ECU Health is advancing pediatric surgical care in eastern North Carolina by introducing robotic-assisted surgery, a cutting-edge approach that enhances precision, improves outcomes and expands minimally invasive options for children in the region.
Dr. Courtney Harris, a pediatric surgeon at ECU Health, recently performed the health system’s first pediatric robotic-assisted cholecystectomy (gallbladder removal).
“Robotic surgery is still relatively new in pediatric care, and it offers significant advantages for both surgeons and patients,” said Dr. Harris. “The enhanced range of motion, improved precision and advanced imaging technology allow for a more refined approach, leading to better outcomes.”
Robotic-assisted procedures enhance precision with robotic arms that offer wrist-like movement. This technology provides greater dexterity, similar to open surgery, while preserving the benefits of a minimally invasive approach.

With extensive experience in robotic procedures, Dr. Harris has collaborated closely with Dr. Shannon Longshore, the division chief of pediatric surgery and medical director of the pediatric trauma program at ECU Health Medical Center, and the surgical team to bring this technique to ECU Health.
“Bringing this technology to ECU Health means we can offer our youngest patients the latest advancements in surgical care right here in eastern North Carolina,” said Dr. Longshore. “We’re excited about the possibilities this opens up for pediatric surgery and are committed to expanding access to these innovative procedures.”
Robotic-assisted surgery builds on the strengths of traditional laparoscopic techniques, offering enhanced precision and efficiency, with some procedures completed more quickly. The technology reduces physical strain on surgeons, supporting long-term physician wellness. Both techniques offer similar incision sizes and recovery times.
“The introduction of pediatric robotic surgery at ECU Health marks a significant step forward in expanding minimally invasive surgical options for children,” said Tara Stroud, vice president of Women’s and Children’s Services, James and Connie Maynard Children’s Hospital at ECU Health Medical Center. “ECU Health continues to drive innovation in pediatric surgical care, ensuring that children in the region have access to the highest quality treatments available.”
For Melissa and Jimmy Worrell, their love story started with a horse. Melissa, a horse trainer and riding instructor at the time, met Jimmy when he brought his horse to the barn where she worked. That chance encounter led to marriage in 1988, a move from New Jersey to North Carolina and a life filled with love, adventure and raising their quadruplets.
But in recent years, their journey took an unexpected turn. Jimmy was diagnosed with kidney disease and placed on the transplant waiting list. For nearly eight years, he waited, knowing that each passing day brought him closer to dialysis—a life-sustaining but time-consuming treatment that filters waste from the blood when the kidneys can no longer do so.
“Dialysis is a lifeline for many patients, but machines just cannot do the work of an organ that works automatically, 24/7,” said Dr. David Leeser, professor and chief of transplantation at ECU Health Medical Center. “We know that when a patient is transplanted, they gain a tremendous boost to their quality of life, and they will live longer as well. Transplantation is by far the best available renal replacement therapy available to patients with kidney failure.”
Throughout the process, doctors frequently asked if he had identified a potential donor. Jimmy never asked Melissa to consider donating, but she made the decision on her own.
“I knew I was O-negative, so I figured I’d at least get tested,” Melissa said. “I thought, well, I had to at least try.”

The couple was shocked to learn she was a perfect match.
Throughout the process, Melissa was supported by a donor advocate at ECU Health—someone who had been through the experience and could provide firsthand insight. She believes this kind of support is crucial for potential donors.
“When you’re thinking about doing this, it’s good to talk to someone who has been there,” Melissa said. “It’s reassuring to know that life goes on and that we’ll both live normal, healthy lives.”
Their transplant surgery was successfully completed Nov. 12, 2024. Melissa, now a recreational therapist and volunteer with Team River Runner in Wilmington, which provides veterans and active-duty military with healing opportunities on the water, specifically outrigger canoeing, kayaking, paddle boarding and rowing, took time off to recover. Jimmy returned to work earlier than expected, eager to get back to normal life. More importantly, the transplant has given them back their active lifestyle.
“Before, if I asked him to go for a walk, he’d say, ‘I can’t do that,’” Melissa said. “Now, we can do things together again. It’s a big change.”
The couple enjoys boating along the Intracoastal Waterway, dining out, going for walks and simply spending time together. Beyond her personal experience, Melissa hopes to raise awareness about living kidney donation.
“It’s amazing how something so small can make such a big difference in someone’s life,” she said. “People are often surprised when they hear what I did, like I was risking my own health. But the doctors wouldn’t have allowed it if I wasn’t okay. I think if more people heard these stories, they might consider donating. I especially want to thank the friendly and caring transplant team at ECU Health, who provided great pre and post care.”
For the Worrells, this journey has deepened their bond and given them a renewed appreciation for the simple joys of life. Now, with Jimmy’s health improved, they’re looking forward to many more years of adventure together.
Resources
In 1984, Jaimie Yahnker faced a decision: move to North Carolina with his parents or stay in Long Island, New York.
“Here I was fresh out of high school,” Jaimie recalled. “I went to a school for individuals with cerebral palsy, which incorporated physical therapy and the like into your education, so I graduated when I was 20. After graduation, I decided to move with my parents to North Carolina, which was the best decision I could have made.”
Jaimie was one of seven children, and three of his other siblings also lived in North Carolina. In November of that year, Jaimie was hired by ECU Health Medical Center, then Pitt County Memorial Hospital, and he’s never looked back.
Jaimie’s first job with the system was at the Information Desk, but when that didn’t work out, his connection to what was then called the Education Department through his sister, who also worked at the hospital, landed him a position putting together orientation packets for new team members on a part time basis.

“That went well, and I stayed in that role until I lived in North Carolina for a year and achieved my residency,” he said. At that point, Jaimie knew he wanted to go to school, so he attended Pitt Community College in the morning while working in the education department during the afternoons. “That’s how I got my degree in human services,” Jaimie said.
After graduation, Jaimie applied and interviewed for several different jobs. “No one was hiring,” he said. It was about that time, also, that the Americans with Disabilities Act (ADA) was signed into law, something ECU Health’s then human resources (HR) director Charles Fennessy and the hospital’s HR department knew about and supported.
“He [Charles] was determined to help me all he could,” Jaimie said. “He saw the fire in me. He knew I was trying hard to find work and not getting offers, so he found a full-time position in the Insurance Department under Financial Services, and I worked in that department for nine or 10 years.” During this time, Jaimie also went back to Pitt Community College to get his degree in human resources.
Jaimie enjoyed his work, but he didn’t enjoy being in a cubicle all day. “I’m a people person,” he said. At the same time, Jaimie tore both of his rotator cuffs after walking with forearm crutches for years, an injury that required surgery to repair the damage.
“I knew Dave McRae [the chief executive officer at the time], and I told him I wasn’t sure how my recuperation would go, but that if I could return to work, I didn’t want to be in a cubicle,” he said. After Jaimie’s surgery, McRae helped him find a clinical support position at the front desk in the Rehabilitation department, where he worked first under Martha Dixon, and later with Wanda Bennett.
“Later I worked in hospitality (now called experience) where I stayed for a few years and through COVID,” Jaimie said. “The new rehab director, Dr. Felicia Collins, asked me to come back to their department and I’ve been here ever since.”
While he’s served in several positions across the hospital, Jaimie said he likes his current role because, “I am a good role model for the patients and their family members. They see me do what I am doing, and they think they can also be successful.”
Jaimie also enjoys the people he works with. “They are a great team, very supportive,” he said. “I saw one of our recreational therapists here as a patient, when she had Guillain Barre, and just like me, she had therapy here and was inspired to come back and work. I’m very happy in rehab.”
While he gets asked from time to time when he plans to retire, he has no intentions to leave anytime soon. “Working gives me a reason to get out of bed. I have responsibilities, and I’m comfortable here. It’s the best for my personality.”
Resources
ECU Health recently hosted the Provider Patient Choice Awards at a luncheon honoring more than 200 ECU Health providers.
The Provider Patient Choice Awards recognize ECU Health providers who rank in the top 10% in the nation in the Watson Human Caring[1] question for “Creating a caring environment that helped me heal.”
Attendees, both in-person and virtual, heard from ECU Health leadership as they thanked the winners for their work and discussed how compassionate care impacts patients, families and the health system. ECU Health CEO and Dean of the Brody School of Medicine at East Carolina University Dr. Michael Waldrum said there is no greater honor than being recognized by the patients and community members a provider serves.
“We teach medical students and nurses about all of the technicalities and the hard work that it takes to take care of other humans,” Dr. Waldrum said. “However, one of the most important elements of excellence in providing health care is connecting with other people and caring. We know the data is very clear, it’s been shown many times that the better connection you have with that patient, the better they do. They’ll take their medications, they’ll follow your advice and their outcomes are better.”
He also noted that with expanding technologies and societal changes, the connection aspect in health care is needed now as much as ever and acknowledged a shift toward even more compassionate care in recent years. He expressed deep gratitude for the care teams making caring environments for patient and their families a priority.
Dr. Jason Foltz, chief medical officer with ECU Health Physicians, shared that the morning of the event, he had multiple visits with patients who did not have medical needs, but just needed someone to talk to about anxieties around medications or upcoming procedures. He said these interactions with patients and families are just as important, if not more important, than the medical care he provides.
“These are our patients and what they need is what you all provide them, which is a listening ear and the fact that you choose to care,” Dr. Foltz said. “At the heart of all this, everything we do—we’re just people serving people. That’s what today is about, to recognize and highlight that amazing spirit you bring and what really makes ECU Health, ECU Health.”
Dr. James Powell, a Patient Choice Award recipient, agreed with Dr. Foltz about the heart of a provider’s work. He said his team makes all the difference by starting each visit with a warm smile and a helping hand for patients.
He said he was excited to share the award with his team and recognize them for going above and beyond and developing positive patient relationships, which he uses for the foundation of each visit.
“We’ve been truly blessed, because we have a wonderful head nurse who has really created a good vibe among the staff as they go through day-to-day work. I’m sure a lot of you feel the same way about your staff,” Dr. Powell said. “When patients are calling, they’re calling because they need something. The something that they get is an answer to that question but a lot of times, it’s also just something that helps to calm them down and to make them feel good about things. I think that we’d really be remiss on a day like today if we didn’t think about the staff with whom we work, who really allow us to do what we do every day.”
ECU Health Chief Experience Officer Dr. Julie Kennedy Oehlert served as Master of Ceremonies for the event and encouraged providers to take their award boxes – filled with a plaque, stickers, star pins and more – and share them with their teams who support them every day.
She said during the event that the awards are truly special because they come from the patients these providers serve.
“The patients really showed us that you create a caring environment,” Dr. Oehlert said. “As much as you love them, they love you right back. We just want to thank you all for everything you do every day and recognize that the patients think you are amazing.”
About ECU Health Patient Choice Awards
Established in 2023, Patient Choice Awards recognize and honor ECU Health team members and providers for their dedication, effort and support to eastern North Carolina and the patients and families ECU Health serves. Winning teams and providers are chosen based upon commentary and feedback collected from patient surveys. Recognition events are held throughout the system in the fall and winter to showcase the people and teams who go above and beyond in support of our mission to improve the health and well-being of eastern North Carolina.
More Reading
Teams across ECU Health recognized by patients with Patient Choice Awards
[1] Jean Watson’s Theory of Human Caring is a foundation of patient care and focuses on the importance of the interpersonal relationship between a caregiver and care receiver. The theory states that this relationship helps not only the person receiving care, but the caregiver as well.

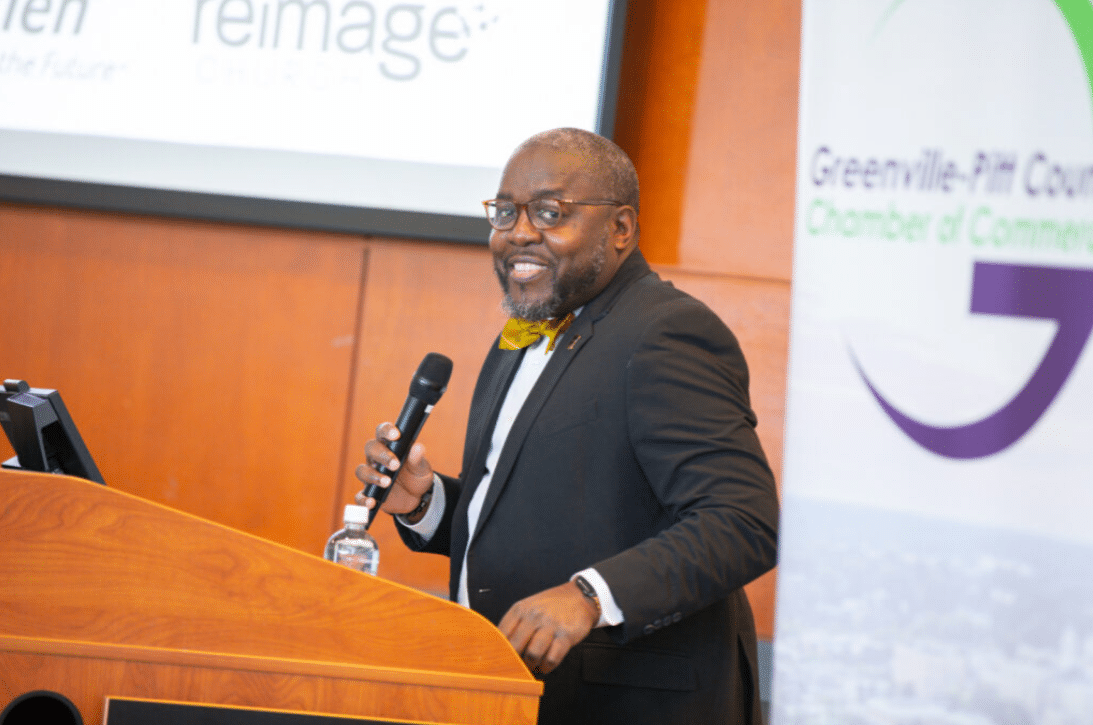
Community leaders, elected officials and eastern North Carolina residents came together on Jan. 20 for the 28th annual Community Unity Breakfast, hosted by the Greenville-Pitt County Chamber of Commerce.
The event brings together the community to reflect upon the life and legacy of Dr. Martin Luther King Jr. while celebrating and expanding diversity initiatives in Greenville and Pitt County.
ECU Health sponsored the event along with other organizations in the area and had the opportunity to present a speaker. Brian Floyd, chief operating officer of ECU Health, represented the system and shared a few words.
Floyd said the word that stands out to him the most during Dr. Martin Luther King Jr. Day is love. He related harmony in a community to the harmony couples seek in relationships with others.

“The hardest thing sometimes is to put ourselves aside in the interest of someone else,” Floyd said. “Yet, relationships and marriages are hard – and that’s when you choose to be with someone you share common values, beliefs and interests with. If we can see that, then certainly we must recognize that living in a community and being in harmony together requires a little bit of work and self-reflection.”
He said ECU Health is proud to see unity in nine hospitals and more than 225 clinics across the health system each day through the life-saving care team members provide. The 1.4 million people ECU Health serves and the 15,000-plus team members are all unique, but care and love is the same.
Floyd also said training students from the Brody School of Medicine at East Carolina University and nursing students from ECU and other local colleges is a privilege and opportunity to pass on the importance of love and care for patients.
“If you read behind Dr. Martin Luther King Jr., you’ll note that love is at the core of the unifying work of bringing people together. We all want to come together and do this really important work to love and care for eastern North Carolina,” Floyd said. “If you ever see the life-saving moments, when our team of 15 or 20 excellent, well-trained people come together around a patient, it always fascinates me how different they all are. They look different, they sound different, they come from incredibly different places and backgrounds. Yet they work in really great harmony in those urgent crisis moments because the need of the patient is coming first.”
Portia Willis, Greenville City Council member, gave the keynote speech during the event. Willis is also the co-founder of Young Scholars and Leaders Institute. Chad Tucker, director of Volunteer Services at ECU Health Medical Center, serves as co-chair of the Community Unity Planning Committee and introduced Willis.
Willis spoke on a number of topics during the event but came back to the refrain that the answer to challenges we face are in the communal “us.” From issues we might face on a team, in business or as a community, it’s on us to come together and work toward solutions.
“This morning, we’re reminded not only of the words of Dr. King, but the example he set. Today is a call to action, a vision of equality and a commitment to the higher ideals of justice, peace and unity,” Willis said. “Dr. King once said, ‘Life’s most persistent question is: What are you doing for others?’ Today as we reflect on those words, we’re reminded that service is not only an affect, but it’s a way of life.”

It’s been a year since the state of North Carolina passed Medicaid Expansion, bringing with it much-needed coverage and financial reprieve for the communities ECU Health serves.
North Carolina’s former governor, Roy Cooper says “One year of Medicaid expansion in North Carolina,” said Dr. Michael Waldrum, ECU Health CEO and Brody School of Medicine’s dean. “As we celebrate this moment. We’re proud to say we’re building the national model for rural health care right here in eastern North Carolina.”
That model depends on Medicaid Expansion and affordable access to care.
“It is a comprehensive health benefit where you can go see a primary care provider, have it covered,” said Kody Kinsley, secretary of the North Carolina Department of Health and Human Services. “Where you can have pharmacy, vision and dental and a copay that is never more than four dollars.”
Cost-effective health care is an important component, but it’s not the only one. ECU Health’s Dr. Karen Coward states “This is the power of Medicaid expansion. It’s not just about providing coverage, it’s about dignity.”
And peace of mind for the patients who need it most. Medicaid Expansion beneficiary and ECU Health patient, Darcy Guill spoke during the event.
“Sixteen years ago, I found myself unable to work and I lost my health insurance,” Guill said. “For the next 15 years, I was either uninsured or under insured.”
Her inconsistent coverage hit home in a different way following a car accident.
“I was hospitalized for two months right here at ECU Health,” Guill said. “I knew I was going to be uninsured again and I didn’t know what to do and I was terrified.”
That panic subsided when she realized share now had another option.
“It didn’t dawn on me at first that it was going to include me but it did,” she said. “Medicaid is literally saving my life. I am the person that benefitted from it and I am no different than all the other people that could benefit.”
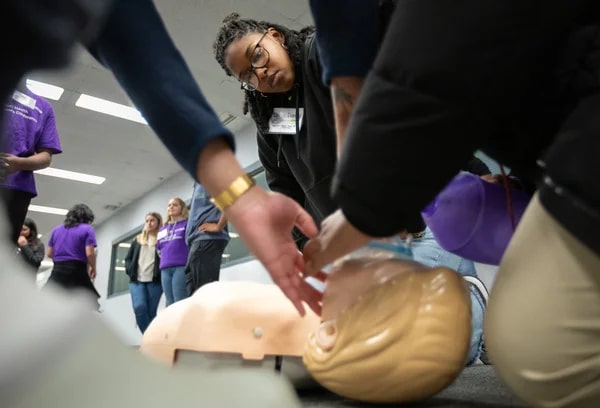
Success stories start as dreams we harbor in our youth. Career days such as the third Future Health Professionals Conference Nov. 23 help fill in the critical details that make it believable.
Nearly 100 students from 11 counties in central and eastern North Carolina made the trip to Greenville and the Health Sciences Campus of East Carolina University for the event hosted by ECU Health and the university.
D.H. Conley senior Chance Frederick of Greenville was one such student, but one of only a handful who had taken part in the very same event last year.
“I was really amazed the first time by everything they offered me, especially the hands-on experience in the dental clinic. It really made me want to come back,” he said. “And just being able to network and meet people, to see these faces that I just know will be really beneficial for my future, I can’t get that anywhere else.”
Investing in the Future of Health Care
Students listened to medical professionals speak about their career arcs, then walked to nearby schools of medicine, dental medicine and nursing to tour facilities and experience hands-on curriculum at training stations and simulations.
“Engaging high school students early is crucial to addressing the national health care shortage, especially in rural areas like eastern North Carolina,” said Koai Martin, an equity and special projects consultant for ECU Health.
Both the health system and the medical school have a demonstrated history and mission of training and employing health care professionals to work in underserved areas of the state. Efforts such as the Future Health Professionals Conference help “create a pipeline of providers and health care professionals who understand the unique challenges of rural health care,” she said.
“Ultimately, it’s about investing in the future of health care while uplifting the region our ECU Health and ECU medical school proudly serve,” Martin said.
Several students from the Brody School of Medicine led hands-on life support demonstrations and Stop the Bleed simulations. Dr. Calvin Blocker, a resident physician at the school and ECU Health, discussed the epidemiology and pathophysiology of strokes and methods for detecting and identifying stroke symptoms that concluded with an interactive experience involving the examination of brain models and specimens to show areas commonly affected.
“The Future Health Professionals Conference gives high school students insight into the daily lives of our students and the responsibilities of practicing professionals,” said Milton Bond, who directs the medical school’s Pathways to Health Careers Program. “It is important for ECU to commit resources to support initiatives like this to invest in building the future health care workforce.”
In the Middle of the Journey
“I knew I wanted to be a dentist from about 10 years old, but I didn’t get to do anything like this, and no one in my family was in the medical or dental field,” said Dr. Scarlett Walston, a clinical assistant professor in the School of Dental Medicine. “I think it’s really cool just for them to be able just to explore. Maybe one of them falls in love with dentistry, and maybe we’ll see them in the application cycle in a few years.”

Walston said preparing for the DAT — the Dental Admissions Test — is something some committed students begin even in high school. Outreach such as the conference can give young students a shot of hope at a time when they might feel bewildered and disadvantaged navigating such a competitive track.
“Helping the next generation find their path is always important,” she said.
Jennifer Kovacs is a career nurse and health sciences high school teacher who brought eight students to the conference from Dare County. She says health care is a wide-ranging industry that employs trades and hourly workers alongside highly trained specialists.
“There are so many opportunities. If blood and sickness are too much, there’s a cubicle you can sit in and be by yourself and still contribute to health care,” Kovacs said. “There’s a microscope; be a researcher developing a new drug or running lab tests. You can sterilize surgical equipment — another surgery cannot begin until you’ve sterilized from the last one.”
Her students, she says, are weighing careers on several factors. Passion is one, but years spent in college and student debt factor into plans.
“Health care is not just doctors and nurses. It is other clinicians. It is secretaries. It is custodial, meal services, environmental services. And it is a family. … and therefore you can get students involved in any of those aspects,” she said.
Frederick, the 17-year-old senior, put his statistical chance of eventually becoming a dentist at the dizzying tip of the range, 99%.
“I’ve wanted to be a dentist ever since I was 3 years old,” he said. “That was the age of my first dental appointment. If I’ve been into it for 14 years at this point, I think I can take the next 14 to make it happen.”
And he expects to make this dream a reality right in his hometown, at East Carolina University.
“Today, I got to meet with a bunch of second- and third-year dental students. I got to walk right into the lab and immerse myself, and they made me feel included,” he said. “So even though I haven’t started, I saw what it was like to be in the middle of the journey, and it makes me feel like, you know what, I can really do this.”
Greenville, N.C. – Trish Baise, ECU Health chief nursing executive, was recently honored as one of Becker’s Hospital Review’s 2024 Chief Nursing Officers (CNOs) to know. Since stepping into the role in 2022, Baise has cultivated a dynamic nursing environment that drives innovations to enhance patient care quality and elevate patient experiences across eastern North Carolina.
“This recognition by Becker’s reflects the collective efforts of the incredible nurses across ECU Health, all of whom are dedicated to creating an environment where nurses and patients alike can thrive,” said Baise. “Together, we are driving innovative approaches in rural health care, committed to excellence in all we do and enhancing patient care across eastern North Carolina. I am honored that ECU Health has been recognized for this commitment.”
Tasked with addressing nurse staffing shortages, managing budgets and fostering growth opportunities for emerging nurses, the nursing leaders recognized by Becker’s play a crucial role in shaping the future of nursing.

Beyond leading nursing departments, CNOs drive innovative initiatives that uphold high patient care standards. Their roles demand a unique blend of clinical expertise and executive leadership. This list honors CNOs for their commitment to optimizing health care.
Baise has led efforts to establish a supportive environment where both nurses and patients can thrive. Under her leadership, ECU Health has achieved its third Magnet recognition, underscoring a commitment to nursing excellence. The Advancing Nursing Practice and Excellence (APEX) initiative has been foundational to this strategy, focusing on innovation, research and collaborative efforts to advance nursing in rural health care. Through partnerships with East Carolina University and local colleges, ECU Health also invests in the future of nursing, offering residency programs to equip new nurses with essential skills. This vision represents ECU Health’s dedication to defining a new standard for patient care and nursing excellence in eastern North Carolina.
“As the region’s largest health care provider and educator, ECU Health has a unique role in shaping community health, and Trish understands that our mission’s success depends on attracting the best providers, nurses and care teams to our health system,” said Dr. Michael Waldrum, CEO of ECU Health and Dean of the Brody School of Medicine at East Carolina University. “Trish’s dedication to service and our mission aligns with ECU Health’s work to build the model for rural academic health care. ECU Health is proud to lead the way in defining the future of nursing in our region.”
Resources
This year, the ECU Health Medical Center’s microbiology laboratory upgraded its technology by adding the BD Kiestra Total Lab Automation (TLA) system. The new equipment improves standardization in laboratory processes, enhances lab efficiency and centralizes microbiology testing. This automated solution to laboratory challenges represents ECU Health’s ongoing pursuit of innovation, efficiency and process improvement.
The Kiestra TLA system is an end-to-end automated lab culture workflow from plate labeling, inoculation, incubation, plate reading, imaging, reading and follow up work, to maximizing staff productivity. “Previously, after incubating cultures, you took the plates out and read each one from the oldest to the newest, but if the culture wasn’t robust enough, the plate had to go back in the incubator,” Caryl Havasy, the system administrator of laboratory service lines, said.
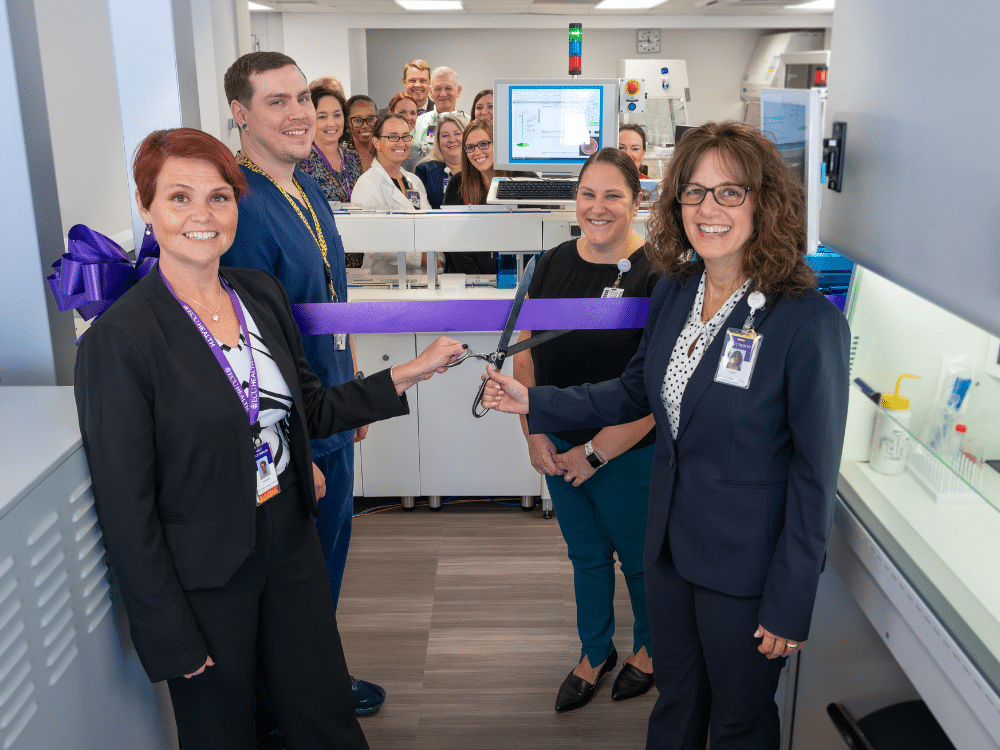
Heather Duncan, the director of ECU Health Medical Center’s laboratory services, further explained the challenge. “Think about incubating plates like baking a cake in the oven,” she said. “The whole time the plate is out of the incubator, it’s not growing the organism, just like a cake stops baking once you take it out of the oven. This can delay an organism’s growth and delay the test results.”
Furthermore, reading plates was subject to human experience and error. The Kiestra, Havasy and Duncan said, takes photos of the plates and uses AI algorithms to see an organism’s growth before the human eye can detect it. “This technology means there’s no variation in how the sample is applied to a plate” Duncan said. That means there’s no delay due to rework, and there’s less room for error.
Acquiring the technology was a four-year process, which included establishing a business case, investing funds, working through construction to get the microbiology lab space ready, installing equipment and training lab technicians. The lab opened officially this past July, and on Oct. 8, the team hosted an open house to celebrate the new technology with a ribbon cutting ceremony and tours for those interested in seeing the new equipment.
It was a great opportunity for Dr. Niti Armistead, the chief quality officer and chief clinical officer at ECU Health, to see the newest technology in action. “The Kiestra is an investment in our people, specifically our laboratory and microbiology team,” she shared. “These are highly trained professionals, and this technology takes away manual, inefficient tasks and allows them to use their skills and education to the fullest extent. This in turn drives improvement in safety with fewer manual errors, efficiency and professional fulfillment. It is another example of how we are advancing our vision to be the national model for rural health as it will be processing specimens from all of our hospitals.”
Jay Briley, the president of ECU Health Medical Center, also attended the event. “It’s exciting to see ECU Health continue to invest in cutting-edge technology like the Kiestra Total Lab Automation system. The system streamlines our processes, reduces manual errors, and allows our highly skilled lab professionals to focus on what matters the most: delivering timely, life-saving results,” he said. “The Kiestra TLA system is a testament to ECU Health’s commitment to innovation and the health and well-being of our patients.”
Andy Zukowski, ECU Health’s chief financial officer, highlighted the value of ECU Health’s investment in this new technology: “The Kiestra Total Lab Automation system represents significant innovation and value for ECU Health. By streamlining our microbiology lab’s processes, it enhances the patient experience and quality of care we provide all while improving throughout and cost savings. The long-term return on investment is clear, as it positions us to continue delivering innovative high-quality care while maintaining fiscal responsibility.”
Amy Campbell, PhD, RN, CPHQ, LSSBB, quality nurse specialist III, represented ECU Health on Sept. 25 at a side event held in parallel to the 79th session of the United Nations (UN) General Assembly in New York City. The meeting, titled “2030 Global Agenda for Sepsis for Attaining Sustainable Development Goals,” was convened as a collaborative effort of the Global Sepsis Alliance (GSA), Medical Women’s International Association, Sepsis Stiftung and UNITE Parliamentarians Network for Global Health.
The meeting was the first-ever global strategy spearheaded by the GSA, with collaboration from 70 partner and member organizations from Regional Sepsis Alliances across Africa, Asia-Pacific, the Caribbean, eastern Mediterranean, Europe, Latin America and North America. The meeting’s objectives were:
- To present the 2030 Global Agenda for Sepsis as the first multi-year global strategy to alleviate the significant human, societal, economic and health care burden of Sepsis.
- To reach consensus on the urgent need for reinvigorating the Sepsis responses at global, regional and national levels for the attainment of 2030 SDGs including the aspirations for Universal Health Care, Maternal, Neonatal and Child Health, AMR, Pandemic PPR, Gender Equality, Peace and Partnerships for Development.
- To discuss the critical role of health care workers, especially the medical women, representing over 70% of the health workforce globally, in the promotion and implementation of the 2030 Global Agenda for Sepsis.
- To call for establishment of a High-Level Political Platform for Sepsis to lead integration of this global health threat into the mainstream of health and development dialogue and architecture, including G7 and G20 Summits, World Health Assemblies, UN General Assemblies, and World Economic Forums.
Dr. Campbell was personally invited to attend and speak by Dr. Mariam Jashi, MD, MPH, MPA and the CEO of the Global Sepsis Alliance, and Michael Wong, founder and executive director of the physician-patient alliance for health and safety. This invitation came as a follow-up to the 2024 World Sepsis Congress held this past April, during which Campbell served on the Scientific Committee. “I saw the invite and initially blew it off,” Dr. Campbell laughed. “I wasn’t sure it was real.” But after reassurance the invitation was legitimate, and with the encouragement of her team and Michael Wong, Dr. Campbell decided to go to New York. “I had a training session scheduled at work, but my colleagues covered for me,” she said. “I’m so thankful to my team and leaders who made it so I could attend.”
Once she arrived at the New York University campus, where the parallel session was held, Dr. Campbell said she met many leaders from across the world. “I met Dr. Eleanor Nwadinobi, the president of the Medical Women’s International Association (MWIA), Thomas Heymann, the president and CEO of the Sepsis Alliance and the Honorable Dr. Ricardo Baptista Leite, a member of the Portugese Parliament. People were speaking all these different languages and here I was from eastern North Carolina.”
The meeting focused on early detection of sepsis and how to treat patients with sepsis, no matter where they live. “As one of the speakers, I had the opportunity to emphasize the urgency of early detection, the critical need for continued research and the importance of securing funding so that everyone, regardless of their geographic location, can receive the same standard of care and chance for survival,” Dr. Campbell said. The speakers also discussed what they anticipated to be the next big problem with sepsis: antibiotic resistance.
Dr. Campbell said it was a great opportunity to represent the work she and ECU Health are doing to address the global problem of sepsis. “The attendees were impressed with the work we’re doing. ECU Health is a big deal; we have incredible people and talent, and we deserve a seat at the table,” she said. And next year, she has a seat waiting for her. “I’ve been invited back to speak next year, and I’ll work more with the GSA,” she shared. “We all have a lot to learn and do. Sepsis transcends borders, affecting individuals of all ages, races and socioeconomic backgrounds. However, the most vulnerable populations – children, the elderly and those in low-resource settings – are disproportionately impacted. Sepsis doesn’t wait, and neither can we.”



