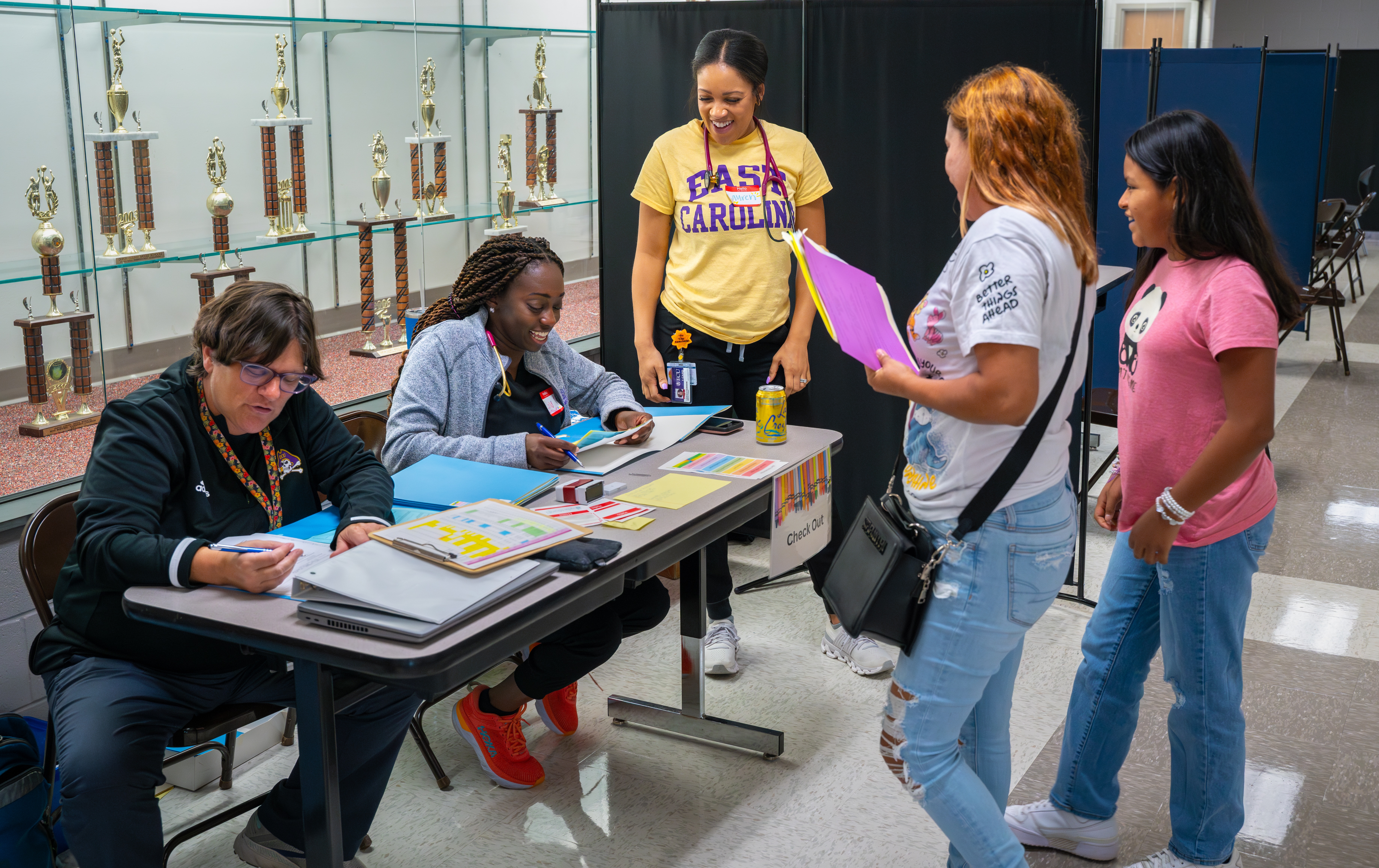
In September, the Healthier Lives at School and Beyond program, an initiative led by the Brody School of Medicine at East Carolina University and ECU Health, hosted an event at Rose Hill-Magnolia Elementary School in Duplin County to help keep 51 students in school by providing health assessments for students.
In North Carolina, students without a health assessment or immunization record on file 30 days after the start of the school year are suspended from school which can disrupt the learning experience.
In previous years, the Healthier Lives at School and Beyond team also visited schools in Jones County and Clinton City Schools in Sampson County to ensure students are up to date on their care and can remain in the classroom.
Dr. Kristina Simeonsson, professor of pediatrics and public health at Brody, said these events are crucial for rural areas like Duplin, Jones and Sampson counties who do not have the same access to primary care as larger counties.
“These are often children who are new to the area, new to the state and possibly new to the country, who haven’t had a chance to establish with a health care provider but desperately need these health assessments done,” Dr. Simeonsson said. “We do these events in September in partnership with the county or city schools along with the county health department to get as many kids seen as possible so that they won’t miss school.”

Healthier Lives at School and Beyond was originally designed as a school-based telehealth program that provides quality nutrition education and counseling, behavioral health, and acute minor medical care services. It officially launched in 2018 to deliver interdisciplinary services virtually to rural school children, staff and faculty during the school day. Whether in school or at home, all appointments take place over a safe and secure online network which allows patients to stay at school or home and parents to stay at work or home.
But in 2020, when many community members had not seen a primary care provider due to the COVID-19 pandemic, the team received a request from Duplin County schools to catch students up on health assessments. The following year, the team realized the need was larger than they anticipated and the program eventually spread to other areas of eastern North Carolina.
“We thought that was a unique situation for COVID and wanted to do everything we could to support our school partners,” Dr. Simeonsson said. “We’ve seen this program grow because there are just so many kids that need the service. Every year we’ve tried to tweak and get a little more efficient, we’ve had medical students, residents and nurses come back if they’ve done this before to help out. Every year we’re getting a little more efficient.”
During the visit to Rose Hill-Magnolia Elementary School in September, Dr. Simeonsson said the team chartered a retrofitted motorcoach from ECU Transit to provide further screenings.
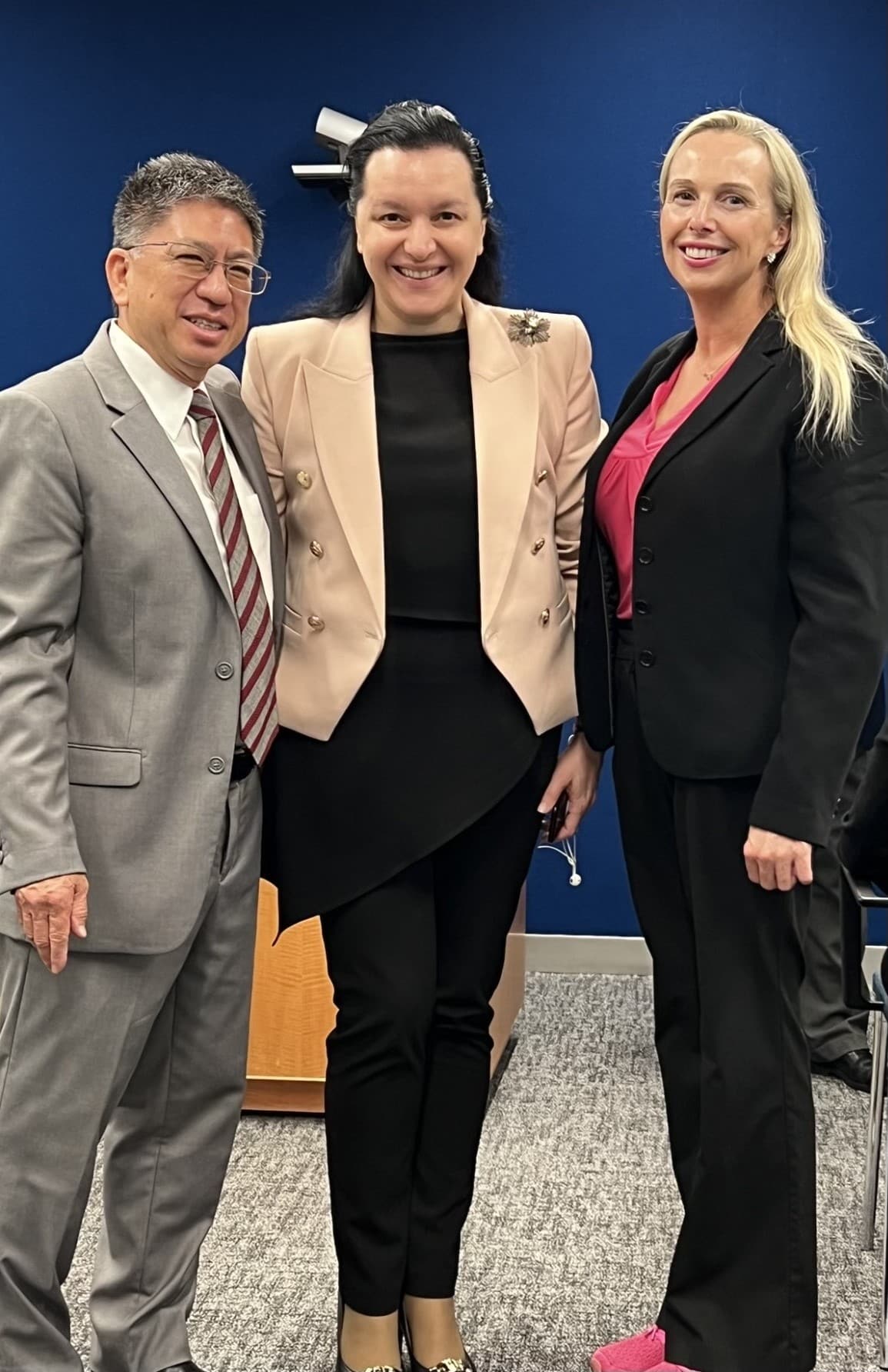
Six physician residents from ECU Health and three medical students from Brody were on hand to help for the Rose Hill-Magnolia Elementary School event. Among the residents were Dr. Maria Canas, a first-year resident, and Dr. Cady Hansen, a third-year resident.
Dr. Hansen said from a training perspective, the experience is invaluable.
“I think exposure and getting out in the community is so important,” Dr. Hansen said. “We’re connecting with the community and we’re treating patients, but it’s more than that.
This allows us to get a much different perspective into the levels of medicine needed in different areas and what people have access to and trying to ensure that we provide the best level of care across populations.”
Dr. Canas, who is from Colombia, was able to connect directly with Spanish-speaking students and families while providing care at the school. She said being a resource for Spanish-speakers made the day special for her.
“I love that. I really appreciate this opportunity,” Dr. Canas said. “It’s really nice because sometimes I get comments like, ‘I’ve never seen a provider speaking Spanish.’ It’s just nice because they can feel a little bit more comfortable speaking to me because it’s the same language and it’s not easy when you don’t have that.”
Sue Ellen Cottle, lead school nurse for Duplin County Schools, said the day was a success and each year she looks forward to the team coming together to do this important work. To date, 354 health assessments have been completed which have enabled 354 students to remain in school.
“We are very fortunate in Duplin County to have the partnership with Brody and ECU Health because otherwise these students would be out of school as of tomorrow morning,” she said. “We’ll do everything from pre-K through 12th grade today, physicals, immunizations, whatever they need to stay in school. We’ll see 51 students today and we’re just thrilled to partner with the team on this.”
Through programs like Healthier Lives at School and Beyond, Brody and ECU Health are living their missions in important and unique ways. The program is exposing Brody medical students and resident physicians to unique care environments and is working to increase the supply of primary care physicians serving the state ultimately to improve the health and well-being of the region. For ECU Health physicians and team members connected to the work, it directly drives forward the mission to improve the health and well-being of eastern North Carolina.
Working together with local partners makes the East a stronger, healthier community and helps ECU Health and Brody meet community members where they are to deliver high-quality, compassionate care.
Greenville, N.C. – ECU Health Medical Center has earned The Joint Commission’s Gold Seal of Approval® Certification for brain tumor care, recognizing the program’s ongoing dedication to delivering safe, high-quality patient care. According to The Joint Commission, the Gold Seal is a symbol of quality that recognizes health care organizations that provide comprehensive care for patients with brain tumors.
“This recognition from The Joint Commission is a testament to the incredible neuro-oncological expertise, technology and research available here at ECU Health Medical Center,” said Jay Briley, president, ECU Health Medical Center. “It is immensely humbling to witness the incredible efforts that take place within the walls of the hospital every single day to further our understanding of brain tumors and brain tumor treatment. We could not be more proud of every team member who helped receive this prestigious certification.”

ECU Health Medical Center underwent a rigorous onsite review in July. During the visit, the Joint Commission reviewer evaluated compliance with related certification standards including compliances with consensus-based national standards, effective integration of evidence-based clinical practice guidelines to manage and optimize care, and organization of approach to performance measurement and performance improvement, including data collection and analysis. Joint Commission standards are developed in consultation with health care experts and providers, measurement experts and patients. The reviewers also conducted onsite observations and interviews.
“Brain tumor care certification recognizes health care organizations committed to striving for excellence and fostering continuous improvement in patient safety and quality of care,” says Ken Grubbs, DNP, MBA, RN, executive vice president of Accreditation and Certification Operations and chief nursing officer, The Joint Commission. “We commend ECU Health Medical Center for using The Joint Commission certification process to reduce variation in clinical processes and to strengthen its clinical program to drive safer, higher quality and more compassionate care for individuals served.”
ECU Health Medical Center boasts a comprehensive neuro-oncological care program, led by a board-certified neuro-oncologist. The Joint Commission’s Gold Seal of Approval® Certification for brain tumor care highlights the collaboration between interdisciplinary teams in oncology and neurosciences who are committed to advancing the treatment of brain tumors through research, numerous clinical trials, patient care, education and prevention.
“Obtaining this certification highlights our team’s unwavering dedication and commitment to delivering exceptional care for our patients with brain tumors,” said Dr. Jasmin Jo, director, neuro-oncology program, ECU Health. “Our primary objective is to ensure we deliver high-quality care consistently throughout every stage of the patient journey, from initial presentation and diagnosis to treatment, and follow-up care, as well as comprehensive education for both patients and their families. I could not be more proud of the entire brain tumor team for their remarkable dedication and hard work in achieving this certification. We remain steadfast in our pursuit of continuous improvement in the treatment and care of our patients.”
In addition to its clinical and academic expertise, ECU Health Medical Center offers an array of comprehensive brain tumor interventions, supported by state-of-the-art technology like GammaTile and Gamma Knife treatment, as well as innovative clinical trials that improve brain tumor knowledge, treatments and outcomes. This blend of cutting-edge technology and academic collaboration enhances the precision and effectiveness of care, ultimately leading to better outcomes for patients.
“Patients diagnosed with brain tumors deserve access to high-quality physicians, technology and treatment options close to home,” said Dr. Stuart Lee, executive director, ECU Health Neurosciences. “I am proud of the team behind this important certification because they are truly living our values as a mission-driven organization. With comprehensive brain tumor services available in the region, we are proud to do our part to improve the health and well-being of those we proudly serve.”
For more information about ECU Health’s neurological care services, please visit ECUHealth.org/Neuro or The Joint Commission website.
Amy Campbell, PhD, RN, CPHQ, LSSBB, quality nurse specialist III, represented ECU Health on Sept. 25 at a side event held in parallel to the 79th session of the United Nations (UN) General Assembly in New York City. The meeting, titled “2030 Global Agenda for Sepsis for Attaining Sustainable Development Goals,” was convened as a collaborative effort of the Global Sepsis Alliance (GSA), Medical Women’s International Association, Sepsis Stiftung and UNITE Parliamentarians Network for Global Health.
The meeting was the first-ever global strategy spearheaded by the GSA, with collaboration from 70 partner and member organizations from Regional Sepsis Alliances across Africa, Asia-Pacific, the Caribbean, eastern Mediterranean, Europe, Latin America and North America. The meeting’s objectives were:
- To present the 2030 Global Agenda for Sepsis as the first multi-year global strategy to alleviate the significant human, societal, economic and health care burden of Sepsis.
- To reach consensus on the urgent need for reinvigorating the Sepsis responses at global, regional and national levels for the attainment of 2030 SDGs including the aspirations for Universal Health Care, Maternal, Neonatal and Child Health, AMR, Pandemic PPR, Gender Equality, Peace and Partnerships for Development.
- To discuss the critical role of health care workers, especially the medical women, representing over 70% of the health workforce globally, in the promotion and implementation of the 2030 Global Agenda for Sepsis.
- To call for establishment of a High-Level Political Platform for Sepsis to lead integration of this global health threat into the mainstream of health and development dialogue and architecture, including G7 and G20 Summits, World Health Assemblies, UN General Assemblies, and World Economic Forums.
Dr. Campbell was personally invited to attend and speak by Dr. Mariam Jashi, MD, MPH, MPA and the CEO of the Global Sepsis Alliance, and Michael Wong, founder and executive director of the physician-patient alliance for health and safety. This invitation came as a follow-up to the 2024 World Sepsis Congress held this past April, during which Campbell served on the Scientific Committee. “I saw the invite and initially blew it off,” Dr. Campbell laughed. “I wasn’t sure it was real.” But after reassurance the invitation was legitimate, and with the encouragement of her team and Michael Wong, Dr. Campbell decided to go to New York. “I had a training session scheduled at work, but my colleagues covered for me,” she said. “I’m so thankful to my team and leaders who made it so I could attend.”
Once she arrived at the New York University campus, where the parallel session was held, Dr. Campbell said she met many leaders from across the world. “I met Dr. Eleanor Nwadinobi, the president of the Medical Women’s International Association (MWIA), Thomas Heymann, the president and CEO of the Sepsis Alliance and the Honorable Dr. Ricardo Baptista Leite, a member of the Portugese Parliament. People were speaking all these different languages and here I was from eastern North Carolina.”
The meeting focused on early detection of sepsis and how to treat patients with sepsis, no matter where they live. “As one of the speakers, I had the opportunity to emphasize the urgency of early detection, the critical need for continued research and the importance of securing funding so that everyone, regardless of their geographic location, can receive the same standard of care and chance for survival,” Dr. Campbell said. The speakers also discussed what they anticipated to be the next big problem with sepsis: antibiotic resistance.
Dr. Campbell said it was a great opportunity to represent the work she and ECU Health are doing to address the global problem of sepsis. “The attendees were impressed with the work we’re doing. ECU Health is a big deal; we have incredible people and talent, and we deserve a seat at the table,” she said. And next year, she has a seat waiting for her. “I’ve been invited back to speak next year, and I’ll work more with the GSA,” she shared. “We all have a lot to learn and do. Sepsis transcends borders, affecting individuals of all ages, races and socioeconomic backgrounds. However, the most vulnerable populations – children, the elderly and those in low-resource settings – are disproportionately impacted. Sepsis doesn’t wait, and neither can we.”
As recovery efforts continue following Hurricane Helene’s devastating impact in western North Carolina, team members from the east continue to do their part in support of those impacted.
The local efforts, led by the Eastern Healthcare Preparedness Coalition (EHPC) at ECU Health, include boots-on-the-ground contributions that started immediately after the storm hit the state and continue today in various capacities.
Chris Cieszko, Disaster Services Specialist with EHPC, was among the first group of team members to travel to western North Carolina in the Medical Ambulance Bus the day after Helene hit the western part of the state. Along with other members of EHPC, Cieszko said they helped with the immediate response which included logistical support during the staging period such as changing batteries, loading trailers and “a little bit of everything” to help manage supplies.

Using the medical bus, the team partnered with Lumberton Rescue Squad and assisted with the local EMS response from Linville-Central Rescue Squad to help evacuate 23 patients from a damaged assisted living facility in Grandfather Mountain to a safer location away from the impacted area.
“It was obviously a difficult situation given the conditions and circumstances,” Cieszko said. “No one wants to leave the comfort of their own living space. We were able to talk to them, take care of them and ultimately get them to a safe location. The entire response was a true testament to the teamwork between EHPC, Linville-Central Rescue Squad and of course our sister agencies in the North Carolina Healthcare Preparedness.”
The EHPC team also helped with technology and communication needs in the immediate aftermath of the storm, which is a vital asset to disaster response. Matthew McMahon, disaster services specialist with EHPC, helped connect a Starlink to the medical bus ensuring it had internet, and programmed helicopters to provide connectivity with ground support.
Recovery efforts have not stopped since Helene’s arrival, and neither has EHPC. Chris Starbuck, Healthcare Preparedness Coordinator with EHPC has been stationed in Raleigh at the North Carolina Department of Public Safety Emergency Operations Center. His role includes supporting health care staffing needs at all several operational sites managed by the state.
These needs, along with EHPC support, represent the importance readiness to respond to disasters immediately, while also being prepared to provide long-term help as recovery efforts continue.
“A huge outpouring of medical personnel from all over NC have volunteered to assist with the response efforts in the west,” Starbuck said. “Many are wondering ‘when’ they are going to get a chance to help. We can be ready for when the call comes. Have plans for your family, kids, and pets along with working with your employer so they can plan schedules.”
In March of 2021, Jalen Hill, MLT (ASCP)CM, joined ECU Health Beaufort Hospital as a cook in the Food and Nutrition Services department. “I wanted to go to culinary school,” he said. “But once I was at the hospital, I found out about a whole other world of opportunities.”
Those opportunities began with one conversation with Human Resources (HR). “Someone in HR heard me talk about wanting to do something different,” Jalen shared. “I wanted to be more involved and out in the field, doing patient care. I was considering going into radiology, and I thought I could train in phlebotomy and then transfer into a radiology program; but then the person in HR talked to me about the medical laboratory technician (MLT) role, which I had never even heard about. She was the one who set me up with the lab to do some job shadowing, and that was the spark.”
From there, Jalen entered the medical laboratory technician program at Beaufort County Community College in August of 2021, and at the same time, he also trained as a phlebotomist. In July 2023 he completed his phlebotomy training, and in May of 2024 he graduated with an associate degree in medical laboratory technology. That following June he began working at the hospital as an MLT.
Now Jalen truly enjoys his work and the chance to meet different people every day. “You are talking to people and hearing their stories every day. I’m drawing blood to help doctors, and I’m in the lab running tests to help get a diagnosis. That means a lot,” he said. He also values his co-workers, without whom he might not have found his true calling. “In this job, I’ve gained friendships and I’ve learned a lot. Andrea Latham and Sherry Langely were the ones who encouraged me to train as a phlebotomist and let me shadow in the lab. When I was in school, I still worked in the cafeteria, and they’d come by and ask how classes were going. They offered to help if I had any questions. I appreciated them checking up on me.”
The Washington, North Carolina native is now pursuing a bachelor’s degree in medical laboratory science at Winston-Salem State University, and he is already considering his future education and career options. “I’ve researched forensic science, but I’ve also looked into a master’s in business administration or a master’s in public health, where I could be an epidemiologist or toxicologist. It feels good to have these opportunities ahead of me,” he said.

To anyone considering making a career shift to health care, Jalen said go for it. “It’s a great decision. You have a direct influence on people’s lives every day. Every time you clock in, you are doing something that’s meaningful to someone, whether it’s a simple blood draw or talking to a nurse about lab test results. It’s a rewarding career.”
It’s not just in October, which serves as Breast Cancer Awareness Month, that you can find the ECU Health Cancer Care Outreach team making connections in the community.
Jennifer Lewis, outreach coordinator for cancer care at ECU Health Medical Center, said she spends much of her time reaching out to community partners, talking to groups in Pitt County and beyond, and connecting with ECU Health patients and families. However, she said, the most rewarding part of her job is the monthly free breast clinic she helps run.
The clinic, for women in Pitt County age 40 and older who are low income and do not have health insurance, provides screening mammograms while sharing other resources available for health care in the area with those participating in the screening.
Lewis said she is grateful to help with the program and is proud of the impact it has on Pitt County.

“Patients don’t see a bill because of donations to the Cancer Center and the ECU Health Foundation, and that’s just an amazing thing we get to offer,” Lewis said. “We start with a breast exam by a provider to check for obvious abnormalities. Then they have their 3D mammogram, so they get state of the art imaging just like anyone else would get and they don’t get lesser quality. If they have an area that is of suspicion, we can do a diagnostic mammogram and if the radiologist looks at those images and feels like there’s some more concern about something, next would be an ultrasound of that area of suspicion. The program that we have here pays for all that.”
She shared that while ECU Health Beaufort Hospital and Outer Banks Health currently have their own programs outside of Greenville and Pitt County, other hospitals across ECU Health’s system are working toward establishing the program as well.
Lewis said the partnerships and volunteerism associated with the program make it truly special. She and her team work closely with the Pitt County Health Department to help patients who need further care through the Breast and Cervical Cancer Control Program (BCCCP).
“We can’t do this without our partners, that’s for sure,” Lewis said. “We have such a great working relationship with the Pitt County Health Department and the mammography technicians, Patient Access Services, Language Access, Volunteer Services, radiology and ultrasound, and then our nurse residents who help out all work together so well. After patients are seen during the free clinic day, we have Access East on hand, too, to share information and resources about other services they can get access to. It’s such great teamwork all around that makes these events successful.”
The program sees so many patients throughout the year that they’ve recently added an extra clinic day twice a year, once in February and once in October, to help meet the needs of the community.
While Lewis is frequently in the community talking to groups and spreading awareness, October is especially important. She said she’ll spend much of the month meeting with community groups and in churches discussing risk factors, signs and symptoms and why screenings are important.
“This month is an intentional time set aside to speak about risk factors, family history, and signs and symptoms, because that’s the one time of the year that you can sit back and think, ‘OK, am I having any of these symptoms?’ Or ‘What is my family history? Because last year I didn’t have any, but this year my mother or sister has been diagnosed with it.’ It really creates that intention for people to have that moment sometime during the month,” Lewis said. “Whether it’s an ad on Facebook or hearing someone like me speak, it’s important to have that moment of reflection, remind yourself to get a mammogram and just put that in the forefront of women’s minds.”
She said if there’s one thing she could remind the community, it’s that anyone can be diagnosed with breast cancer. She noted that there are many myths, including that because someone is without family history, is otherwise healthy or is a male, that they cannot develop breast cancer. This is why she said it’s critical for everyone to be aware of signs and symptoms and receive screenings as recommended.
Resources
Breast Screening Events
ECU Health Cancer Care
More Breast Cancer Information
It was a packed house at ECU Health’s Monroe Conference Center on Oct. 1, as ECU Health and Pitt County Department of Social Services (DSS) welcomed dozens of community-based health partners for a conference designed to help tackle a complex challenge: reducing unnecessary emergency department utilization to ensure enhanced access for those needing emergency care.
It is no secret that overcrowding in emergency departments is a challenge facing hospitals across the country. ECU Health Medical Center, the only Level I Trauma Center in ECU Health’s 29 county service area, is no exception. The medical center serves a largely underserved rural region where access to care is difficult for many. That includes primary care, behavioral health care and other services best rendered in outpatient settings. Combined with a disproportionate number of uninsured community members, this lack of access to care means patients often times end up at hospital emergency departments.
Dr. Leigh Patterson, chief of services for emergency medicine at ECU Health Medical Center and chair of emergency medicine at the Brody School of Medicine at East Carolina University, said ECU Health’s nine hospitals will see nearly 250,000 visits to the emergency department this year, with more than half of those occurring at the medical center. She said conversations with key community health leaders, like the one hosted by ECU Health and Pitt County DSS, can help ensure community members are aware of, and have access to, non-emergent health care resources outside the emergency department setting.

“When I look at what happens inside the emergency department, I see the opportunity for us to help fill the care gaps that exist outside of it,” Dr. Patterson told the group, noting that she sees about 225 adult patients per day in the medical center ED, about 40% of whom could be more appropriately served in an outpatient setting. “When it comes to addressing this problem, it will take all of us as a health care community to make meaningful change. That’s why I’m heartened that so many of you have joined us today to work together toward solutions that make an impact in our community.”
The conference represented true regional community collaboration. Health care partners present at the conference included ECU Health, DSS Directors from across eastern North Carolina, Juvenile Justice, Trillium Health Services, Public School leaders, NC DHHS, payors and other eastern North Carolina hospitals and key stakeholders.

“The ECU Health/Pitt County DSS ED conference was an excellent example of cross system collaboration,” said conference co-sponsor Sharon Rochelle, director, Pitt County DSS. “This was a day to build mutually beneficial partnerships that have common goals to better serve the children and adults of the community.”
The conversation focused on both adult and pediatric/adolescent patient populations and heavily examined the challenges that behavioral health patients face accessing care. Despite the new inpatient behavioral health hospital slated to open in Greenville in 2025, those in attendance agreed that the issue needed immediate attention which involves creating increased interconnectedness among those providing care both in the community and in the hospital setting.
“We are grateful for all agencies involved in this important and challenging work,” said Jacob Parrish, vice president of capacity and throughput at ECU Health. “We know that the complex challenges we face cannot be solved at emergency departments alone. We are fortunate to have so many committed partners who share our vision for continuous improvement through strong relationships and close collaboration. Together, we can ensure the highest quality of care for communities across the East.”
The recent meeting was the first day of the two-day conference, largely centered around examining the issues through open and honest conversations. Those in attendance will reconvene later in the month for the second meeting to develop an action plan with concrete steps and strategies for improving access to care and reducing unnecessary ED utilization in eastern North Carolina.
“This is a complex set of issues, but I am confident we have the right people in our community committed to finding the solutions,” said Brian Floyd, ECU Health chief operating officer. “While these challenges are not exclusive to our health system or region, I know that together we can help support our emergency departments and improve the experience for those needing access to high-quality emergency care which is rendered at our hospitals every single day.”
Resources
The Teachers of Quality Academy (TQA) at the Brody School of Medicine at East Carolina University and ECU Health officially welcomed its 8.0 cohort, comprised of a group of multidisciplinary health care professionals committed to quality improvement, leadership development and improved patient outcomes, at its first learning session on Sept. 19.
TQA 8.0 is a professional development program for health care leaders designed to fundamentally change care delivery through a curriculum focused on building knowledge and skills in Health Systems Science which comprehensively explores how health care is delivered. Participants engage in advanced learning in quality improvement, patient safety and team leadership, develop improvement projects to apply these skills across the health system, teach others in their environment about these concepts and evaluate the outcomes of improvement interventions. Leading by example, TQA participants promote a culture of quality and safety across the enterprise.

“Our goal is to help participants take the lessons they learn in TQA back to their clinical areas,” said Dr. Jennifer Sutter, TQA physician director. “It is important that we use this opportunity to equip and empower our leaders to be quality teachers for their colleagues and teammates in order to improve patient care across the system.”
With 36 learners in TQA 8.0, participants spent their first learning session gaining invaluable knowledge about quality, the role it plays in high quality care and the impact it has on ECU Health’s mission to improve the health and well-being of eastern North Carolina. The newest cohort includes health care professionals from clinical, administrative, leadership and educational backgrounds, all of whom were selected from a highly-competitive pool of applicants. The cohort is comprised primarily of ECU Health team members but also features, for the second time, participants from outside the health system.

In one of the main team-building activities during the first learning session, groups of participants worked together to build paper airplanes. The catch? The airplanes had to be built quickly and to exact specifications. The activity helped reinforce key themes that will be instrumental to the year-long TQA experience: communication, teamwork and focus on details. The lessons are all designed to help participants create a Quality Improvement Project at the end of the program.
“Their growth throughout the program is going to be tremendous,” said Dr. Amy Campbell, quality nurse specialist at ECU Health and one of the quality coaches. “The airplane project is a great example of what they’ll experience in TQA. At first it can be overwhelming, but it helps them problem solve and then apply those lessons to their quality projects. Learning that connection between quality and patient experience can help us all provide better care and reach for better outcomes.”
ECU Health Rehabilitation will host its 13th annual Run, Walk and Roll to Independence event on Saturday, Nov. 9, bringing together former patients, their families and community members of all physical abilities. Participants can choose between a 5K or 1K course, with proceeds supporting vital rehabilitation programs. This year’s event carries special significance for Brittany Parker, who is returning not just as a participant but as a symbol of resilience after her own journey through rehabilitation.
In August 2023, Parker was navigating her first week back at work after maternity leave when she began experiencing unusual symptoms. What started as a mild tingling sensation in her fingers and toes on Monday gradually escalated. By the end of the week, Parker felt increasingly weak and fatigued, and by Friday, she could no longer lift her three-month-old baby.
Initially attributing her symptoms to exhaustion or perhaps low iron, Parker realized something was seriously wrong when she struggled to stand and walk. After falling at home, she and her family made the decision to go to the emergency room.
At the hospital, doctors quickly identified the underlying cause of her symptoms: Guillain-Barre syndrome (GBS), a rare but serious autoimmune disorder in which the body’s immune system mistakenly attacks the peripheral nerves. The condition can lead to muscle weakness, paralysis, and in severe cases, respiratory failure.
“By the time I reached the hospital, I could no longer lift my arms or legs,” Parker said.
At ECU Health Medical Center, she was diagnosed early, and treatment began right away, which helped stop the progression of the disease.

While her physical symptoms improved, Parker faced a new challenge: learning how to do everything again. After two weeks in the hospital, she was transferred to ECU Health’s rehabilitation center, where she began the long road to recovery.
“I had to relearn how to walk and even how to swallow,” said Parker.
The rehabilitation process was difficult, but Parker found strength in her care team.
“Everyone I worked with was amazing, from physical therapists to speech therapists. Melissa, my physical therapist, was so positive and encouraging. She celebrated every small victory with me, which made me want to push harder,” Parker said.
For four weeks, Parker worked tirelessly in rehab, gradually regaining the strength to walk, eat and move on her own again. Her recovery exceeded expectations, and she was able to return home earlier than anticipated.
“Being back home with my kids motivated me to recover even faster,” she said.
While doctors initially estimated her recovery could take up to a year, Parker was walking independently just three months after her diagnosis. She credits her faith, family support and the dedication of her care team for helping her through such a challenging time.
“I was so thankful to have a strong support system around me because not everyone is as fortunate,” she said. “I had such a great experience in rehab, and I want to show my support and tell everyone how amazing they are.”
Now, she’ll be able to do just that at the Run, Walk and Roll event where she will have a chance to connect with other rehab patients and share her perspectives.
“Brittany’s journey from being unable to walk to participating in the Run, Walk and Roll event is a powerful testament to her resilience and the exceptional care she received at ECU Health,” said Kasey Shue, recreational therapist, ECU Health Rehabilitation, and organizer of the Run, Walk and Roll event.
Through her participation, she hopes to inspire others and raise awareness about the importance of rehabilitation services. To learn more about the event and sign up, please visit: https://www.bikesignup.com/Race/NC/Greenville/RunWalkRoll.
Eastern North Carolinians know all too well the devastation that accompanies major hurricanes. When Hurricane Helene hit our neighbors to the west, ECU Health and Eastern Healthcare Preparedness Coalition (EHPC) team members did not hesitate to answer the call. Since Friday, these specialized team members have been providing ongoing support to hospitals and health care facilities as they work to ensure patients can be safely cared for in the fallout of the catastrophic storm.
“Our folks are great. As soon as this happened, our disaster preparedness group started putting together what we have, how can we help and how we can get there,” said ECU Health Chief Operating Officer Brian Floyd. “One of the things I love about ECU Health is we are filled with people who just care. I could not be more proud of the collective response from our team members, including those who went as part of our organizational response, and those who are helping donate to recovery efforts.”
Across western North Carolina, more than 20 hospitals were impacted by the storm and thousands of people left devastated. Some are without water and power and others are in various phases of assessment and stabilizing operations. Beyond facility issues, hazards rendered the roads dangerous and, in some cases, unable to be used at all.

Through our EHPC, ECU Health is closely aligned with NC Emergency Management for daily coordination of hospital and patient care needs. In one example, the team directly supported the evacuation of 23 residents in a care facility and help relocated the individuals to a safer location using the Medical Ambulance Bus.
Stephanie Seals, disaster services specialist with EHPC, was among the first group of team members to deploy to western North Carolina. Within 24 hours, the team “pre-deployed” to the area carrying supplies, the ambulance bus and experts to help. The ECU Health team was among the first to arrive in the region in the early hours after the storm moved through.
Shortly after she arrived on-site in western North Carolina, Seals was tasked with an important job by the state: directing the Statewide Patient Coordination Team support cell. This support cell – which is vitally important given the outages impacting connectivity at hospitals and health care facilities – brings all transfer centers together to help expedite critical care transports out of the western part of the state and to safer locations.
Many transfers from impacted hospitals to new locations have required assistance from the Statewide Patient Coordination Team support cell. This process involves assessing patient needs, working to find capacity at a new facility and helping to arrange critical care transport.
“It’s hard to overstate the importance of this work, especially during a disaster that impacts critical communication services that care teams and patients rely on,” said Seals. “It takes tremendous coordination to ensure we can get patients safely transferred to a facility that has availability to care for them. In some cases, we’re receiving phone calls from people huddled in the corner of the hospitals because that’s the only place they can get service for a few moments. From there, we take that information to help arrange the necessary transport services.”
Should patients need to be transferred as far east as ECU Health, the system stands ready to serve patients and families from western North Carolina. In the meantime, as recovery efforts continue, ECU Health and EHPC are continuing to do their part to support those impacted by the devastation of the storm in whatever way they can.
“ECU Health is deeply involved and fully aware of what’s going on and is staying connected in the work, and we need to remember this is not a short-term turnaround,” said Floyd. “This issue is going to take a long time for them to get to some form of stability. But we’re here to help and committed to doing what we can to support those impacted.”








