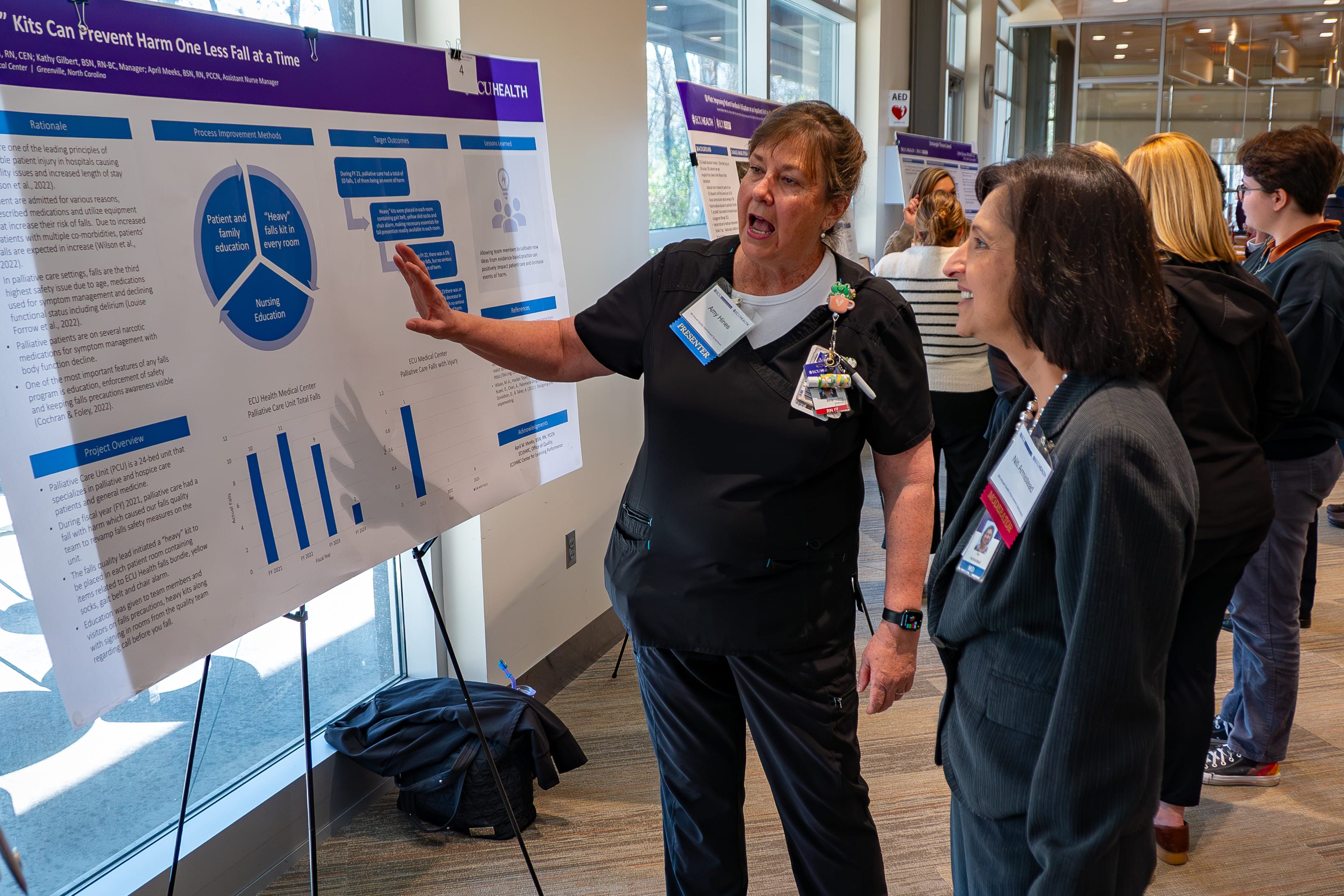
A multidisciplinary group of physicians, health professionals, care teams, residents, fellows and students came together Wednesday for the 9th annual ECU Health Quality Improvement Symposium at Eastern AHEC. With educational sessions, a keynote speaker, podium presentations and a poster session, the day was jam packed with quality improvement initiatives and ideas from across ECU Health and East Carolina University’s Health Sciences Campus.
Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine, provided opening remarks at the symposium and reflected on his personal journey in quality improvement, which began 35 years ago and continues today.
“And in that 35 years, so much has changed, but really so much hasn’t changed. The essence of collaboration and caring and love is the essence of quality,” said Dr. Waldrum.

“The fact that you all care about your environments and each other and the patients we serve is what inspired me 35 years ago. Now, with changing technologies like artificial intelligence and other impacts to the care environment, the essence of quality, caring, taking care of each other and loving each other has never been more important. Thank you for doing that and carrying that message out for our organization, working in your units every day and living our values. That is who we are at ECU Health as we create the model for rural health care and educate the future health care professionals.”
Dr. David Tillman, chair of the Department of Public Health at Campbell University, provided keynote remarks to the group of 143 in-person and 63 virtual attendees. His presentation, “Rooted in Rural: Enhancing Patient Care and Quality Improvement by Valuing the Rural Context,” focused on understanding how engagement with rural communities provides essential insights for effective and empathetic health care.
“I’m based at Campbell and get to work closely with the communities in eastern North Carolina as do so many of the attendees here, and so often the rural context is forgotten in the broader quality improvement context,” said Dr. Tillman. “Having this topic as the keynote puts ‘rural’ at the center of quality improvement efforts. You can’t just replicate quality improvement efforts in rural communities. Instead, you have to think deeply about how it applies.”
The symposium showcased more than 40 projects related to system improvement, practice redesign and other methods for improving quality within health care and here in eastern North Carolina. The projects, categorized into podium presentations, poster presentations and works-in-progress presentations, offer a snapshot of ECU Health and the Brody School of Medicine’s commitment to driving continuous quality improvement across the health enterprise.
Awards for the top podium and poster presentations were announced following the showcase.
Podium Presentation:
Outstanding Podium Presentation: Michelle Ball, MSN, RN, CCRN-K, CIC, Infection Prevention, ECU Health Medical Center – “Standardization of Skin Antisepsis for Hip Replacement Surgery
Honorable Mention Podium Presentation: Dr. Nusiebeh Redpath, Perinatal-Neonatal Medicine, ECU Health Medical Center – “Increasing Parenting Activities in the NICU by Parents with Very Preterm Neonates”
Quick shot podium presentation:
Outstanding Quick Shot Podium Presentation: Alissa Meyerhoffer, MS2, LINC Scholar, Brody School of Medicine, ECU – “Improving Patient Throughput at the ECU Health Pediatric Specialty Clinic”
Honorable Mention Quick Shot Podium Presentation: Pankti Sheth, MS4 LINC Scholar, Brody School of Medicine, ECU – “Timely Extubation in Low-Birth Weight Preterm Infants Using a Standardized Protocol”
Honorable Mention Quick Shot Podium Presentation: Dr. Greeshma Sheri, Department of Internal Medicine, Brody School of Medicine, ECU – “Improving Inpatient Sleep Quality”
Poster presentation:
First Place Poster Presentation: Mariam Tariq Awana, MD, Internal Medicine and Pediatrics, Brody School of Medicine, ECU – “Enhancing HIV PrEP Prescription Adherence through Physician Education and Assessment”
Second Place Poster Presentation: Aimee Dunn, BSN, RN, CCRN, SCRN, Neurosciences Intensive Care Unit, ECU Health Medical Center – “Targeted Interventions for CAUTI Prevention: A Success Story in Reducing Infection Rates in the NSICU”
Third Place Poster Presentation: Missy Barrow, MA, LSSGB, Internal Medicine Community, ECU Health Medical Center – “Communication Between Hospital Allied Health and Primary Care Practitioners: A Collaborative Approach to Improving Hospital Discharge Summaries”
Dr. Jennifer Sutter serves as the current physician director of the Quality Improvement Symposium, helping presenters with their projects and supporting the judges as they review each body of work. But it wasn’t long ago that she herself was standing at the podium presenting her quality improvement work. The experience, she said, can benefit health care professionals in powerful ways.
“As a presenter, it can be nerve wracking to put yourself out there, but you get so much great feedback that can help you move your project forward,” Dr. Sutter said. “From my standpoint now, it’s great to create this environment where that learning and growth can happen. It takes a team to do quality improvement, and we have people here from across the health system who are collaborating to do just that. There’s nothing better.”
The day closed with two educational sessions designed to help those in attendance take the day’s learning and apply it to their mission-driven work.
Erika Taylor, clinical faculty member and instructor in the Division of Behavioral Medicine in the Department of Family Medicine at the Brody School of Medicine, and Patricia Huerta, clinical assistant professor in the Department of Family Medicine at the Brody School of Medicine, hosted “Dialectical Behavior Therapy Skills for Medical Providers” to encourage health care providers to engage with a variety of coping skills to support their mental health and the mental health of their patients.
Randy Cobb, director of Talent Development at ECU Health, led a session called “Leading Change: Two Success Factors” where participants explored the importance of leading people through change by crafting a change plan via an interactive experience.
To learn more about the symposium and view a list of presentations, please click here.
Dr. Jonathan Hamilton, chief of urology at ECU Health, was recognized with the Patriot Award, an honor presented by the Employer Support of the Guard and Reserve (ESGR) that underscores Dr. Hamilton’s exceptional support for military personnel and their families.
This award reflects the vital role Dr. Hamilton has played in fostering a supportive environment for team members who serve in the National Guard and Reserve, as well as their loved ones. The award highlights efforts such as granting time off prior to and after deployment, accommodating flexible work arrangements, providing leaves of absence as needed and assistance to military families.
“I am truly honored to receive this award,” said Dr. Hamilton. “As someone deeply patriotic, with both of my grandfathers having served in World War II, I’ve always believed that service takes many forms.

While my path has been different, I feel it’s my duty to support those who serve our country. Dr. Hugh Mallory Reeves is not only a great friend and colleague, but also a true patriot who has made tremendous sacrifices for this nation. It’s a privilege to support him as he fulfills his duty to our country.”
Dr. Hugh Mallory Reeves, a urologist at ECU Health who also serves as a lieutenant colonel in the Army Reserves, nominated Dr. Hamilton for the Patriot Award in recognition of direct and meaningful support. Dr. Reeves, one of only a few urologists serving in the Army Reserves, has balanced his dual careers since 2003 with significant support from Dr. Hamilton and ECU Health.
“ECU Health supports veterans and appreciates their service,” said Dr. Reeves. “If it weren’t for an entity like this and people like Dr. Hamilton, we wouldn’t be able to be here with long careers as physicians and military service.”
Retired Navy Cmdr. Ken Oppenheim, a representative from the ESGR, alongside Dr. Reeves, formally presented the award to Dr. Hamilton, providing an opportunity to celebrate his impactful contributions and recognize the ways he has supported service members and their families.
“ECU Health has always been a strong advocate for serving veterans and supporting our military,” said Dr. Jason Foltz, chief medical officer at ECU Health Physicians. “Dr. Hamilton’s commitment to accommodating physicians currently serving in the military is integral to who we are.”
Anthony Bartholomew, vice president of operations for ECU Health Physicians, echoed these sentiments.
“Dr. Hamilton is a remarkable leader who supports all of his team members – military and non-military – in every way possible,” said Bartholomew. “It’s an honor and a privilege to have someone so dedicated to eastern North Carolina and our patients as part of our team.”
Dr. Hamilton’s nomination was reviewed and approved by the ESGR state committee. The North Carolina ESGR is a Department of Defense office led and operated by volunteers who aim to foster supportive work environments for members of the National Guard and Reserve.
An ordinary day in Greenville, North Carolina, became unforgettable when a health care worker and a cardiac arrest survivor were brought together by a twist of fate. Years after Vicky Greco performed CPR on Tony Parker when he collapsed from cardiac arrest during a race, the two were finally reunited and reflected on that fateful day.
In 2021, Greco and her daughter found themselves at Town Common in Greenville, a location they did not typically visit. As her daughter played on the playground, a commotion near the finish line of a local 5K race caught her attention.
“We usually go to Peppermint Park,” Greco recalled. “But for some reason, we decided to go to Town Common that day.”
As Greco’s daughter played on the playground, she noticed a commotion.

“She said, ‘I think someone needs help, Mom,’” Greco said.
That someone was Tony, who had collapsed suddenly in cardiac arrest. His wife, Delia Parker, a trained dental assistant with CPR certification, had already started chest compressions when Greco arrived.
Without hesitation, she stepped in to assist. As manager of the Pediatric Day Medical Unit at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center, Greco had experience performing CPR. Together, they worked tirelessly until emergency responders arrived.
“It was a miracle to be there, to have the training and to have the outcome we did,” Greco said. “It’s something I’ll never forget.”
A previous ECU Health News story shared Tony’s inspiring story and his recovery experience with ECU Health Heart and Vascular Care. At the time, Tony and Delia did not know who the person was that stepped in to perform chest compressions. They called the unidentified person their “angel.” After seeing the story, Greco reached out to identify herself.
Over three years later, Tony and Greco were finally able to meet under much happier circumstances. The reunion was deeply emotional, with Tony expressing heartfelt gratitude for Greco.
“Today, God revealed our angel,” said Tony. “If it weren’t for Vicky and Delia, I wouldn’t be here today. It’s amazing how everything aligned.”
For Greco, the encounter affirmed her faith in being at the right place at the right time.
“I’m thankful that God put me there that day,” she said. “The outcome was nothing short of amazing.”
Motivated by their experience, Tony and Delia Parker have since joined forces with organizations like Greenville Fire and Rescue and the Compress and Shock Foundation to promote bystander CPR training. Together, they visit local churches, community centers and underserved areas across eastern North Carolina to emphasize how simple actions can save lives.
“We teach people that you don’t need to be certified to make a difference,” Delia explained. “It’s about empowering others to act.”
The Parkers continue to share their story, inspiring communities to act in moments of crisis.
“Nearly 90 percent of out-of-hospital cardiac arrest victims do not survive,” Tony said. “Even with help, survival is only about 30 percent, but without it, it’s almost zero. Every second counts, and timely intervention can significantly increase survival rates.”
According to the American Heart Association, if performed immediately, CPR can double or triple the chance of survival from an out-of-hospital cardiac arrest.
Tony has also become an advocate for greater access to automated external defibrillators (AEDs) and the use of road identifications for athletes.
“I encourage everyone in my running and biking groups to wear one,” he said. “It can be a lifesaver.”
Following his recovery, Tony has embraced life with renewed purpose.
“Life is good,” he shared. “Even with a cardiac issue, you can still enjoy life. This experience taught me that every moment matters.”
Their story stands as a testament that heroes often emerge in unexpected moments, and that simple acts of courage and compassion can change lives forever. Their journey continues to inspire others to learn, act and save lives.
To be a health care provider is to answer a calling. For some, the journey to health care is a straight line; for others, the road is winding. This series features stories from ECU Health team members who took the winding road, but found the destination to be worth the effort.
When Deborah Rice, a staff nurse III on the palliative care unit at ECU Health Medical Center, was 13, her father died; this changed the trajectory of her adult life. “As a young girl, I knew I wanted to be a nurse,” Deborah shared. “But when my father was killed, I didn’t feel like I could put the financial burden on my mother, or leave her home alone with my younger brother, so when it was time for me to go to college, I didn’t go.”
Deborah got married and had children, and for 20 years she worked at a bank as a database analyst.
Then she learned her department was being let go, and she found herself at a crossroads. “My husband asked me if I still wanted to be a nurse, and I said yes.”
Around the same time, Deborah found herself dealing with the illness and death of several family members. “In 2008, my stepfather died from bone cancer, and from that point on for the next two to three years, we lost about five or six others in my family,” she said. “I had a hand in taking care of them when they were in their last days, and it just solidified for me that nursing was where I needed to be.”
With the support of her husband, children and mother, Deborah made the decision to pursue her dream of becoming a nurse. She first earned? her certified nursing assistant (CNA) and applied to nursing school at Edgecombe Community College, and at age 48, she graduated with her associate degree in nursing (ADN). She then went on to East Carolina University to get her bachelor of science in nursing (BSN). After graduation, Deborah knew exactly where she wanted to work. “When I was in nursing school, they were getting ready to build the Cancer Center, and I always said that was where I wanted to work.”
It took some time, but Deborah landed her dream job and now works in the palliative care unit. “It’s a special group that I work with,” she said. “It’s about helping a patient die with dignity and respect. Not everyone has a family, so we are there with those who are alone as well as those with lots of family. And we take care of the patient and their family, helping them get through this difficult time.”
The work is rewarding, but Deborah acknowledged it’s not for everyone. “It takes a special kind of person, somebody with compassion and empathy, because it’s not easy taking care of people who die and their families. But we talk with them and spend time with them, helping them accept what’s going on. You’ve got to love what you do, and our team does.” Not only do they love what they do, but the team supports each other when things get tough. “If we need to go into a room and cry, we go cry. We cry with each other, and we laugh and joke. We have to do all these things to survive.” That level of support is important to Deborah. “My team is very supportive. I wouldn’t work anywhere that didn’t have good teamwork, because that’s what gets you through the day. It encourages us to go forward and do and learn more.”
It’s equally gratifying to make connections with the patients and their families. “I tend to bond with my patients. I keep in touch with some of the family members. They’ll reach out to me from time to time to ask how I’m doing. It’s so great to build those relationships and help people through those times,” Deborah shared.
It’s clear when you talk with her that Deborah loves her work. “It’s been an experience of a lifetime, and it’s one I continue to learn and grow in. There’s never a dull moment. I love oncology and palliative or hospice care, and I keep learning and encourage everyone to keep learning. Love what you do and learn every chance you get.” She also was recently recognized as a Great 100 Nurse of North Carolina, yet another signifier that she is exactly where she should be.
To anyone thinking about starting their nursing career later in life, Deborah quickly offers reassurance. “I’m glad I did it. Even at 48 years old, I wouldn’t change a thing. I try to instill in everyone I meet that you’re never too old to go to nursing school. Even if school is challenging, I say keep going. And if you don’t succeed the first time, but it’s what you really want to do, don’t ever stop,” she said. “I hear people say they would go back to school but they’re 36 and will be 40 when they’re done. I say, you’re still going to be 40; you might as well put that time to good use.”
And Deborah has certainly put her time to good use. “Being a nurse has been the biggest blessing of my life,” she said. “My husband and my mom were my biggest fans. I wouldn’t be who I am today without my mom because she raised me from the time my father was killed. And if my dad was alive, he would be very proud of me. I did it for him as well because I knew he would want me to do it. It was not an easy thing to wait until I was 48, but it was well worth it.”
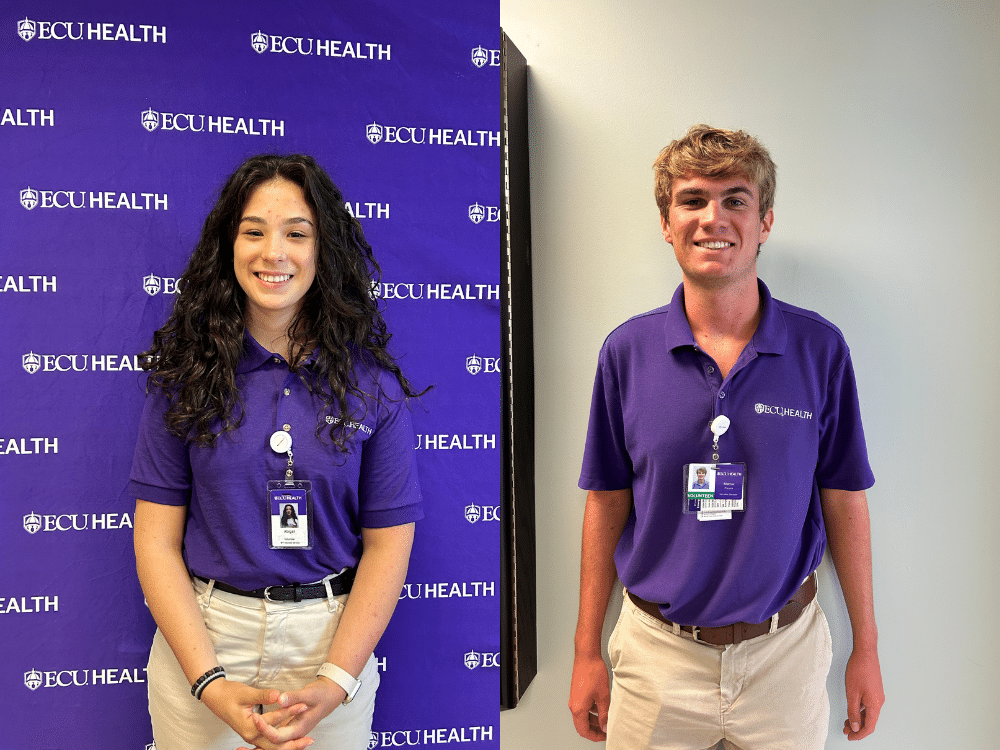
The ECU Health Volunteen Summer Program is designed to teach students ages 15 to 17 the value of community service and to provide experiences that foster growth and maturity. The program also provides an opportunity for the students to learn about and explore health care careers. Mattox Piscorik, a senior this year at D. H. Conley High School in Greenville, and Abigail Williford, a junior at the North Carolina School of Science and Mathematics in Durham, have both served as Volunteens at ECU Health Beaufort Hospital, a place where they enjoyed working in a small, family-like community.
Mattox Piscorik
For Mattox Piscorik, ECU Health is a family affair. His entire family works in health care in some way, making it natural for him to also choose a career path in the field.

“My mom’s a nurse at ECU Health, my sister-in-law is a cardiovascular sonographer, my brother is an ECU dental school student, and my other brother is in pharmaceuticals,” he laughed. “I even recruited my grandmother to be a NICU volunteer. I grew up in health care and I love it.”
His brothers also both served in the ECU Health Volunteens program, which sparked Mattox’s interest in volunteering at the hospital when he got old enough to do so. He began at the ECU Health Medical Center, but this past summer he spent time at ECU Health Beaufort Hospital. That’s where he got the idea to pursue a career as a hospital administrator. “I thought I wanted to be an emergency department (ED) doctor,” Mattox explained. “But after starting the Volunteens program and talking to Dr. [Dennis] Campbell (president of ECU Health Beaufort Hospital) this past summer, I fell in love right then and there with health care administration. I want to work at ECU Health and give back to the families in need in eastern North Carolina.”
While Mattox enjoyed his experience volunteering at the ECU Health Medical Center, which offered many opportunities to learn, he said he especially enjoyed the small community setting at Beaufort. “Everyone knows everyone, and you get to know the patients and their families. I wanted to make a strong connection and impact that community,” he said.
While at Beaufort, Mattox said he worked in the ambulatory surgery unit (ASU) taking patients to pre-op and then back to their cars after surgery. He also worked in the hospital lobby greeting patients and families and helping them find where they needed to go. “I also shadowed an ED doctor, and it was so awesome to see exactly what nurses, physician assistants, doctors and the others do in that setting,” he said.
This type of work is extremely gratifying, said Mattox, especially considering he’s seen the hospital from a patient’s family member perspective. “My dad had a couple of cardiac events and was in the hospital,” he said. “I got to see things from that side, and it showed me that these families need someone to show them compassion.”
That patient and family interaction is what Mattox enjoys the most. “You don’t know what they’re going through, and just being able to put a smile on their face and give them someone to lean on means a lot. Everyone comes together at the Medical Center and Beaufort, and it’s a team effort to provide care for eastern North Carolina. This includes the volunteers, and it means I can make an impact.”
Abigail Williford
Abigail Williford is a Chocowinity native who plans to attend medical school. She’s known for much of her life that she wanted to work in health care, in part because of her own experience as a patient at the ECU Health Medical Center. “I was born 10 weeks early and was in the NICU,” she shared. “Every year we go to Greenville and take the NICU a cake and a card to show our appreciation for them and what they do.” Her specific area of interest has evolved over time, from a neonatologist to a surgeon; but whatever she chooses, Abigail said it’s always medicine and she wants to give back.
That’s why being a Volunteen at ECU Health Beaufort Hospital made sense. “My mom heard about the program and she told me about it. I thought it sounded interesting and have been doing it for two years now.” Abigail opted to serve at Beaufort Hospital. “It’s smaller and that was better for me starting out,” she said. “Starting in a smaller community lets you get your bearings, and I plan to go back next year.”
Abigail said it’s the people that keep her coming back. “Everyone is so nice. You’re welcomed there, and everyone is willing to give you opportunities to help and learn.” Some of the services Abigail has provided include taking phone calls, delivering meals and flowers, working the front desk and signing people in, running wheelchairs to various parts of the hospital, helping in the ASU and directing people to where they need to go. “It’s cool to hear the patients and families tell their stories. I try to bring joy to their lives and it’s great to see their happy faces.” She also had the chance to observe a few surgical procedures, and some of her time volunteering in cardiac rehabilitation gave her the chance to see patients work hard to recover.
This experience has taught her that you never know what people are going through. “You might look at someone and wonder why they are so upset, but then you realize they have something serious going on. You have a choice to be a light in their day.”
Angelina Brittle, the manager of volunteer services at ECU Health Beaufort Hospital, sees the Volunteen program as a great way for teens to connect with their community while gaining valuable skills. “The Volunteen program provides a meaningful opportunity for students to experience the health care environment firsthand,” she said. “At ECU Health Beaufort, we see incredible value in offering these experiences, not only to help teens explore potential career paths, but also to foster personal growth, teamwork and a spirit of giving back. Volunteering in a health care setting allows them to connect with their community in a unique way, leaving a lasting impact on both the teens and those they serve.”
The process to apply to be a Volunteen is easy, and both Mattox and Abigail encourage any students interested in working in a hospital setting to apply. Applications for the 2025 program, which runs from mid-June to the beginning of August, open in January 2025, and students can volunteer at ECU Health Medical Center, Beaufort, Duplin or Edgecombe. Due to an increased interest in the program, applicants are encouraged to apply as soon as the application opens. To learn more about the Volunteen program and to apply online in January 2025, visit ecuhealth.org/volunteers/#Beaufort or email Angelina Brittle at [email protected].
Joshua Thomas, a lively and spirited seven-year-old, has never let his severe form of Osteogenesis Imperfecta (OI), commonly known as brittle bone disease, dampen his spirit or excitement for life.
“Joshua is full of life,” said his mother, Shakeema Thomas. “Even with everything he’s been through, he’s very active.”
Brittle bone disease is rare, impacting about 25,000 to 50,000 people in the United States, according to the National Institute of Health. The genetic disorder means Joshua’s bones are fragile and prone to frequent fractures. Over the years, Joshua has experienced a series of challenges, including approximately ten femur fractures, often from falling or seemingly harmless movements like repositioning in bed.
According to Shakeema, Joshua has broken the same femur bone about ten times. When Joshua sustained yet another displaced femur fracture, his family turned to Dr. Michael Firtha, a pediatric orthopedic surgeon at ECU Health who has treated both Joshua and his fifteen-year-old brother—who also has OI—for multiple fractures over the years.
“Displaced femur fractures in kids with osteogenesis imperfecta are difficult problems with limited options,” said Dr. Firtha. “You have to consider fixing the bone, allowing continued growth and preventing future fractures in the same area.”

In the past, Joshua’s treatment included body and leg casts, but these approaches didn’t prevent recurring injuries. Determined to find a solution that worked better for Joshua, Dr. Firtha surgically implanted a telescoping metal rod, a procedure that was first-of-its-kind at ECU Health.
This innovative implant stabilizes the fractured bone while allowing it to grow naturally. As Joshua’s femur lengthens, the rod telescopes along with it, providing long-term protection without hindering development.

“This technology is a game-changer,” Dr. Firtha said. “It lets us fix the bone, promote healing and ensure Joshua’s growth isn’t compromised. I’m fortunate to work in a health system that prioritizes patient outcomes and embraces advanced technologies.”
The results have been transformative. Since the surgery, Joshua has had a few minor falls that would have previously resulted in fractures but did not this time. For Shakeema, the change is nothing short of remarkable.
“We’re so grateful for the care Joshua has received, and Dr. Firtha is so amazing,” Shakeema shared. “He’s doing well so far, and he’s completing physical therapy now every day to get stronger.”
Joshua’s story is a testament to the importance of advanced techniques and technologies that improve the quality of life to patients with rare and challenging conditions. To learn more about ECU Health Orthopedics, please visit ECUHealth.org/ortho.
It’s been a year since the state of North Carolina passed Medicaid Expansion, bringing with it much-needed coverage and financial reprieve for the communities ECU Health serves.
North Carolina’s former governor, Roy Cooper says “One year of Medicaid expansion in North Carolina,” said Dr. Michael Waldrum, ECU Health CEO and Brody School of Medicine’s dean. “As we celebrate this moment. We’re proud to say we’re building the national model for rural health care right here in eastern North Carolina.”
That model depends on Medicaid Expansion and affordable access to care.
“It is a comprehensive health benefit where you can go see a primary care provider, have it covered,” said Kody Kinsley, secretary of the North Carolina Department of Health and Human Services. “Where you can have pharmacy, vision and dental and a copay that is never more than four dollars.”
Cost-effective health care is an important component, but it’s not the only one. ECU Health’s Dr. Karen Coward states “This is the power of Medicaid expansion. It’s not just about providing coverage, it’s about dignity.”
And peace of mind for the patients who need it most. Medicaid Expansion beneficiary and ECU Health patient, Darcy Guill spoke during the event.
“Sixteen years ago, I found myself unable to work and I lost my health insurance,” Guill said. “For the next 15 years, I was either uninsured or under insured.”
Her inconsistent coverage hit home in a different way following a car accident.
“I was hospitalized for two months right here at ECU Health,” Guill said. “I knew I was going to be uninsured again and I didn’t know what to do and I was terrified.”
That panic subsided when she realized share now had another option.
“It didn’t dawn on me at first that it was going to include me but it did,” she said. “Medicaid is literally saving my life. I am the person that benefitted from it and I am no different than all the other people that could benefit.”
Greenville, N.C. – ECU Health, the health system serving eastern North Carolina, marked a year of clinical advancements, record recruitment, expanded access to care, academic growth and national recognition in 2024. The health system’s progress demonstrates its unwavering commitment to improving health outcomes for the region’s rural communities.
“At ECU Health, 2024 was a successful year marked by groundbreaking innovations, impactful collaborations and significant achievements that solidify our position as a national model for rural health care,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University.

“From advancing academic excellence and clinical innovation to expanding access to care, these milestones reflect the unwavering dedication and hard work of our exceptional team members. As an exciting new year begins, we remain committed to building on this momentum to address the unique health care needs of our communities with a focus on meeting our mission of improving the health and well-being of eastern North Carolina.”
A few key highlights from 2024 include: celebrating the first graduating class of its Rural Family Medicine Residency Program and also expanding class sizes moving forward, investing in research with the Brody School of Medicine, introducing innovative technologies such as the BEAR® Implant, FARAPULSE™ and EluPro® BioEnvelope to enhance patient outcomes and offer state-of-the-art treatment options, and the system earning several prestigious recognitions, including becoming the only Level I Pediatric Trauma Center in eastern North Carolina and one of four in the state, Electrophysiology Lab accreditation and Magnet® designation for nursing excellence, and hosting the one year anniversary celebration of Medicaid expansion, highlighting the number of eastern North Carolinians who now have access to health insurance.
More 2024 highlights include:
- ECU Health Medical Center received The Joint Commission’s Gold Seal of Approval® for brain tumor care.
- ECU Health strengthened its network with the opening of the Outer Banks Health Cancer Center, groundbreaking for Outer Banks Health Family Medicine in Manteo, the launch of the JOY Clinic and the ECU Health and Pitt County Health Department’s vaccine and health assessment clinic for local kids.
- ECU Health achieved record recruitment of physicians and nurses committed to the ECU Health mission.
- ECU Health expanded access to primary care access by adding 198 new primary care providers and opening more than 900 new primary care appointments per week.
- ECU Health celebrated the first graduating class of its Rural Family Medicine Residency Program and expanded the class size.
- ECU Health started fellowships in Electrophysiology and American Sign Language.
- The Brody School of Medicine broke ground on its new Center for Medical Education, a step toward increasing its class size from 86 to over 120 students, addressing the growing need for physicians in the region.
- ECU and ECU Health’s NC-STeP program received a national achievement award by the American Psychiatric Association.
To explore more milestones and highlights from 2024, visit ECUHealth.org/YearInReview2024.
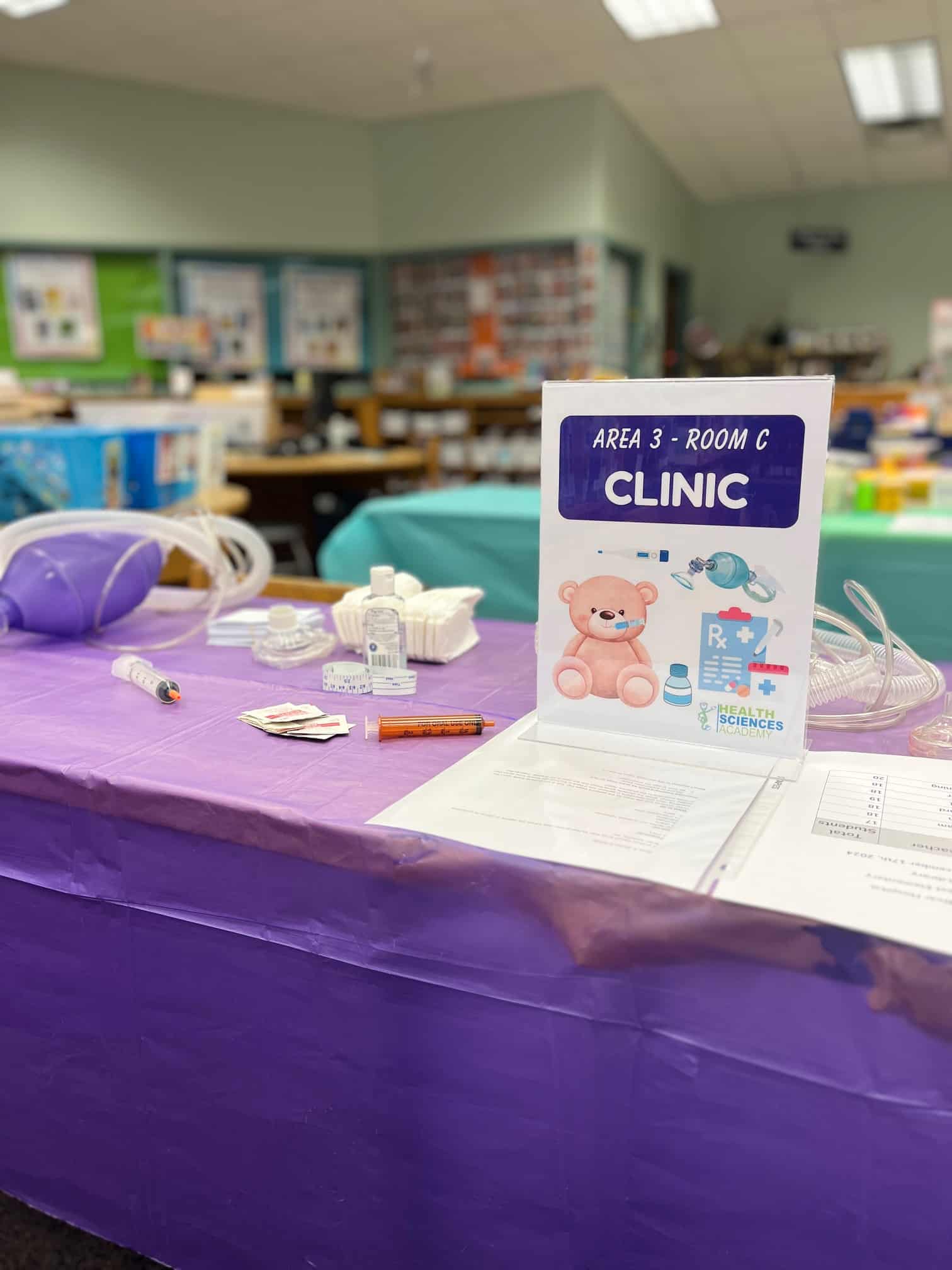
Nurses and Child Life staff from ECU Health brought the Teddy Bear Hospital to Northwest Elementary School in Pitt County on Tuesday, Dec. 17, as part of the Pitt County Health Sciences Academy. Nearly 130 kindergarten and first-grade students participated in the event, designed to introduce young children to health care professionals in a welcoming and interactive setting.
Dressed in scrubs and personal protective equipment (PPE), the students acted as caregivers for their favorite stuffed animals. They guided their “patients” through the health care process, starting with check-in and triage. ECU Health nurses examined the stuffed animals, provided a diagnosis, and directed the children to one of three stations: Sutures & Bandages, Operating Room, or Clinic. Afterward, the students and their stuffed animals visited the recovery area, where each received a certificate of bravery.
“This event offers a unique and playful way to familiarize children with health care professionals,” said Nancy Turner, workforce development consultant at ECU Health. “By engaging with the students in a hands-on setting, we’re helping to make health care less intimidating while sparking curiosity about health-related careers.”
Turner emphasized the impact of early exposure to health care.
“When kids see the process in a fun and supportive environment, it not only eases fears about doctor’s visits but also shows them that health care is approachable and full of possibilities,” said Turner.
For many students, the Teddy Bear Hospital is just the beginning of their exploration of health care. ECU Health team members, in collaboration with the Health Sciences Academy, host a variety of programs for middle and high school students, including job shadowing, career fairs and events like “Chat with a Doc.”
“The goal is to engage students at every stage of their education,” said Turner. “Starting in elementary school, we show them that health care careers are diverse and accessible. Whether their interests lie in nursing, technology, or another area, there’s a role for everyone in health care.”
These programs reflect ECU Health’s commitment to inspiring the next generation of health care professionals while building a strong, local pipeline of talent to serve eastern North Carolina.
The Pitt County Health Sciences Academy is a partnership between ECU Health, Pitt County Schools, Pitt Community College, East Carolina University, the Brody School of Medicine, Colleges of Allied Health Sciences, Engineering and Nursing at East Carolina University, School of Dental Medicine at East Carolina University, the Eastern Area Health Education Center and the Greenville-Pitt County Chamber of Commerce.
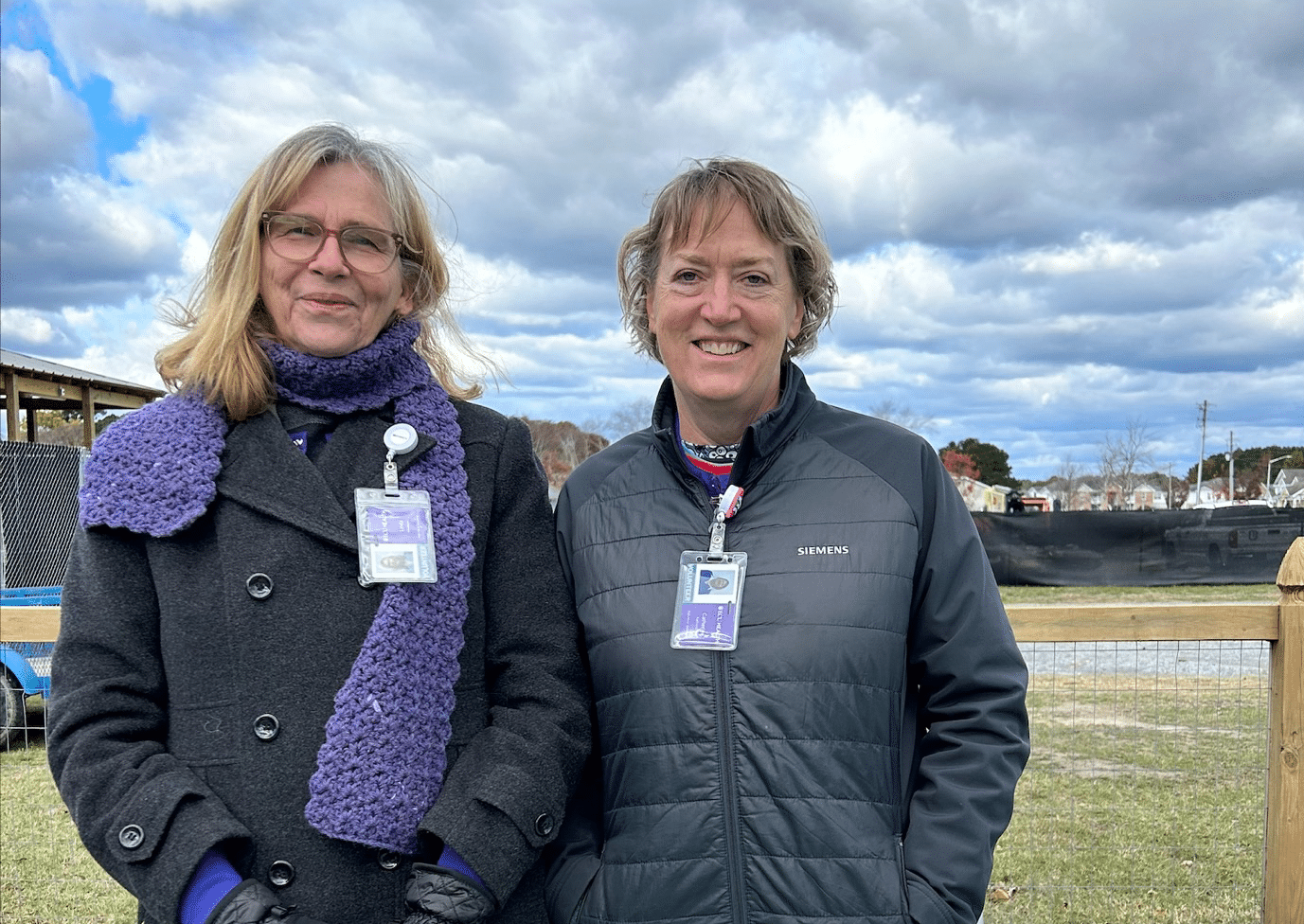
ECU Health Beaufort Hospital, a campus of ECU Health Medical Center, brought the community together to celebrate healthy living at its third annual Fall Harvest Event. Held at the Community Well-Being Zone next to the ECU Health Wellness Center in Washington, the event offered fresh produce, free health screenings and opportunities to learn about nutrition and wellness.
Attendees harvested sweet potatoes, leafy greens and fresh herbs, while enjoying the educational atmosphere. The space, designed to promote wellness and community engagement, includes 10 raised beds for vegetables, two large planters for herbs, a storage shed and areas for outdoor learning.
“This event is about more than just providing fresh vegetables,” said Dr. Tammy Thompson, ECU Health’s Director of Experience, Engagement, Education and Design. “We’re fostering wellness habits and creating a space where the community can connect, learn and thrive. Hosting this event by the Wellness Center also allows us to showcase the resources available to help community members live healthy lifestyles.”
In addition to the harvest, the event featured free health screenings on a mobile bus and tours of the ECU Health Wellness Center. Community members received guidance on growing food at home, nutrition tips and exercise information, further emphasizing the importance of holistic health. The event provided fresh vegetable soup for attendees, and warm apple cider as they toured the garden.

The event’s success was also supported by partnerships and volunteer efforts. The Conetoe Family Life Center contributed additional produce for attendees, while an East Carolina University Public Health intern welcomed guests and shared educational resources.
Volunteers like Cathy Karlovich, were thrilled to be part of the initiative.
“Healthy eating is very important to me,” Karlovich said. “I understand how eating well can impact your whole life, so doing something like this for the community and sharing valuable information is really special.”
Thompson encouraged the community to get involved, noting that volunteer opportunities are available for those interested in supporting the garden and its mission.
“My hope with events like this is to cultivate not just a garden, but a healthier, more connected community,” Thompson said.
The garden is open to community members from 9 a.m. to noon each Wednesday and Friday where any produce ready to be harvested will be distributed and other educational materials will be shared. For more information, please visit ECUHealth.org/WBZ