
Trish Baise
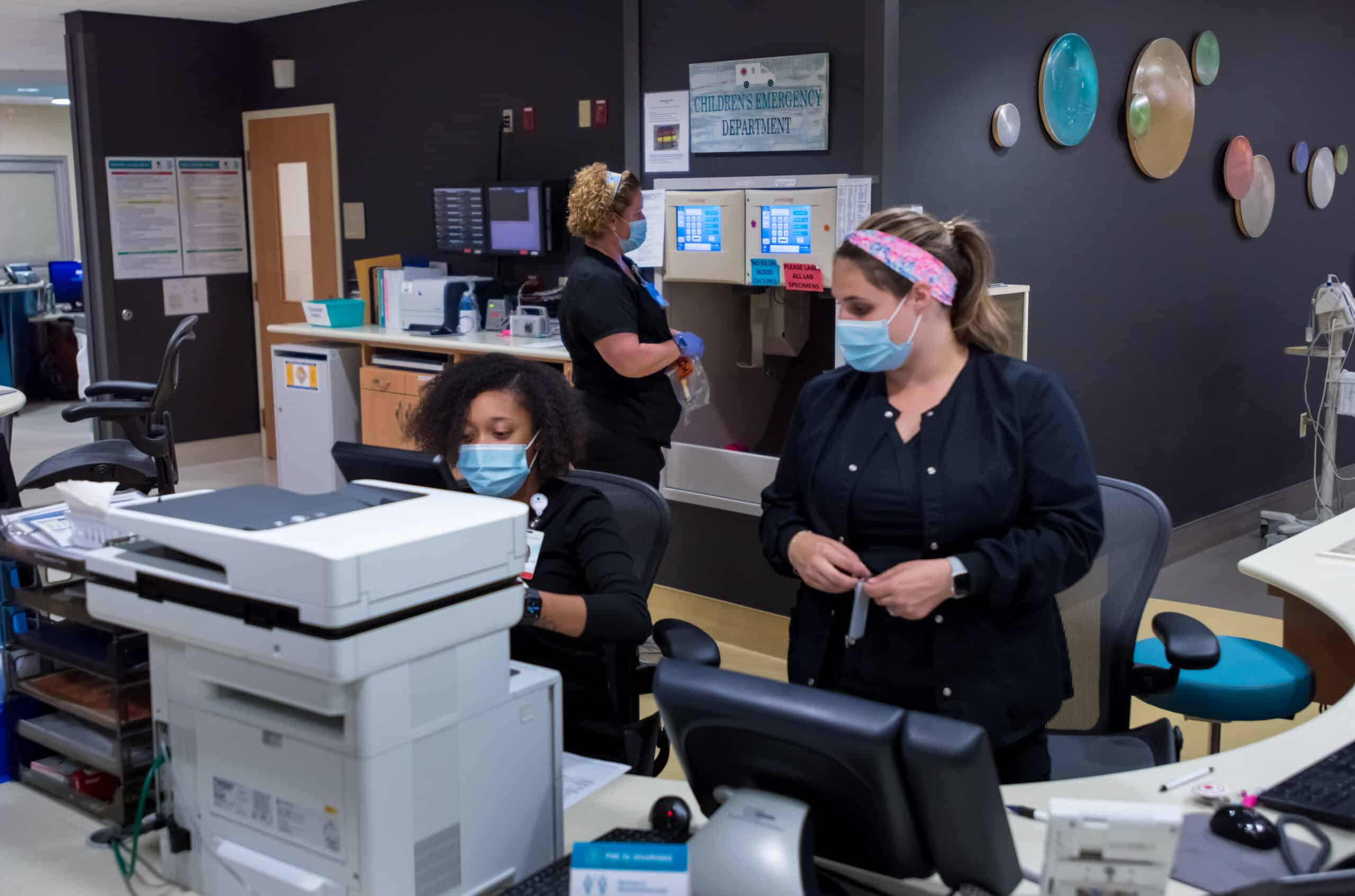
Since my arrival to the organization in January, I have enjoyed the privilege of getting to get to know the nurses of ECU Health. I’ve visited our acute care environments and interacted with a number of ambulatory care teams. In every visit, I come away inspired by the level of nursing care that is provided on a daily basis in communities across eastern North Carolina.
This week, May 6-12, is National Nurses Week, and it is my distinct honor to recognize and celebrate the incredible contributions of our ECU Health nurses. They demonstrate the mission, vision and values of ECU Health by providing excellent care in our hospitals and clinics. Nurses also serve in other critical roles across our health system focused on improving well-being, quality, safety, outcomes and access.
All nurses, regardless of their role, have a profound connection to purpose. Our purpose might be to provide hope to the hopeless, administer life-saving care that impacts generations of a family, give the support a colleague needs at just the right time, teach the next generation of nurses or be a part of innovation that fundamentally changes health care. If we pay attention, our careers our filled with daily moments of purpose, some small, some life changing. Our nurses are joined in purpose by 4.2 million nurses nationwide. It is the tie that binds us together. Together we will build upon our shared purpose as ECU Health nurses and become a national model for nursing excellence.
During National Nurses Week and beyond, I encourage our community to take the time to celebrate each and every one of the nurses providing care for our family, friends and neighbors. Nursing is the backbone of health care, and achieving the ECU Health mission would be impossible without them.
Thank you, ECU Health nurses, for your compassion, commitment to excellence and all you do for your patients and their families every day. ECU Health, our patients and our communities all benefit because you choose to serve eastern North Carolina.
“It was very nerve wracking coming here,” said Denique Barnett, a pediatric rehab nurse at the James and Connie Maynard Children’s Hospital and international nurse at ECU Health. “I’m an only child, so leaving my family in Jamaica was very hard.”
For Barnett, pursuing her passion has been a journey of more than a 1,000 miles.
“The welcome that I received was a good one,” Barnett said.
The warm reception Denique received is one ECU Health offers nurses from around the world as part of the International Nurses Program.
“My passion is pediatrics, but specifically neonatal nursing,” Barnett said. “Back home there is no degree program for neonatology. So I decided that, you know, to further my studies and to self-actualize, I would need to come to the United States.”
Not only does the program foster additional growth and training for participants, it also fills an important recruiting need for the health system.
“We bring international nurses from all over the globe to come to our organization to spend about two years in a clinical environment,” said Charlene Wilson, chief people officer of ECU Health.
Launched in November 2019, 175 nurses from 21 countries have since spent time at ECU Health.
“Even though these are nurses that are seasoned nurses, they have to go through our NCLEX,” Wilson said. “They then go through the immigration process. They then begin to understand the culture of the various hospitals that have openings for international nurses. One of the things that is very different about their practice here versus their practice in their home countries is the technology.”
“At first, you know, getting used to just how things are done here using technology for me, that was a bit of a challenge,” Barnett said.
“I’m always told by the clinicians, including the doctors, that one of the things that is fascinating about what they bring is their analytical skills, because they don’t have the technology that we have here in the United States,” Wilson said.
It’s a unique perspective put to work for a common goal, improving the health and well-being of the region these nurses now call home.
“As an international nurse, making the leap is the best decision that you will make. There is a lot of opportunities for growth,” Barnett said. “There are a lot of benefits to being here at ECU Health, you know, just make the leap, come, you won’t be disappointed.”
 Greenville, N.C. – After an extensive national search and interview process with stakeholders from across the organization, ECU Health is pleased to announce Trish Baise, DNP, RN, NEA-BC, FACHE as ECU Health’s first Chief Nursing Executive (CNE). Dr. Baise will officially join ECU Health on Jan. 1, 2023.
Greenville, N.C. – After an extensive national search and interview process with stakeholders from across the organization, ECU Health is pleased to announce Trish Baise, DNP, RN, NEA-BC, FACHE as ECU Health’s first Chief Nursing Executive (CNE). Dr. Baise will officially join ECU Health on Jan. 1, 2023.
“The impact nurses have on patients and their loved ones – from their clinical expertise to delivery of compassionate care – is at the heart of all we do,” said Brian Floyd, chief operating officer, ECU Health. “The creation of the CNE position and the appointment of Dr. Baise to lead in this role allows our organization to innovate and collaborate to further build a nursing culture that helps recruit and retain talented nurses and care givers who are dedicated to serving our region.”
The CNE will serve as a catalyst and role model to advance nursing care, education, research, care delivery models and leadership across ECU Health’s ambulatory, outpatient and inpatient areas. In her role, Dr. Baise will be responsible for integration and coordination of the nursing practice for the health system.
Throughout her more than 30 years of health care experience, Dr. Baise has led forward-focused initiatives within nursing recruitment and retention, specifically within the areas of culture and experience. She also has proven expertise in designing and deploying quality initiatives that improve quality performance and create safer care environments for patients and team members.
In addition to her vast experience in care delivery, leading care teams and strategy development, her passion for and understanding of the importance of rural health care will help advance the organization toward our vision of becoming the national academic model for rural health care.
“I am honored to have the opportunity to pioneer the Chief Nursing Executive position at ECU Health,” said Dr. Baise. “ECU Health is a recognized leader in rural health care and the organization’s mission aligns with my professional values of providing high-quality care to communities in rural environments. I am constantly inspired by the difference nurses make in the lives of those they care for, and I look forward to working alongside the great nurses that live the ECU Health mission every day.”
Dr. Baise joins ECU Health from Atrium Health Cabarrus. Prior to her role at Atrium Health Cabarrus, Dr. Baise held various system leadership roles throughout her tenure at Ballad Health System (formally Mountain States Health Alliance and Wellmont Health Systems) – a 21-hospital health system including five teaching hospitals, in rural Tennessee for 11 years.
Over the past few weeks, two events were hosted in Greenville to honor the Great 100 nurses. While the pandemic impacted the in-person celebration events for the 2020 and 2021 Great 100 nurses, these recipients were able to celebrate their accomplishments this year alongside their 2022 Great 100 colleagues!
The Great 100 nurses are selected through nominations from patients, coworkers, friends and family members. To learn more about Great 100, click here. To find out more about the 2022 nurses honored with the Great 100, check out our Newsroom.
ECU Health Great 100 Nurses of NC Brunch Celebration
On Sept. 28, ECU Health hosted a brunch celebration to honor the Great 100 Nurses recipients from 2020, 2021 and 2022. Nurses and leaders from across the system attended the event and vocally celebrated the accomplishments of the honorees including Brian Floyd, president of ECU Health Medical Center and chief operating officer of ECU Health, Jay Briley, president of ECU Health Community Hospitals and Dr. Bimbola Akintade, dean of East Carolina University’s College of Nursing.

Great 100 Gala
The 34th Annual NC Great 100 gala was held at the Greenville Convention Center on Oct. 8. The black-tie gala honored the 2022 Great 100 nurse recipients from across the state, with 22 of those nurses from the ECU Health system.
Check out some photos from both these special events.
Great 100 Brunch
Great 100 Gala
Greenville, N.C. – Since 1989, The North Carolina Great 100, Inc. has recognized and honored nurses around the state for their commitment to excellence and to promote a positive image of the nursing profession. Out of thousands of nominations that are submitted annually, 100 recipients are selected based on their outstanding professional abilities and contributions made to improving health care services to their communities.
This year, 22 ECU Health nurses have been selected to the 2022 NC Great 100. This is the largest number of ECU Health nurses to receive this recognition. This year’s honorees will be celebrated at a gala hosted by The North Carolina Great 100, Inc. in Greenville on Oct. 8.
ECU Health extends heartfelt gratitude to these nurses for their contributions to patient care and living the ECU Health mission of improving the health and well-being of eastern North Carolina.
The ECU Health nurses chosen this year are:

Alyssa Ballestero, MSN, RN-BC, APRN, is a staff nurse III in the Neuroscience Intermediate Unit and a nurse practitioner with ECU Health Neurosurgery in Greenville. Alyssa has worked at ECU Health Medical Center for seven years. Alyssa earned her bachelor’s degree in nursing from Barton College in Wilson, North Carolina and her master’s degree in nursing, family nurse practitioner from Simmons University in Boston, Massachusetts. She obtained specialty certification in medical-surgical nursing, as well as certification in emergency neurological life support and the stroke response team. Alyssa is an active member of the Sigma Theta Tau International Honor Society of Nursing.

Cathy M. Bellamy, MSN, RN LNC, is the manager of Education Services at ECU Health Edgecombe Hospital in Tarboro. She has been with the ECU Health system for more than 30 years. She started her career in Surgical Intensive Care at Duke Hospital before joining ECU Health. Cathy has varied experiences in pain management, endoscopy, surgery, orthopedics and pediatrics as a Clinical Manager. For the last 20 years, Cathy has worked in the field of Staff and Professional Development, doing what she loves in her role as a nurse educator with ECU Health Edgecombe Hospital and working on system initiatives.
Marcia Bryant, MSN, RN, NE-BC, is vice president of Clinical Operations and chief nursing officer at The Outer Banks Hospital in Nags Head. Marcia earned her bachelor’s degree in nursing from the University of North Carolina at Greensboro and her master’s degree in nursing from East Carolina University. She was appointed Chief Nursing Officer in 2015, bringing nearly 30 years of nursing experience to the role. Her leadership posts include director of cardiac services for Children’s Healthcare of Atlanta and administrative supervisor for Emory University Orthopedics and Spine Hospital. She has also held nursing leadership roles at Mission-St. Joseph Health System in Asheville, and ECU Health Medical Center in Greenville. Bryant serves on the Outer Banks Dementia Task Force and led The Outer Banks Hospital to be the first dementia-friendly hospital in the state.

Kristy Cook, PhD, RN, IBCLC, is an assistant nurse manager in the Special Care Nursery/Neonatal Intensive Care Unit at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center in Greenville. She earned a bachelor’s degree in nursing in 2009 and completed the BSN to PhD program at East Carolina University in 2019. Kristy began her career in the Newborn Nursery of Pitt County Memorial Hospital 14 years ago as a nurse extern. She has since worked in various units, such as Rehab Spinal Cord Injury, Mother/Baby, Special Care Nursery, and is currently training with the Neonatal Intensive population. She has grown with the organization, remaining at Maynard Children’s Hospital for more than eight years. Dr. Cook has served in numerous roles, including as a volunteen, nursing assistant, staff nurse, charge nurse, quality liaison, breastfeeding champion, lactation consultant and clinical coach.

Jamie Hall, BSN, RN, CIC, is an infection preventionist II at ECU Health Medical Center. She has been with the medical center for three years in infection control and prevention. Jamie earned her associate degree in nursing from Cape Fear Community College and a bachelor’s degree in nursing from the University of Mount Olive. Jamie started her nursing career as an operating room nurse and later worked as a staff nurse for a colorectal and general surgery outpatient clinic. Jamie is certified in infection prevention and control, is a DAISY Award recipient, a member of the Association for Professionals in Infection Control and Epidemiology (APIC) and serves on the North Carolina APIC Chapter Recognition Committee. Jamie is a co-chair of ECU Health’s central line-associated infections (CLABSI) sub-committee and is involved with system-wide CLABSI quality improvement projects.
Daniel Hill, MSN, APRN, FNP-BC was recently the manager of Patient Care Services—Medical Unit at ECU Health Beaufort Hospital, a campus of ECU Health Medical Center. Daniel will continue his tenure as a nurse practitioner at ECU Health Multispecialty Clinic- Belhaven beginning fall 2022. He is a board-certified Medical-Surgical Registered Nurse and a Family Nurse Practitioner. He began his medical career in the United States Army, serving multiple tours of duty in Iraq as a combat medic. After 15 years of military service, Daniel earned a bachelor’s degree in nursing from East Carolina University and a master’s degree in nursing from Simmons University in Boston, Massachusetts. He has been with ECU Health since 2019 and has served in various roles, including staff nurse, charge nurse and nursing manager.

Jamie Hoggard, MSN, RN, CCRN, is a clinical education specialist at ECU Health Roanoke-Chowan Hospital in Ahoskie. She has been with the system since 2009, starting as a nursing assistant before becoming a registered nurse, and has served in her current role for seven years. Jamie earned her bachelor’s degree from East Carolina University and her master’s degree from the University of North Carolina Wilmington. She is a certified critical care nurse, certified in Nursing Professional Development, a member of the American Association of Critical Care Nurses and a member of the Association for Nursing Professional Development.

Amanda Isbell, CNM, MSN, C-EFM, is a staff nurse with ECU Health North Hospital in Roanoke Rapids, and will continue her tenure as a nurse midwife with ECU Health Duplin Hospital in Kenansville beginning fall 2022. Amanda has been with ECU Health for 17 years, dedicated to her nursing career in maternal-newborn nursing. Amanda earned her bachelor’s degree in nursing from Chamberlain College of Nursing and her master’s degree from Frontier Nursing University with her post-graduate certificate in nurse midwifery. She is certified in nurse midwifery and fetal monitoring, and is a member of the Association of Women’s Health, Obstetric and Neonatal Nurses; the Association of Certified Nurse Midwives; Sigma Theta Tau; and Phi Theta Kappa.
Patrick M. Jones, RN-ADN, is a staff nurse III in the 3N Neurosciences Unit at ECU Health Medical Center. Patrick has been a nurse for nine years, and served at ECU Health Medical Center for five years. Patrick earned his degree from Pitt Community College in 2013 and practiced nursing in a variety of environments, including nursing homes, home health, and inpatient nursing. Patrick enjoys the positive impact nurses have in caring for patients, families and the community.

Kimberly Lodato, BSN, RN, CMSRN, is a staff IV nurse on the Medical/Surgical Unit at ECU Health North Hospital. Kimberly has been a nurse for 22 years and has worked on the same unit at the same hospital for the entire time. She graduated with an associate degree in 2000 from Halifax Community College and obtained her bachelor’s degree in nursing in 2021 from the University of North Carolina Wilmington. Kimberly is a Certified Medical Surgical Nurse and a member of the Academy of Medical Surgical Nurses.

Lawrence Madubeze, BSN, RN, is an assistant nurse manager on the Neurosciences Unit at ECU Health Medical Center. Lawrence has worked at ECU Health for 10 years and in his current role for two years. Prior to his current role, Lawrence served as a cardiac travel nurse and a staff nurse on the Neurosciences Unit. He earned an associate degree from Cape Fear Community College and earned his bachelor’s degree from Fayetteville State University.

Pamela Di Mattina, MPH, BSN, RN, is a staff nurse IV in the Palliative Care Unit at ECU Health Medical Center where she has worked for three years. Pam earned her bachelor’s degree in nursing in 2002 from Binghamton University in New York. She is a certified hospice and palliative nurse and was “the most outstanding nurse of the year” as a Vidant Brody Award recipient in 2021. She is the skin champion for her floor and is a member of the Hospice & Palliative Nurse’s Association. Pam is currently enrolled in the Adult-Gerontology Clinical Nurse Specialist master’s program at East Carolina University.

Grayson Moore, MSN, MBA, RN, is an education specialist for nursing at ECU Health Medical Center. Grayson has been with ECU Health Medical Center for 11 years and worked in nursing education for the last six years. Grayson earned her bachelor’s degree in nursing from East Carolina University, master’s degree in nursing and business administration from University of North Carolina at Greensboro, and is currently pursuing her doctorate in nursing practice at the University of North Carolina Wilmington. She is certified in Nursing Professional Development and is a member of the Association of Nursing Professional Development; the Sigma Theta Tau International Honor Society of Nursing; and Betta Gamma Sigma.

Toria Moore, BSN, RN, is an education coordinator at ECU Health Edgecombe Hospital, where she has worked for 19 years. Toria has been in her current role for more than a year and previously served as a staff nurse in the Emergency Department. She received an associate degree in nursing from Edgecombe Community College and earned a bachelor’s degree from Fayetteville State University. She is currently pursuing her master’s degree in Nurse Education at the University of North Carolina Wilmington.

Lou Montana Rhodes, MSN, RN, is the vice president for the Office of Experience at ECU Health. Lou has been with ECU Health for 20 years, served as the vice president of nursing in two regional hospitals and worked in the Office of Experience for the last five years. Lou earned her associate degree at Beaufort County Community College, her master’s degree at East Carolina University and will graduate this year with her Doctorate of Nursing Practice focused in Nursing Leadership from East Carolina University. She is a member of the North Carolina Nurses Association, the North Carolina affiliate of the American Organization of Nurse Leaders and the Watson Caring Science Institute. Lou is a member of East Carolina University’s Sigma Theta Tau, Omicron Delta Kappa, Phi Kappa Phi, Golden Key Honor Society and the Society for Collegiate Leadership and Achievement. She also serves on the Center for Family Violence Prevention Board.

Meredith Pauli, BSN, RN-BC, is a staff nurse III for the Neurosciences Unit at ECU Health Medical Center. Meredith has worked at ECU Health for seven years. She earned her bachelor’s degree from East Carolina University and is certified in medical surgical nursing.

Erin Pearson, BSN, RN, leads clinical performance improvement work throughout the ECU Health system. She is a content expert in central lines and Foley catheters, guiding organizational best practice related to infection prevention. In her role, Erin collaborates with operations, information services and infection control and is responsible for building extensively successful relationships with those partners. She manages the best practice-based auditing program for ECU Health Medical Center in Greenville. Erin is a two-time DAISY Award recipient and has participated in multiple award-winning BSI quality improvement projects. She’s a recipient of the ECU Health Board Quality Leadership Award; North Carolina Organization of Nurse Leaders, Best Practice Award; and the 6th Annual ECU Health Quality Symposium, Outstanding Podium Presentation Award.

Shannon Powell, RNC-LRN, is a staff nurse IV in Special Care Nursery/Neonatal Intensive Care Unit at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center. Shannon has been a member of the medical center team for 27 years, beginning her career at the hospital as a nurse extern in Newborn Nursery/Convalescent Nursery. Upon graduation from East Carolina University with a bachelor’s degree in nursing in 1996, Shannon transitioned to a registered nurse role. Certified in Low-Risk Neonatal Nursing, Shannon has dedicated her entire career at ECU Health to serving the neonatal population and their families.

Jessica Scheller, MSN, RNC-NIC, ACCNS-N, is a neonatal clinical nurse specialist at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center. She has been with the hospital for 17 years and began her nursing career in the Neonatal Intensive Care Unit. She has been in her current role for four years. Jessica earned her bachelor’s and master’s degrees in nursing from East Carolina University. She is a member of the National Association of Neonatal Nurses, National Association of Clinical Nurse Specialist and American Association of Critical-Care Nurses. She has a specialty certification in Neonatal Intensive Care nursing and Clinical Nurse Specialist Wellness through acute care (Neonatal).

Tara Stroud, DNP, APRN, NNP-BC, is the administrator for Patient Care Services at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center. Tara has been with ECU Health for more than 15 years. She earned a bachelor’s degree in nursing from East Carolina University and began her nursing career in the Neonatal ICU. Furthering her career, she earned a master’s degree in nursing from East Carolina University, practicing as a Neonatal Nurse Practitioner, and a doctorate of nursing practice in Executive Nursing Leadership from Baylor University. Tara maintains specialty certifications as a neonatal nurse practitioner and a nurse executive advanced. Tara is a member of the American Organization for Nursing Leadership and the North Carolina Nurses Association.
Beverly Venters, MSN, RN, CPHQ, is the director of Quality for ECU Health Bertie Hospital in Windsor and ECU Health Chowan Hospital in Edenton, and director of Nursing for ECU Health Chowan Hospital. Beverly received her associate degree in nursing at College of the Albemarle, bachelor’s degree in nursing at East Carolina University and master’s degree in nursing with an emphasis on Leadership in Healthcare Systems at Grand Canyon University. She started her nursing career in 1995 as a nursing assistant at ECU Health Chowan Hospital. She joined the Quality Department at ECU Health Chowan Hospital in 2006, and began providing leadership for the department in 2008. She is a member of the National Association for Healthcare Quality, the North Carolina Association for Healthcare Quality and serves on the Albemarle Hopeline Board. She is a certified professional in Healthcare Quality.
Rebecca Williamson, BSN, RN, CMSRN, is an assistant nurse manager for 4 North Surgery at ECU Health Medical Center. Rebecca has been with ECU Health for 13 years. She earned an associate degree in nursing from Beaufort County Community College and her bachelor’s degree in nursing from the University of North Carolina Wilmington. She is a Certified Med-Surg RN, a DAISY Award honoree, and a member of the American Association of Critical Care Nurses and North Carolina Nurses Association.
Each day at Vidant Health, incredible nurses go above and beyond to care for the patients and families of eastern North Carolina.
In February, ECU Health Medical Center (VMC) volunteer Frank Crawley had a moving experience with nurse Felicia Parker at ECU Health Cancer Care that he felt compelled to write about.
“What you don’t know is you did something to me that day,” Crawley said to Parker, as the two met again exactly a month after their interaction. “You moved me to do some things that I’ve wanted to do for a long time. That’s to write about some things having to do with this hospital and how much it has meant to me.”
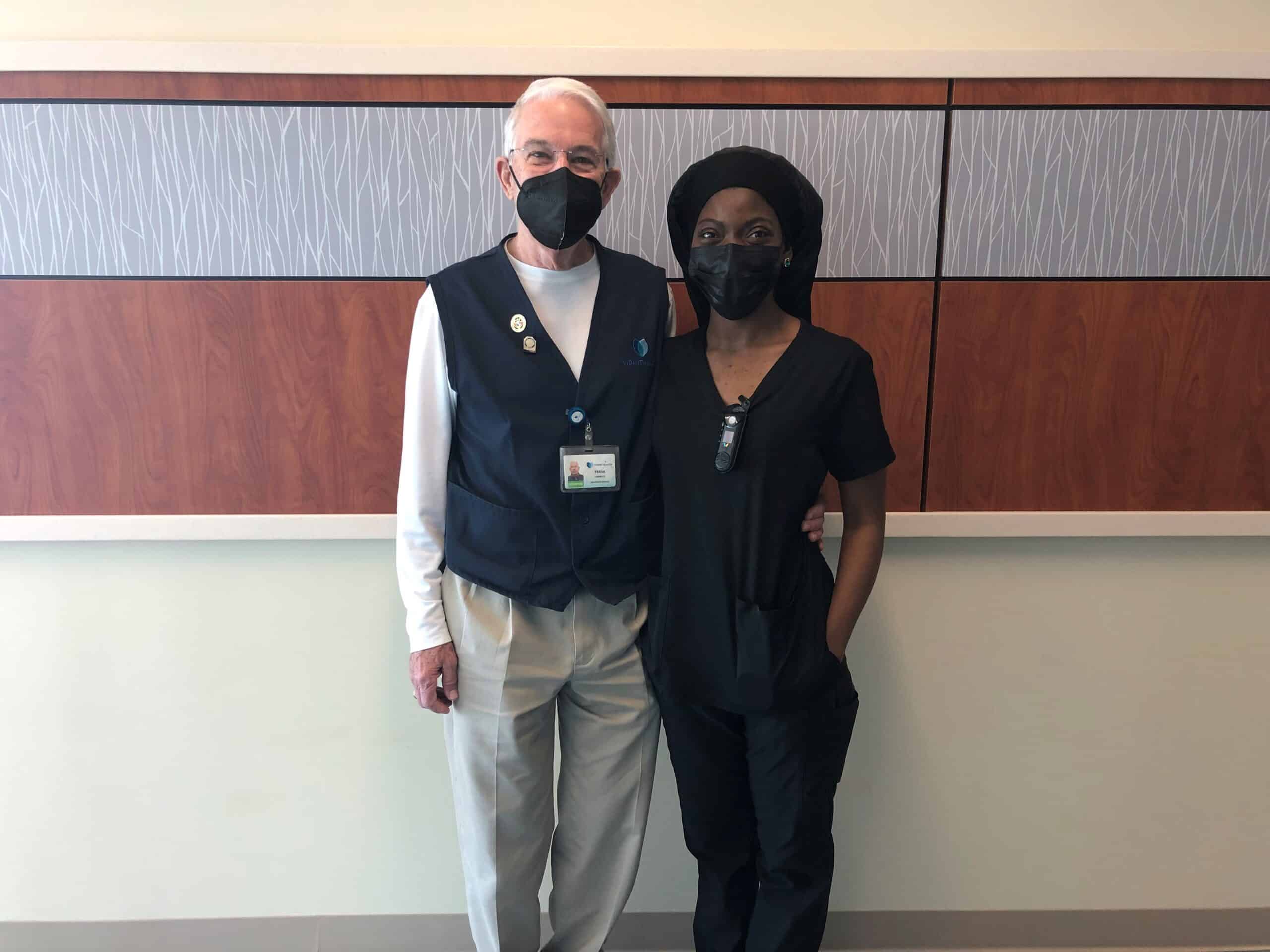
This National Health Care Volunteers week, we are proud to share the below story written by Crawley after his experience at VMC.
“On the morning of Feb. 15, 2022, a call came to Patient Escort to bring a wheelchair to the Cancer Center, room 418, to transport a patient to the Dental Clinic. I took the call. When I arrived, I knocked on the door, opened it, greeted the occupants and announced that I was there to take the patient to the Dental Clinic. Lying in the bed was a frail, elderly man. Standing by his side was his wife, who immediately said there was no way her husband was able to make the trip to the clinic in a wheelchair.
I left the room and located the nurse assigned to room 418, whom I later learned was Felicia Parker. She and I both entered the room. Ms. Parker explained to the patient’s wife that her husband desperately needed dental work. The wife seemed very concerned that her husband lacked the strength to make the trip, that his blood pressure would drop and that he could have a seizure, particularly if taken in a wheelchair. She said that he might be able to make the trip in his bed. The soft-spoken Ms. Parker explained that the bed was too large to transport into the clinic. Additionally, she said that to alleviate the wife’s concerns, she would accompany her husband to the clinic, assuring her that every precaution would be taken. First, she explained that we would exchange the Staxi for a Stryker wheelchair, carry an oxygen tank with us, along with a blood pressure/heart rate attachment to monitor her husband’s vital signs.
The wife began to weep quietly. She walked into the bathroom and continued to sob, fearing for the welfare of her husband. Ms. Parker followed her to the bathroom. She spoke softly, lovingly to the patient’s wife, hugged, consoled and reassured her that we would take every precaution to see that her husband made the trip to the clinic without incident. Still hugging, Ms. Parker told the patient’s wife that she would call her once we reached the clinic. I was so impressed at that moment with the love, patience, caring and empathy Ms. Parker showed her — far beyond what I had expected to witness that day. With the wife comforted and reassured, Ms. Parker and I located a Stryker chair, added an oxygen tank and a vitals’ monitor. Next, Ms. Parker said that she was raising the bed to a sitting position so that the patient could sit upright for a few minutes and adjust to the change in position. Doing so, she explained, we would be able to see whether his blood pressure and heart rate would respond favorably to the positional change. Next, Ms. Parker and I moved the Stryker chair next to the bed and slowly moved the gentleman’s feet off the side of the bed. All went well — at first.
Within seconds of moving his feet off the bed, there was a sudden drop in the patient’s blood pressure and a change in heart rate. Carefully but quickly, Ms. Parker moved the patient’s feet back onto the bed and slowly lowered the bed. She immediately left the room and called for backup help — not calling for a “code blue” but the next level below, as I heard her say. Within a few minutes, the room was filled with attending physicians, nurses and aides. I quickly moved back, stepping out of the room to allow Ms. Parker and the medical staff space to work. Within what seemed like only a few minutes, the patient’s vital signs were restored to normal, and the room was calm again. Ms. Parker then turned to the patient’s wife, hugged and comforted her.
With the room restored to calm and the father’s vitals stable, Ms. Parker came to me and thanked me for my help.
“No,” I said. “Thank you for allowing me the privilege to witness, firsthand, nursing at its very best.”
Not only was Ms. Parker highly competent, as evidenced by the technical skills she displayed, she also possessed that rare ability to sincerely comfort, console and empathetically connect with the very distressed patient’s wife. Empathy is near impossible to teach. Neither can it be faked. Deeply moved and with tears in my eyes, I hugged Ms. Parker.
“Never had I expected to report to volunteer duty Tuesday morning and see the loving, compassionate face of Jesus on display,” I said.
That day was most rare and wonderful, and I knew it.
After writing down his experience, Crawley shared this with the volunteer team and eventually it found its way to Parker. When she received the email, she had her daughter read the story to her sons. Parker said she was moved by him sharing his experience with her and her family.
“It’s nothing that I gave a second thought to – it’s just what we do every day,” Parker said, who will celebrate three years in the system in June. “Sometimes we kind of don’t look at what we do, how it impacts others. Especially, we feel like it’s just something that we’re just supposed to do. You’re supposed to get up, you’re supposed to greet people when we see them. We don’t think anything of it. That’s what it was for me. It was just, ‘Hey, what you do does matter.’”
Crawley said he has been volunteering at the medical center for nine years. Previously, he was an education professor at East Carolina University.
“In the busyness of life, and I think it has a lot to do with my age, I look for those moments that I can connect with people or when I can see them connecting, because I believe that’s what we were born to do,” Crawley said.
“We do a lot of things for which we get paid and it’s difficult to find something in you down deep that in that busyness,” Crawley said. Then looking at Parker, he continued, “I know you had lots of other patients, but in that busyness to console the woman who wasn’t your patient. You saw something there that was a greater need and you met that need. That was just powerful.”
We are so proud to have experiences like this unfold along the halls of Vidant hospitals each day. Thank you to the care teams, volunteers and team members who serve eastern North Carolina. If you are interested in joining the Vidant team, visit our Careers site.
Two Vidant leaders were recognized on Friday, March 18 and inducted into the East Carolina University (ECU) College of Nursing Hall of Fame along with seven other recipients.
Dr. Julie Kennedy Oehlert, chief experience officer at Vidant Health, and Dr. Kamilah Williams, administrator for nursing professional practice, development and clinical education at ECU Health Medical Center (VMC), were each honored last week after being nominated by colleagues and accepted into the ECU College of Nursing Hall of Fame.
Dr. Williams is a 2005 graduate of the ECU College of Nursing and an eastern North Carolina native. She said she is proud to serve the community she calls home and the induction was a great honor.

“I’m so humbled and proud to be a Pirate nurse,” Dr. Williams said. “I’m proud to give back to my community here in eastern North Carolina, where I grew up as a young child. It’s an honor to serve and care for the population that I grew up with. I’m just grateful.”
Dr. Williams is tasked with developing nurses in her role at Vidant. Under her leadership, VMC achieved accreditation for the Nurse Residency Program and has developed an International Nurse Fellowship Program.
She said she loves what she does and is happy to give back to her profession and region through her role.
“When I think about the mission of our organization and being able to improve the health of the people here in eastern North Carolina, it’s exactly why I do what I do,” Dr. Williams said. “As a young child, I always knew I wanted to be a nurse and be able to give back to my community. Now in my role, to be able to help develop future nurses, it’s just a humbling experience.”
Dr. Julie Oehlert has used her experience as a nurse to improve the experience of patients, families and Vidant team members across eastern North Carolina. Dr. Oehlert came to Vidant and eastern North Carolina in 2016 and said the recognition made her feel at home.
“For me, I was so humbled and excited to be recognized with other Pirate Nurses,” Dr. Oehlert said. “I came from outside of Vidant but my heart is with Vidant and ECU. I feel welcomed into this community. I was so overwhelmed when I was nominated and accepted.”
Dr. Oehlert said she is proud to be part of a health system with so many Registered Nurses as leaders in different areas. With nurses in non-traditional roles lending their health care expertise and compassion for patients and families, the nursing heart can be seen in many facets of the health system.
“I don’t get to work directly with nursing but the nursing heart of all the leaders that have RNs behind their name, is pretty darn special at Vidant,” Dr. Oehlert said. “Many of our presidents and executives have that RN heart and that means we are always caring about our communities, we always have a holistic view on care and I love that.”
With the nine inductees for 2022, the ECU College of Nursing Hall of Fame that started in 2011 has grown to 150 members.
One of the past inductees on hand for the event was Dr. Daphne Brewington, senior vice president nurse executive at ECU Health Medical Center.
“It’s just been an amazing night and both Dr. Williams and Dr. Oehlert are so deserving of this award,” Dr. Brewington said. “I’m so proud that they have been inducted into the ECU College of Nursing Hall of Fame. I was inducted in 2018 so it’s just really special and surreal to be able to support colleagues that are on this journey as well.”
Inductees into the Hall of Fame also help fund a scholarship for ECU College of Nursing students, which has raised $170,000 throughout the years to support the next generation of nurses.
Learn more about the ECU College of Nursing Hall of Fame on ECU’s website.
Work culture makes a difference in recruitment, retention and team well-being, and all health care organizations strive to offer a more loving work environment where team members can thrive.
Vidant Health Chief Experience Officer Dr. Julie Oehlert joined the SEE YOU NOW podcast, from Johnson & Johnson and American Nurses Association, and discussed leading organizational change on Episode 64: Reporting Powers: Leading With Love.
A new, loving culture
Dr. Oehlert said “power-over” or hierarchical relationships are at the core of many relational issues, and missed opportunities in health care. She encourages all of health care to work together with team members on culture innovations.
“I think most organizations use the definition of culture of ‘How we do things around here,’” Dr. Oehlert said. “That cultural definition is like you’re a fish swimming in a bowl. It is not actionable. We believe that culture is defined by how our relationships are structured with each other – how we treat each other, how we treat patients, how we treat our community, and that definition is very actionable and everyone can impact the culture.”
As team members partner to create a new, loving environment, team and organizational goals become much more achievable. Dr. Oehlert said measures such as whether team members are afraid of reporting safety events, if they feel heard by their manager, and if the community believes the health system is their partner, are key indicators of a positive, changing culture.
Dr. Oehlert noted the importance of looking to an organization’s own team members to change cultures and innovate in their own space. She believes that health care can improve if they listen to their team members who want to have a voice in their own work environment.
“You don’t need other people to help you with your culture. Do you know you have innovators sitting around in your hospital? They’re everywhere,” Dr. Oehlert said. “Your EVS and food services workers will redesign your food delivery in a hot minute. Don’t bother to pay a consultant. Your innovation awaits you if you walk into your departments. Give them an environment and ask them, listen to them and they will design beautiful things.”
It starts at the top
A culture shift in health care must include changes to leadership development. Transformational leadership is full of love, kindness and mentorship.
So, she and the Organizational Development department felt they needed to carve its own path.
“I called our chief operating officer and I had all of these books sitting around me, you know your scholarly books on leadership development,” Dr. Oehlert said. “So I’m looking at all these different models and I’m putting my head in my hands and I’m like, ‘None of these are going to take us where we want to go. We’re going to have to develop our own leadership curriculum and our own leadership framework.’”
A team came together and different and new frameworks were pulled together to create a unique system for Vidant to develop talented team members and grow leaders.
This new system was necessary to transform and later maintain a culture of love, empathy and power-with attitudes from organizational leaders.
“Leadership development is so important because the leaders are at the top of the hierarchy; if they are perpetuating fear or dominance, whether intentional or not, because some leaders were just taught to lead that way, that has to shift,” Dr. Oehlert said. “A new leadership way of being has to emerge.”
Policies reflect culture
Policies are a reflection of the workplace culture and policies can frequently be outdated and not in line with the culture of the organization.
Dr. Oehlert said as the culture shifted, the organization needed to review policies and procedures.
“It’s amazing how many policies, once you read them with a lens of caring and love that you realize – ‘This is terrible. Why would we have this policy?’” Dr. Oehlert said. “Are your policies by their nature punitive? How do you handle mistakes and coaching and errors with your team members? Do you have grace when they are humanly failing? Do you have grace for their mental health issues? You really have to dismantle that.”
Looking for more?
Find and listen to the SEE YOU NOW podcast, Episode 64. Reporting Powers: Leading with Love, wherever you get your podcasts.
Read more on Dr. Oehlert’s previous appearance on the SEE YOU NOW podcast.
Vidant Chief Experience Officer Julie Oehlert talks about nursing innovations on SEE YOU NOW podcast
Vidant Health Chief Experience Officer Dr. Julie Oehlert took time recently to discuss the Vidant system, nursing and innovation on the podcast series SEE YOU NOW.
Johnson & Johnson and the American Nurses Association launched SEE YOU NOW, a storytelling podcast that highlights innovative and human-centered solutions driven by nurses. The podcast addresses today’s most challenging health care problems.
Changing a culture
During her time on the podcast, Dr. Oehlert reflected on the importance of a positive culture in health care and how a strong culture can lead to improved patient and team member experience. When she first arrived at Vidant, she noticed the organization’s culture had room for improvement—including a shift from a “power-over” to a “power-with.” Dr. Oehlert said she focused most of the work in her first two or three years in the system on team members, love, empathy and bringing those elements into relationships so that a new, loving culture could emerge.

“It’s very clear in the science that one type of culture begets certain things and another type of culture doesn’t,” Dr. Oehlert said. “So in a power-with culture, you get a lot of innovation, empathy and compassion. You usually have good mentorship, good talent management, you have shared decision making, great patient experiences, good quality outcomes and people aren’t afraid to report near misses. That culture will deliver results that everyone in health care wants.”
As this desired culture became a reality at Vidant, it built a foundation for resilience in the eight-hospital health system and the more than 13,000 team members. Resilience is necessary at all times in health care to face the various daily challenges, especially in rural health care. But as a pandemic closed in, its importance was magnified.
Delivering health care in rural areas
Dr. Oehlert said delivering health care in rural areas is a challenge Vidant faces every day. The communities Vidant serves face many of the same problems other rural health systems see, along with its own unique challenges.
“People can’t get places, people don’t have access to things that they need or want. Anywhere where there are rural environments, in those kind of forgotten places anywhere in the world, these challenges would be the same,” Dr. Oehlert said. “When you’re in an urban environment, you’re 10 minutes from a resource. Here, you could be an hour and a half from a resource. That brings with it a lot of really interesting possible solutions.”
One of those solutions for Vidant is keeping resources out in the communities that need them. With regional hospital and clinic locations, she said Vidant can keep care and resources as close to home as possible for patients and families throughout a 29-county service area.
Adapting in a crisis
 The COVID-19 pandemic has made the need for care and resources close to home much more important. Dr. Oehlert said a key innovation since the onset of the pandemic has been clinic pop-ups throughout eastern North Carolina.
The COVID-19 pandemic has made the need for care and resources close to home much more important. Dr. Oehlert said a key innovation since the onset of the pandemic has been clinic pop-ups throughout eastern North Carolina.
These community health events bring crucial services, screenings and resources to areas that need them. Talent recruitment is another important service provided during these community events.
“We always bring a recruitment person. So we actually give people jobs, which is what our communities’ want, so we hire right out of these community events,” Dr. Oehlert said. “Then as soon as our entry-level workers get here, we say, ‘What else would you like to be? What else would you dream of doing?’ We do a lot of really relational recruitment right from our low-trust communities.”
Giving team members the room and resources to grow through various programs, like the HomeGrown program, is one way Vidant makes an effort to invest in its team members.
Innovating together
COVID-19 has changed the typical way of doing business across all industries, and health care is no different. Innovation often is born during crisis and desperation and Dr. Oehlert said that while health care is changing and innovating rapidly, advice from a mentor gives her comfort.
“Teddie Potter used to say very kindly to me when things were very chaotic, ‘Julie, sometimes things have to disassemble before they reassemble.’ That gives me some peace because health care is disassembling, but it’s only disassembling so we can reassemble it in a much better, more loving, more caring way that is exactly where we need to head for health care to be what we need it to be for our future,” Dr. Oehlert said.
Dr. Oehlert said while health care moves forward, it will be crucial to keep nurses involved in discussions around innovation because of their unique perspective and connection to the patients they serve.
“They can do it with love and empathy and joy and hope as well as having the technical and scientific expertise,” Dr. Oehlert said. “That’s the beauty of nursing, it’s a heart job but it’s a science job.”
Looking for more?
Find and listen to the SEE YOU NOW podcast, Episode 61. Reporting Powers: Insights in Action wherever you get your podcasts.
Greenville, N.C. – Sept. 28, 2021 – Since 1989, The North Carolina Great 100, Inc. has recognized and honored nurses around the state for their commitment to excellence and to promote a positive image of the nursing profession. Out of thousands of nominations that are submitted annually, 100 recipients are selected based on their outstanding professional abilities and contributions made to improving health care services to their communities.
This year, 14 ECU Health Medical Center (VMC) nurses have been selected to the 2021 NC Great 100.
Vidant Health extends heartfelt gratitude to these nurses for their contributions to patient care and living the Vidant mission of improving the health and well-being of eastern North Carolina.
The Vidant nurses chosen this year are:
Anthony Ayscue, BSN, RN, CRN, is the assistant nurse manager for ARU, VAT and Radiology Nursing at VMC. Anthony has been with Vidant for more than 18 years and has been in his current role for more than five years. Anthony is a certified radiology nurse, and earned an associate’s degree from Edgecombe Community College and a bachelor’s degree from Barton College. He is a member of the Association for Radiologic & Imaging Nursing.

Youssef Belahchich, RN, is a staff nurse III working in the Neurosciences Unit at VMC. Youssef has worked at Vidant for seven years and previously served as an orthopedic RN. He graduated from Pitt Community College with an associate degree in nursing and worked in a skilled nursing facility before joining VMC.

Amy Campbell, PhD, RN, CPHQ, LSBB, is a quality nurse specialist III on the Performance Improvement Quality Analytics team at VMC. Amy started her career as a staff nurse on the pediatric floor at the former Pitt Memorial Hospital in 2000. Amy has been in her current role for 12 years. Amy earned an associate degree in nursing from Pitt Community College, bachelor’s degree in science nursing from East Carolina University (ECU), as well as a master’s degree and PhD in nursing from ECU. She is certified in Lean Six Sigma Black Belt from North Carolina State University and is a certified professional in Health Care Quality. Amy was an East Carolina Hall of Fame doctoral scholar and the 2018 Association for Leadership Science in Nursing Doctoral Grant recipient. Amy is a member of National Association of Healthcare Quality, Association of Leadership Science and Sigma Theta Thau.
Michelle Carawon, MSN, RN, CCRN-K, is an infection control preventionist III at VMC. Michelle has been with Vidant for 16 years and has been in her current role for the past year. Michelle is certified in critical care nursing and earned a bachelor’s degree in nursing from East Carolina University and a master’s degree in nursing from Walden University. Michelle is a member of the American Association of Critical Care Nurses, Sigma Theta Tau-International Honor Society of Nursing, the Association for Professionals in Infection Control and the East Carolina University Alumni Association.

Miriam Coggins, BSN, RNC, is a staff nurse at VMC’s Neonatal Intensive Care Unit (NICU). Miriam has worked in the NICU at VMC for 36 years. She earned a bachelor’s degree in science nursing from East Carolina University. Miriam has held multiple roles at VMC including permanent charge nurse, assistant nurse manager and interim manager. As interim manager she assisted with the opening of VMC’s current 50 bed NICU. Miriam has a certification in neonatal intensive care and serves as co-chair of the Central Line Team.

Roland Ennis, RN, is an assistant nurse manager of the Orthopedic Unit at VMC. Roland has been with Vidant for 21 years and has served in his current role as assistant nurse manger for 10 years. He earned an associate’s degree in nursing from Edgecombe Community College.

Amanda Helms, BSN, RN, is a staff nurse III in the Trauma Surgery Intermediate Unit at VMC. She has been at Vidant for 15 years and has served in her current role for nine years. Amanda earned an associate’s degree in nursing at Beaufort County Community College and received a bachelor’s degree in nursing from University of North Carolina at Wilmington. Amanda obtained trauma nursing core course certification and is a member of the American Nurses Association, North Carolina Nurses Association, Society of Trauma Nurses and Sigma Theta Tau International Honor Society of Nursing.

Kristie Hertel, MSN, RN, CCRN, ACNP-BC, FCCM, is an advance practice provider with the Trauma and Surgical Critical Care Department at VMC. Kristie started at VMC in 2006. Kristie earned a bachelor’s degree from Nazareth College, a master’s degree from Rush University and is currently enrolled at UNC Wilmington working toward a doctorate in nursing practice. She has received specialty certification as a certified critical care nurse and acute care nurse practitioner along with induction as a fellow in the Academy of Critical Care Medicine. Kristie is a member a member of the American Association of Critical Care Nurses, Society of Critical Care Medicine and Sigma Theta Tau International.

Stephanie Head, MSN, RN, PMGT-BC, NE-BC, is the nurse manager of the Vidant Pain Management Center, a hospital outpatient department of VMC. A Vidant nurse for 30 years, Stephanie has been the manager at the Vidant Pain Center for the past nine years. Prior to her current role, Stephanie served as a nursing assistant for two years. Stephanie earned a bachelor’s degree and master’s degree in nursing leadership from East Carolina University. She holds a specialty certification in pain management nursing and is a nurse executive-BC. Stephanie is an active member with American Society of Pain Management Nurses and North Carolina Organization of Nurse Leaders.
Patty Jordan, MSN, RN, NE-BC, CCCC, is a senior nurse administrator in Patient Care Services at VMC. Patty has been with Vidant for five years. She earned a bachelor’s of science degree in nursing and a master’s of science degree in nursing and health care administration from Southern Illinois University – Edwardsville. Patty has obtained specialty certifications as a nurse executive, and as a cardiovascular care coordinator. Patty is a member of American Association of Critical Care Nurses, East Carolina Chapter of American Association of Critical Care Nurses, American Organization of Nurse Leaders, Sigma Theta Tau, and the North Carolina Nurses Association.

April Meeks, BSN, RN, PCCN, is the assistant nurse manager on the Palliative Care Unit at VMC. April has been with Vidant for 15 years and in her current role for more than a year. She earned an associate degree in nursing from Edgecombe Community College and a bachelor’s degree in nursing from the University of North Carolina at Wilmington. April is specialty certified as a progressive care certified nurse. April is a Daisy Award Honoree and a Vidant Brody Award Finalist. April is a member of the American Association of Critical Care Nurses, North Carolina Organization of Nurse Leaders, North Carolina Association of Healthcare Quality and Sigma Theta Tau.

Shannon Mazza Roberson, BSN, RN, CPEN, SANE-P, is a staff nurse IV in the Special Care Nursery at Maynard Children’s Hospital. Shannon has been with VMC for the past eight years and she earned a bachelor’s degree from Barton College. She began her career with Vidant in the Children’s Emergency Department as a staff nurse. Shannon has been a part of the leadership team within Emergency Services as both assistant nurse manager of the Children’s ED and nurse manager of the Adult ED. Shannon has more than 23 years of nursing experience and has cared for pediatric patients throughout her career. She is a certified pediatric emergency nurse as well a sexual assault nurse examiner for pediatrics. She is a 2020 finalist for the Vidant Brody Award as well as a Daisy and Team Daisy Award recipient. Shannon holds multiple certifications in the field of Emergency Services. Shannon is a member of the International Association of Forensic Nurses, the Emergency Nurses Association and a member of Sigma Theta Tau.

Sherry Stone, DNP, RN, NPD-BC, is an education specialist in nursing at VMC. Sherry has been at Vidant for six years. She earned an associate degree from Patrick Henry Community College, a bachelor’s degree from Old Dominion University, a master’s degree from Western Governor’s University and a doctorate in educational leadership from American Sentinel University. Sherry has obtained certification in nursing professional development. She is a member of the American Nurses Association, the North Carolina Nurses Association, the National League for Nursing and The Association for Nursing Professional Development for which she serves as the chair for the Recognition Committee.

Ashley Venters, MSN, RNC-LRN, is a staff nurse III in Special Care Nursery at VMC. Ashley has been in her role for more than 14 years and earned a bachelor’s degree and master’s degree in nursing education at East Carolina University. Ashley is currently working towards post-master’s work in the field of family nurse practitioner. Ashley obtained her specialty certification in low-risk neonatal nursing and is a member of Beta Nu and Sigma Theta Tau.















