibilities,” said Turner.
For many students, the Teddy Bear Hospital is just the beginning of their exploration of health care. ECU Health team members, in collaboration with the Health Sciences Academy, host a variety of programs for middle and high school students, including job shadowing, career fairs and events like “Chat with a Doc.”
“The goal is to engage students at every stage of their education,” said Turner. “Starting in elementary school, we show them that health care careers are diverse and accessible. Whether their interests lie in nursing, technology, or another area, there’s a role for everyone in health care.”
These programs reflect ECU Health’s commitment to inspiring the next generation of health care professionals while building a strong, local pipeline of talent to serve eastern North Carolina.
The Pitt County Health Sciences Academy is a partnership between ECU Health, Pitt County Schools, Pitt Community College, East Carolina University, the Brody School of Medicine, Colleges of Allied Health Sciences, Engineering and Nursing at East Carolina University, School of Dental Medicine at East Carolina University, the Eastern Area Health Education Center and the Greenville-Pitt County Chamber of Commerce.
ECU Health Beaufort Hospital, a campus of ECU Health Medical Center, brought the community together to celebrate healthy living at its third annual Fall Harvest Event. Held at the Community Well-Being Zone next to the ECU Health Wellness Center in Washington, the event offered fresh produce, free health screenings and opportunities to learn about nutrition and wellness.
Attendees harvested sweet potatoes, leafy greens and fresh herbs, while enjoying the educational atmosphere. The space, designed to promote wellness and community engagement, includes 10 raised beds for vegetables, two large planters for herbs, a storage shed and areas for outdoor learning.
“This event is about more than just providing fresh vegetables,” said Dr. Tammy Thompson, ECU Health’s Director of Experience, Engagement, Education and Design. “We’re fostering wellness habits and creating a space where the community can connect, learn and thrive. Hosting this event by the Wellness Center also allows us to showcase the resources available to help community members live healthy lifestyles.”
In addition to the harvest, the event featured free health screenings on a mobile bus and tours of the ECU Health Wellness Center. Community members received guidance on growing food at home, nutrition tips and exercise information, further emphasizing the importance of holistic health. The event provided fresh vegetable soup for attendees, and warm apple cider as they toured the garden.

The event’s success was also supported by partnerships and volunteer efforts. The Conetoe Family Life Center contributed additional produce for attendees, while an East Carolina University Public Health intern welcomed guests and shared educational resources.
Volunteers like Cathy Karlovich, were thrilled to be part of the initiative.
“Healthy eating is very important to me,” Karlovich said. “I understand how eating well can impact your whole life, so doing something like this for the community and sharing valuable information is really special.”
Thompson encouraged the community to get involved, noting that volunteer opportunities are available for those interested in supporting the garden and its mission.
“My hope with events like this is to cultivate not just a garden, but a healthier, more connected community,” Thompson said.
The garden is open to community members from 9 a.m. to noon each Wednesday and Friday where any produce ready to be harvested will be distributed and other educational materials will be shared. For more information, please visit ECUHealth.org/WBZ
The remedē System is an innovative, FDA-approved medical implant indicated for adult patients with Central Sleep Apnea (CSA)—and it’s now an available treatment option for certain ECU Health patients. CSA is an abnormal breathing pattern that disrupts normal breathing during sleep; there is a disconnect between the need to breathe and the brain sending signals to the diaphragm. Symptoms include chronic fatigue, irritability and brain fog, but there are other secondary outcomes to sleep apnea, such as worsened heart arrythmias and congestive heart failure. The remedē System provides a significant advance in the treatment of CSA when other interventions are not effective.
The remedē System is implanted beneath the collar bone with one or more leads that are placed near the phrenic nerve. The device then delivers mild electric impulses that stimulate the phrenic nerve, which signals to contract the diaphragm and helps patients breathe when there’s an absence of that stimulus from the brain.

After programming the device, the system turns on when the patient lies down to rest during their normal sleep time. Dr. John Catanzaro, the division chief of cardiology at East Carolina Heart Institute, sees the remedē System as an important option for patients with CSA. “There’s a very low risk with this treatment, and phrenic nerve stimulation is a contemporary option for patients with CSA who haven’t responded well to other therapies,” he said.
Patients undergo a screening process at ECU Health’s Sleep Center to determine their eligibility for the procedure. After implanting the device, the surgical team tests it to ensure it works and the patient doesn’t have any side effects. Once the implantation site is healed, the Sleep Center team takes over to determine how to administer the therapy and restore the patient’s sleep pattern.
To get this technology to ECU Health, it required collaboration among professionals from different disciplines, including Dr. Zia Rehman, the medical director of the Sleep Center, Dr. Rajasekhar Nekkanti, cardiologist, professor and director of the Cardiology Fellowship and Dr. Sam Sears, a professor in ECU’s departments of psychology and cardiovascular sciences and an expert on the psychological care and quality of life outcomes of patients with implantable defibrillators.
That the remedē System specifically treats CSA is an important distinction, especially since ECU Health is now the only place in North Carolina other than Winston-Salem to offer the procedure. This provides care to a significant population and will provide an overall improvement in patients’ quality of life while resulting in fewer hospitalizations – achievements that align with ECU Health’s mission and values. “We want ECU Health to be a leader in health care for the state of North Carolina and beyond,” said Dr. Rehman.
The intent is that the program will treat 12-15 patients the first year, with the goal to serve 35 – 40 patients annually after that. To learn more about sleep apnea, including the use of remedē as a treatment option, visit https://healthlibrary.ecuhealth.org/Search/85,P01301.
While Heather Duncan, the director of ECU Health Medical Center’s laboratory services, knew she wanted to work in health care from an early age, her career plans changed when she learned about the medical technologist program at her school. “I thought I’d be a dermatologist,” she recalled. “But I liked biology and science, and the medical tech program fit my interests. That steered my career, and I’ve never looked back.” The South Carolina native has served in her current role at ECU Health for six years, and she is now wrapping up her four-year term with the Clinical Laboratory Improvement Advisory Committee (CLIAC), which is an appointed position. During her time with CLIAC, Duncan has been instrumental in bringing positive change to her profession.
CLIAC is a federal advisory committee that provides guidance to the Department of Health and Human Services (HHS) and is managed by the Centers for Disease Control and Prevention (CDC). The advice and guidance the committee provides pertains to general issues related to improvement in clinical laboratory quality and laboratory medicine practice.
Duncan said she didn’t even know CLIAC existed until a former co-worker approached her to gauge her interest in being nominated for a position. “They asked me if I would be interested, and it was exciting because CLIAC is so impactful.”
In the past four years, Duncan said she’s been privileged to collaborate with 20 other professionals to develop educational resources for the lab community and update the CLIA regulations. During her tenure, Duncan chaired the CLIAC Certificate of Waiver (CoW) and Provider-performed Microscopy (PPM) Procedures workgroups.

“The work that has come out of those groups has allowed CLIAC to make recommendations to modernize our regulations, which impact the laboratory community at large. We’ll see those impacts here at ECU Health,” Duncan said.
One such regulation restricts who is allowed to train new personnel to perform certain functions in the lab. With Duncan’s work, the regulation has now expanded to allow more people in the lab community to perform that training. “Because there is such a workforce shortage with laboratory technicians, this is impactful by expanding who can provide training, and it improves the overall quality of lab testing,” Duncan said. Caryl Havasy, the system administrator for laboratory services, sees Duncan’s work with CLIAC as instrumental in gaining more lab technicians. “ECU Health, like other health systems, faces an ongoing shortage of laboratory testing personnel. Heather’s experience in laboratory operations and regulatory compliance in our rural-focused health system brings a much-needed perspective to the work of CLIAC, specifically its role in creating the regulatory structure that defines the qualifications for frontline laboratory roles,” Havasy said.
Another exciting recommendation that emerged from the most recent CLIAC meeting would allow for virtual competencies, which would expand training capability and incorporate cutting edge technology into practice. “Because we serve rural communities, having this technology would cover a huge network,” Duncan shared. “We have benefitted from having a direct pipeline to the work CLIAC is doing. For example, our lab was one of the initial beta testers for virtual lab safety training. They sent us four Oculus headsets and they push new training programs to us.”
While this technology isn’t widely used yet, Duncan said being a part of an organization that promotes advancements in technology and makes recommendations on a federal level is gratifying. “This work allows for a forward-thinking process, and it will impact our whole community,” she said. “Our vision is to be the national model for rural health care, so we should use every tool available. Being a part of CLIAC means I’ve been able to make a real difference.”
Havasy highlighted other areas CLIAC and Duncan’s work with the committee makes an impact, including, “a change to rules surrounding histocompatibility testing (performed to match organ donors with recipients, i.e., kidney transplants) that will remove specific requirements for obsolete methods and practices, accept newer testing techniques and eliminate redundant requirements. This will result in a decreased compliance burden on the laboratory and more efficient testing for our eastern NC kidney transplant patients.” Duncan also worked with the CoW workgroup, which addresses regulations as they pertain to labs with a Certificate of Waiver. This waiver is granted to labs that only perform waived tests, which are simple laboratory procedures and examinations with a low risk of an incorrect result (including urine pregnancy tests or blood glucose monitoring). Labs must pay certification fees every two years to acquire and maintain the certificate. Duncan explained that one area her workgroup focused on was an updated fee schedule. “CLIA is a self-funded program, and they haven’t updated their fees in a long time,” Duncan explained. The group also worked on establishing a broader range of sanctions for laboratories that operate under a Certificate of Waiver but are not compliant with the CLIA regulations.
Because of her work with CLIAC, Duncan said ECU Health has a seat at the table and can provide input for advancements in laboratory operations. “Through these efforts,” Havasy added, “Heather embodies the ECU Health vision of bringing our rural health care system needs and potential solutions to a national stage, impacting not only our own operations but those of every health care system across the country.”
Greenville, N.C. – ECU Health and the national nonprofit Undue Medical Debt are pleased to announce an initiative that will help eliminate more than $186 million worth of past-due hospital medical debt for more than 32,000 qualifying patients. Debt relief letters will arrive over the course of December’s holiday season into the New Year on a rolling basis given the size of this relief effort
Eligible community members do not need to apply, and there is no application process. Instead, community members who qualify for this one-time debt relief will receive a branded letter from Undue Medical Debt indicating which past-due hospital debt or debts have been eliminated. Undue Medical Debt works with hospital systems and other providers across the country to purchase past due medical debt belonging to those least able to pay in large portfolios for pennies or less on the dollar and then erases the debt.

ECU Health’s collaboration with Undue Medical Debt pre-dates North Carolina Department of Health and Human Services’ medical debt relief initiative which spans all hospitals in the state and lays out a plan for medical debt relief coupled with changes to Medicaid/Medicare reimbursement policy and financial aid standards in 2025.
Under Undue Medical Debt guidelines, those who qualify for this medical debt relief have hospital medical debts that are 5% or more than their annual income or earn at or below four times poverty-level income. The current federal poverty level is an annual income of under $31,200 for a family of four which means a qualifying family of four would make under $124,800. Community members do not need to take any action, as the eligible hospital medical debt will automatically be eliminated for those who qualify.
“We’re grateful to collaborate with ECU Health to help ease the burden of medical debt in eastern North Carolina,” said Undue Medical Debt CEO and President Allison Sesso. “Helping community members burdened by medical debt takes thoughtful collaboration and I’m proud of the results: over 30,000 people helped this holiday season. We hope this program provides financial and emotional relief to recipients and encourages them to continue engaging with the healthcare system.”
The collaboration with Undue Medical Debt is one of many ways in which ECU Health is living its mission to improve the health and well-being of eastern North Carolina. The initiative aligns with the health system’s commitment to serving underserved communities in the East, many of which have disproportionate numbers of low-income and uninsured or underinsured people. The initiative is also in alignment with ECU Health’s long-standing practice of non-predatory billing practices, which emphasize charity care, zero-interest payment plans, transparent pricing and dedicated resources to help patients navigate financial requirements.
“At ECU Health, our commitment to our mission and patients is at the heart of all we do,” said ECU Health Chief Operating Officer Brian Floyd. “We have always been guided by a deep desire to support our patients in whatever way we can, and this collaboration with Undue Medical Debt will make an enormous impact on so many in our largely underserved region. We could not be more thankful to find an organization like Undue Medical Debt which shares our vision for making high-quality rural health care accessible here in eastern North Carolina.”
Greenville, N.C. – ECU Health, eastern North Carolina’s leading academic health care system, has named Todd Hickey, MHA, FACHE, as president of ECU Health North Hospital, effective Jan. 1, 2025. Hickey will serve as president of ECU Health North in addition to continuing his current role as chief strategy officer for the health system.

“I could not be more pleased to welcome Todd into his new role as president of ECU Health North Hospital,” said D. Van Smith, MBA, MSHA, ECU Health Community Hospitals President. “Todd brings more than 20 years of experience in health care operations, strategic planning and leading transformational change to the role, and I am confident he will continue to guide ECU Health North Hospital in service to communities in the northeastern part of our region. I want to also thank Dennis Campbell for his leadership as the interim president at North over the last six months.”
Hickey joined ECU Health in 2008, serving in service line and hospital operations executive leadership roles at ECU Health Medical Center until becoming the health system’s first Chief Clinical Network Development Officer in 2016. In this role, Hickey successfully led and implemented joint ventures, service line expansions, an integrated population health model and key acquisitions, including the integration of Halifax Memorial (now ECU Health North Hospital) into ECU Health in 2019. He transitioned to Chief Strategy Officer in 2022 which expanded his oversight to include developing and guiding the ECU Health enterprise 3–5-year strategic plan.
“It is an honor to serve as president of ECU Health North Hospital,” Hickey said. “I am fortunate to have had the opportunity to help bring ECU Health North into the ECU Health system and I have a deep appreciation for the important role it plays in Halifax County, Roanoke Rapids and the surrounding communities. I am excited to work with the ECU Health North team to continue advancing the legacy of providing high-quality, compassionate care.”
In recognition of the one-year anniversary of Medicaid expansion in North Carolina, Gov. Roy Cooper visited ECU Health Medical Center in Greenville to reflect on the impact of expansion and celebrate a year of reaching North Carolinians in need.
Since Medicaid expansion officially launched in North Carolina on Dec. 1, 2023, more than 80,000 eastern North Carolinians and nearly 600,000 people statewide have benefited from access to vital health insurance. Along with Medicaid expansion, the state also passed the Healthcare Access and Stabilization Program (HASP), which provides critical relief to rural hospitals.
Gov. Cooper said Medicaid expansion’s reach in rural communities, like ECU Health’s 29-county service area, has been especially impactful in the last year.
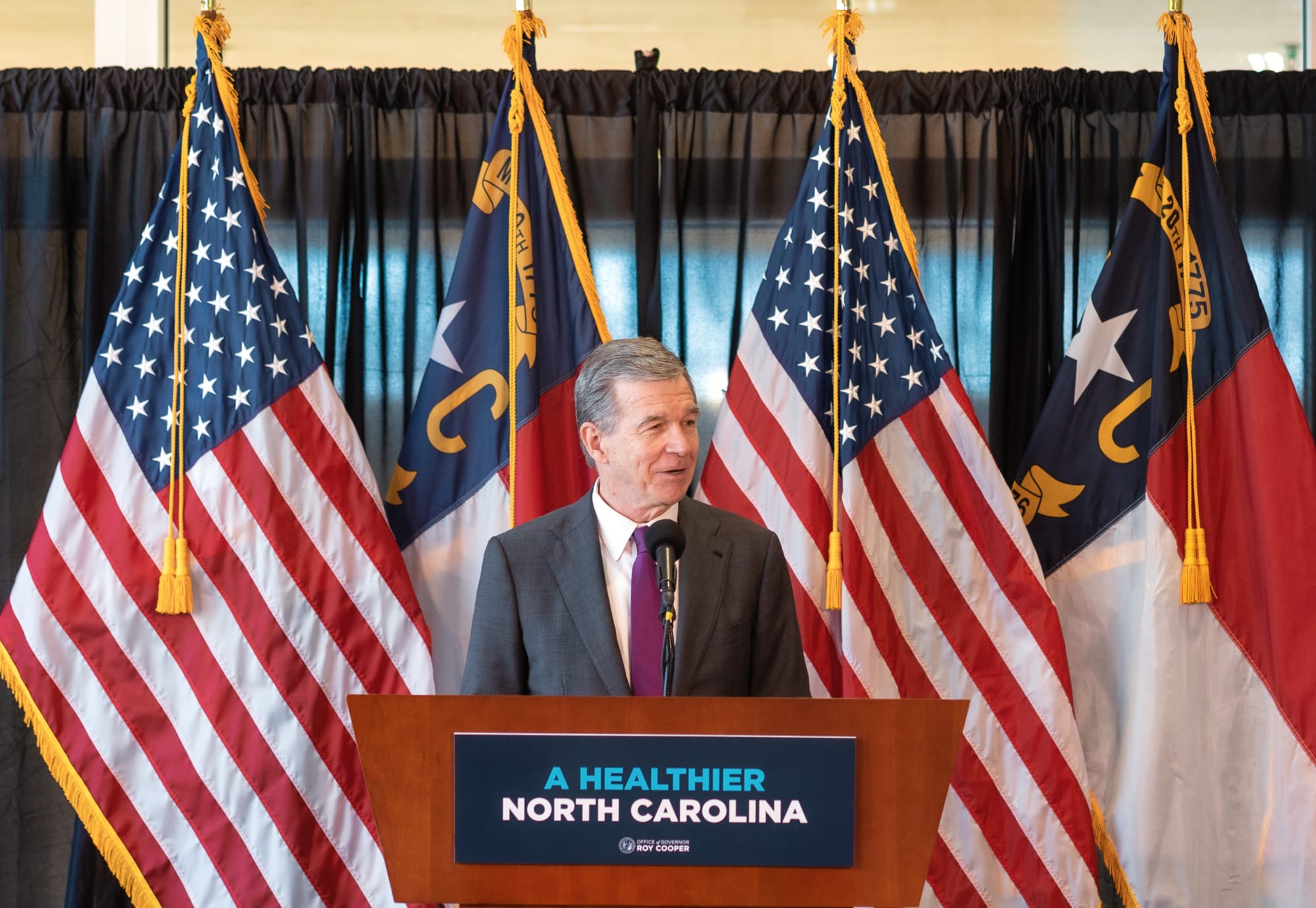
“The last year showed us that this is something that people desperately needed, particularly here in rural North Carolina,” Gov. Cooper said. “I grew up in Nashville and we know that rural North Carolinians have been helped more by Medicaid expansion than anyone else. I hold close to my heart the mission of getting people healthier. I knew getting Medicaid expansion passed and signed into law was the most important thing we could do to accomplish that.”

This milestone reflects the culmination of more than six years of advocacy by ECU Health, driven by the challenges faced by uninsured and underinsured patients.
Dr. Michael Waldrum, ECU Health chief executive officer and dean of the Brody School of Medicine at East Carolina University, said Medicaid expansion and HASP funding is creating real differences for patients, health care workers and the future of health care in places like eastern North Carolina.
“Medicaid expansion has helped improve access to primary care, empowering people to take control of their health and their lives,” Dr. Waldrum said. “It is also an investment in rural health organizations like ours. At the same time and in partnership with the state, ECU Health and the Brody School of Medicine are also committed to doing their part to support primary care expansion efforts in rural health care.”
He highlighted the expansion of the Rural Family Medicine Residency program, which will train nine rural residents per class across three training sites in the East and the upcoming Center for Medical Education Building on Brody’s campus. This investment has helped and will continue to help ECU Health and Brody serve the combined mission of improving the health and well-being of eastern North Carolina.
Dr. Karen Coward, a family medicine physician with ECU Health, is a Kinston native and practices in Tarboro. She said she knew by age 10 she wanted to be a family physician in her home community. She attended Brody and stayed true to her dream of serving eastern North Carolina.
She said before Medicaid expansion, many of her patients would rely on the emergency department for care. Even if a patient was connected with primary care, it was difficult for them to follow through with appointments or afford medications. Chronic conditions like diabetes, hypertension or even cancer would go unchecked. Now, she said, she’s seen a life-changing shift.
“Patients who once cycled through the emergency department are now establishing relationships with primary care providers like me,” Dr. Coward said. “They are keeping their appointments, following through on recommendations, treatments, and gaining access to medications and specialist referrals that were previously out of reach. For many, this will mean earlier diagnoses and interventions, reducing the burden of advanced diseases.”
Kody Kinsley, secretary of the North Carolina Department of Health and Human Services, joined the event and said that in the past year over $58 million in dental claims alone were filed, millions of prescriptions were filled and hundreds of millions of dollars in claims supporting hospital care were taken care of through Medicaid expansion.
He said this comprehensive health insurance is already making a real difference for individuals and families.
“Medicaid expansion is life changing for families,” Sec. Kinsley said. “It is peace of mind for people as they sit up late at night thinking about how the next day will impact them. Will a sickness impact their family? Will they end up in debt? They don’t have to worry about that anymore.”

The event also included remarks from a Medicaid expansion beneficiary, Darcy Guill from Ayden, who shared her gratefulness for regular care she’s receiving, specialists she’s able to visit and prescriptions she can fill, thanks to Medicaid expansion.
As we look back over the previous year, we’re proud to build the national model for rural health care here in eastern North Carolina at ECU Health and we’re grateful for the support the region and health system through Medicaid expansion and HASP.