Greenville, N.C. – ECU Health Medical Center has once again earned Magnet® recognition, which is awarded every four years and represents the highest national honor for professional nursing practice, marking its third consecutive successful accreditation for exemplary nursing practice. The American Nurses Credentialing Center’s Magnet Recognition Program® distinguishes health care organizations that meet rigorous standards for nursing excellence.
“Earning Magnet recognition is a tremendous honor and reflects our commitment to delivering the highest quality of care to eastern North Carolina,” said Trish Baise, chief nursing executive, ECU Health. “Our repeated achievement of Magnet recognition is an incredible source of pride for our nurses and drives our entire nursing program to strive harder each day to meet the health care needs of the people we serve This prestigious designation is a testament to the dedication, professionalism and compassion of our outstanding nursing team in collaboration with our interprofessional partners across the health system.”

Research demonstrates that Magnet recognition provides specific benefits to health care organizations and their communities, such as:
- Higher patient satisfaction with nurse communication, availability of help and receipt of discharge information.
- Lower risk of 30-day mortality and lower failure to rescue rates.
- Higher job satisfaction among nurses.
- Lower nurse reports of intentions to leave their positions.
Magnet recognition is the gold standard for nursing excellence. To achieve initial Magnet recognition, organizations must pass a rigorous and lengthy process that demands widespread participation from leadership and staff. This process includes an electronic application, written patient care documentation, an on-site visit and a review by the Commission on Magnet Recognition.
Health care organizations must reapply for Magnet recognition every four years based on adherence to Magnet concepts and demonstrated improvements in patient care and quality. An organization reapplying for Magnet recognition must provide documented evidence to demonstrate how staff members sustained and improved Magnet concepts, performance and quality over the four-year period since the organization received its most recent recognition.
“ECU Health nurses carry forth a legacy of excellence, which was first recognized by the Magnet® Recognition Program in 2013,” said Brian Floyd, chief operating officer, ECU Health. “Since then, our nurses have continually raised the bar for patient care and inspire every member of our team to strive for excellence every day. This year’s Magnet recognition affirms our commitment to meeting our mission of improving the health and well-being of eastern North Carolina. We could not be more proud of the excellent nursing teams in collaboration with our interprofessional partners that made this recognition possible for the third time.”
ECU Health Maynard Children’s Hospital’s Neonatal Intensive Care Unit (NICU) offers the highest level of care for the most fragile of patients; it is staffed with a team of experts who care for critically ill or premature newborns. One of those specially trained nurses is Tara Stroud, who was named in February the vice president for Maynard Children’s Hospital, Women’s Service Lines and Community Health Programs. Recently, Tara received another well-earned recognition—this time as a recipient of the March of Dimes Excellence in NICU Leadership Award.
The national award honors NICU leaders who effectively support their team, advance the care of patients and the operation of their unit, have strategic vision and have excellent communication skills. Only one winner is recognized annually, and this year, Tara Stroud was honored with the award at the Synova 2024 NICU Leadership Forum.
Tara didn’t initially consider nursing as a career when she was younger. “I thought I would be a vet because I love animals,” she said. “But a love for nursing found me.”

After a clinical rotation in a NICU, Tara said she knew that was exactly where she wanted to be. “I wanted to do something that had meaning and value. The babies in the NICU are so critically ill and depend on you for everything, but they’re also so resilient. There’s something about the babies that gives you a different impression on life. That’s what captured and kept me.”
An eastern North Carolina native, Tara joined ECU Health in 2006 after receiving her BSN from East Carolina University. She’s since received an MSN as a neonatal nurse practitioner and her doctorate in nursing executive leadership, and she is excited about the road ahead for ECU Health.
“When you work for ECU Health, the possibilities are endless. When I started in the NICU, I didn’t know where my career would take me. Advancing my education and going into leadership roles was an opportunity ECU Health gave me.” She also loves that her work gives back to her community. “Eastern North Carolina is my home. I want to be where women and children receive exceptional care. If we weren’t here, some of our babies wouldn’t survive a trip. It’s critically important that we are here.”
Tara loves working with the NICU team, a group of leaders and team members who “lead with their hearts,” as she puts it, but she also sees many opportunities in her new role as vice president.
“It’s a chance to solidify the vision for ECU Health for the future of women’s and children’s care across the system,” she said. “We’re focusing on a more holistic view of health across the continuum of care, because both maternal and child health is important to our future. I’m excited to lead ECU Health to continue to impact that health continuum for both mother and child.”
This passion and dedication to her field is why she was recently recognized as the 2024 March of Dimes Excellence in NICU Leadership Award winner. Although “not a crier,” Tara admits she teared up when she learned she won the award. It was even more special that she was able to accept the award at the Synova 2024 NICU Leadership Forum with her husband and daughter in attendance.
“Winning the award surprised me,” she said. “I never thought I would win a national award, but when you’re focused on trying to provide exceptional care, sometimes you don’t realize the impact you’re having on others.”
That impact was clearly noted in Tara’s nomination form, which was submitted by her team and without her knowing. “Tara is an innovative leader who has a vision for the future unlike any I’ve worked with,” said one nominator. Another’s quote read: “She has left a forever impact on the leader I strive to be . . . thank you for leading us to excellence.”
Tara acknowledged that one of her greatest goals and achievements has been to guide her team members into leadership roles.
“My job is to grow the leaders of tomorrow. When my team said I have given each of them a chance to be leaders and make a difference in eastern North Carolina, that sticks with me more than anything,” she said. “To be recognized for this specific award for a population that is so important to me – and to know my team nominated me – it’s an award I cherish.”
The much-deserved award reiterates Tara’s focus on the future of ECU Health’s role in neonatal and maternal care.
“We are laser-focused on providing exceptional care for neonates and mothers in our region,” she said. “Babies in the NICU are getting smaller and surviving at younger ages year over year, and we are continuously adapting our care pathways to meet these needs. We’ve accomplished great work, but there’s more to be done.”
Resources
Greenville, N.C. – Tara Stroud, DNP, APRN, NNP-BC, NEA-BC, vice president of Women’s and Children’s Services, James and Connie Maynard Children’s Hospital at ECU Health Medical Center, was recently awarded the March of Dimes Excellence in Neonatal Intensive Care Unit (NICU) Leadership Award. Stroud accepted the national award at the Synova 2024 NICU Leadership Forum in Charlotte Harbor, Florida.
“I am deeply honored to receive the March of Dimes Excellence in NICU Leadership Award, especially knowing that my team nominated me for an award that recognizes excellence of care in a population that is so important to me,” said Stroud. “Our focus on improving the quality of care for neonates is unwavering, and this national award affirms that ECU Health is a model for exceptional care, particularly in rural communities. I am excited to help lead ECU Health in solidifying our vision for women’s and children’s care across eastern North Carolina.”
The March of Dimes Excellence in NICU Leadership Award honors NICU leaders who effectively support their team, advance the care of patients and the operation of their unit, have strategic vision and have excellent communication skills.

The NICU at Maynard Children’s Hospital offers the highest level of care for the most fragile of patients and is staffed with a team of experts who care for critically ill or premature newborns. Allyson Yelverton, director of Patient Care Services at the Level IV NICU, led the nomination initiative for Stroud’s team.
“Tara is an innovative leader who has a vision for the future, centered around the health and well-being of our patients,” said Kathryn Jarvis, senior director, Patient Care Services, Maynard Children’s Hospital. “She has helped grow high-performing leaders across the organization and serves with a passion for the patients and families we care for every single day. We were excited to nominate her and are so pleased that she was selected for this deserving recognition.”
An eastern North Carolina native, Stroud joined ECU Health in 2006 after receiving her Bachelor’s of Science in Nursing from East Carolina University. Stroud earned a Master of Science in Nursing as a neonatal nurse practitioner and a Doctor of Nursing Practice degree. Stroud worked in the NICU for many years and as senior administrator of Children’s Services at Maynard Children’s Hospital and was named the vice president of Women’s and Children’s Services in February. After becoming vice president, Maynard Children’s Hospital became the only Level I Pediatric Trauma Center serving eastern North Carolina.
“We at ECU Health are proud of Tara for being awarded the March of Dimes Excellence in NICU Leadership Award,” said Trish Baise, chief nursing executive at ECU Health. “Tara’s recognition at the national level is a testament to her unwavering commitment and the exceptional work her team does to advance the quality of care we provide. We are fortunate to have mission-driven individuals like Tara who help us lead the way in becoming the national model for academic rural health care.”
Youth across the state now have better access to mental health services as part of the expansion of the North Carolina Statewide Telepsychiatry Program (NC-STeP), an initiative of East Carolina University’s Center for Telepsychiatry.
Five pediatric primary care sites from the mountains to the coast are providing mental health care for children and adolescents through NC-STeP-Peds. Catawba Pediatric Associates, PA; Clinton Medical Clinic; ECU Pediatrics Clinic; Robeson Pediatrics; and Surf Pediatrics have joined the NC-STeP-Peds network. Once contracts are final, Peachtree Pediatrics in Cherokee will be established as the final of six sites.
NC-STeP-Peds is funded by a $3.2 million investment from the United Health Foundation (UHF). It continues the foundation’s commitment to work with ECU to address mental health challenges in North Carolina and provide mental health care services to children and adolescents in rural and underserved parts of the state.
Dr. Sy Saeed, director of the ECU Center for Telepsychiatry and founding executive director of NC-STeP, said the program offers an innovative approach to providing mental health services through expert consultation support for pediatricians and other clinicians through telemedicine. The model provides integrated care closer to home and deploys several technological innovations.
Each participating practice has a space within the clinic where patients meet virtually with a licensed clinical social worker (LCSW) for therapy sessions. Patients referred for psychiatric care will meet virtually with the psychiatrist in the same space.
“Telepsychiatry is a viable and reasonable option for providing psychiatric care to those who are currently underserved or who lack access to services,” Saeed said. “NC-STeP is also helping address a pressing and difficult challenge in the health care delivery system today with the integration of science-based treatment practices into routine clinical care. We are able to provide telehealth appointments for therapy with a licensed clinical social worker and psychiatric care at their pediatric clinic.”
The initiative’s virtual reality component, “NC Rural Kids Get Well,” has been created by Dr. Yajiong “Lucky” Xue, the Robert D. Teer Distinguished Professor in the Department of Management Information Systems, and students in the ECU College of Business. It provides a 3D community on the Roblox platform to serve three main purposes: education, peer support and surveillance.
Participating pediatricians are beginning to see results from the initiative in their practices.
Dr. Katie Lowry ’00, a pediatrician at Robeson Pediatrics, witnessed her hometown of Lumberton suffer two 100-year floods and the COVID-19 pandemic within a five-year span. She said the emotional impact resulted in increased anxiety and depression among her pediatric patients.
“We still have a long time to kind of get out of those difficulties that they were in,” she said. “Before we were able to get access to NC-STeP and provide that here in our office, we had maybe 150 on our waitlist for counseling.”
Lowry said being part of NC-STeP-Peds brings counseling and psychiatric care into her practice where children and their families are comfortable receiving health care.
“I think the biggest thing is [NC-STeP-Peds] has absolutely just crushed the stigma barrier,” Lowry said. “They’re receiving care in a place that they always receive their care. They don’t have to go to another facility. They don’t have to drive another hour. It’s right here for them, and that has been amazing for our patients.”
Overwhelming need
Dr. Christian Lige, a pediatrician at Surf Pediatrics in Dare County, said NC-STeP-Peds provides more timely care and is an avenue for providing more collaborative care for his patients. Prior to NC-STeP-Peds, the number of patients needing access to mental health services was overwhelming.
His practice sees patients from Dare and four surrounding counties. NC-STeP-Peds allows Lige to connect his patients to care more quickly. Lige said before NC-STeP-Peds, it could have taken nine months to a year to have an appointment with a psychiatrist.
“It’s really difficult to wait to see a psychiatrist for a year when a kid is struggling,” Lige said. “I’m hoping that with us talking with the psychiatrist, with our nursing staff and with the social worker, we’ll have a better picture of what’s going on with the patient.”
Through NC-STeP-Peds, Lige’s patients have their first virtual appointment with a behavioral health manager within weeks. The assessment determines if a psychiatric appointment is needed, and a virtual appointment with the NC-STeP-Peds psychiatrist follows in a few weeks.
“We see quite a few kids who go off and get admitted to a hospital because of an issue. They leave here and they’re on no medicines and they come back on four medicines. For a primary care doc to take care of four psychiatric medications is difficult,” Lige said. “So, we’ve had the ability now to speak to a psychiatrist so we can get input from them on the medicines and interactions, and that’s been very helpful.”
Assessing needs
In the 10 months since the sites launched more than 10,000 children and adolescents have been screened for mental health issues. Saeed said the screenings indicated more than 1,000 had demonstrated an increased likelihood of a behavioral health disorder and 1,800 had demonstrated at least a “mild to moderate” level of anxiety.
“Our ability to screen a large number of children since the program’s inception helps increase awareness of mental health issues in children and emphasizes the importance of addressing these concerns in these communities,” he said. “We currently have more than 200 children and adolescents receiving integrated behavioral and primary care services as part of the program.”
Paula Bowen is one of three LCSWs hired through the UHF grant for NC-STeP-Peds. As a behavioral health manager for the program, Bowen reviews referrals from the pediatric sites and holds virtual intake appointments with the patients and families.

“We’re available to diagnose, make referrals to the psychiatrist and [provide] therapy for the children,” Bowen said. “NC-STeP has increased availability to therapy for kids. We can provide a lot of education [for the families]. Even basic mental health education can go a long way to help parents and their children.”
Saeed said NC-STeP-Peds addresses mental health needs at a critical stage. A recent JAMA Pediatrics study of an estimated 46.6 million U.S. children showed that the national prevalence of children with a treatable mental health disorder who did not receive needed treatment or counseling from a mental health professional was 49.4%. In North Carolina, that number was 72.2%.
Much of that has to do with a shortage of mental health providers — 94 out of 100 counties in North Carolina are designated as mental health professional shortage areas, Saeed said.
“For a young person with symptoms of a mental disorder, early treatment can help prevent persistent and more severe problems later in life,” he said. “Thanks to UHF, ECU is doing everything we can to prevent that through NC-STeP-Peds.”
When Tabitha Tripp, perioperative supervisor at ECU Health SurgiCenter, was initially approached to host Project SEARCH students for internship rotations in 2021, she hesitated. Already managing a full workload, she questioned whether would have the time to mentor a student. However, recognizing the significance of providing these students the opportunity to learn valuable job skills, she decided to embrace the opportunity.
“These students are some of the hardest workers I have ever supervised,” said Tripp.
Project SEARCH is a one-year internship program for students with developmental and intellectual disabilities during their last year of high school offered at ECU Health Medical Center in partnership with Pitt County Schools. Students complete internship rotations across departments like hospital cafeterias, endoscopy, ECHO Lab, Environmental Services and more, where they learn real-world job skills like cleaning, stocking supplies and changing linens.

“Many of our graduates have gained competitive employment in our community upon graduating from the program,” said Katie Houmard, Project SEARCH instructor. “The main goal of the program is to prepare students with the competitive and marketable skills needed to transition into the workforce.”
Three years after deciding to work with Project SEARCH students, Tripp continues to get excited every time she has a student from Project SEARCH at the SurgiCenter.
“These students have become like family to us,” Tripp said. “I cannot begin to explain how rewarding it is to see how much the students grow. I am honored to take part in the growth, maturity, independence and confidence they gain during the Project SEARCH program.”
“There’s lots of different opportunities and advantages to bringing Project SEARCH into the community,” said Lisa Lassiter, director of Workforce Development, ECU Health. “We are showing the value students with different abilities bring to the workplace, fostering growth within the students and our team members. The community is also engaging with our students so they have the opportunity to see the gifts and skills they possess.”
Cindy Ferry, whose daughter Caitlyn just graduated from the program, has noticed a huge difference in her daughter after completing the program.
“The growth in Caitlyn this last year has been amazing,” Ferry said. “Caitlyn spent four years of high school learning the same things over and over and was, of course, bored. But when she started at Project SEARCH, she would jump off the bus at the end of the day and run up to tell us everything she did. She couldn’t wait to tell us what she did, what department she was in and how she got to learn new skills like making a bed or putting gloves on or creating packets for patients.”
According to Matt Fornes, program manager and job coach at Project SEARCH, both the students and hospital team members benefit from the program.

“There’s a good relationship where the students are learning the skills, and the department is learning from them as well, so they grow mutually,” said Fornes.
For Ferry, that growth can be seen in her daughter every day.
“Her growth at home is absolutely, positively astounding,” said Ferry. “The things she’s doing now that she couldn’t do before such as helping set the table and cleaning up the table at the end of the day, helping in the kitchen. She wants to help now, and a lot of times she’ll now say, ‘Mom, I can do that by myself now.’”
Caitlyn is one of nine Project SEARCH graduates from the program this year and is part of its ninth graduating class.
“This program is really amazing, and so are all of the people who run the program,” said Ferry. “They really have the kids’ best interests at heart.”
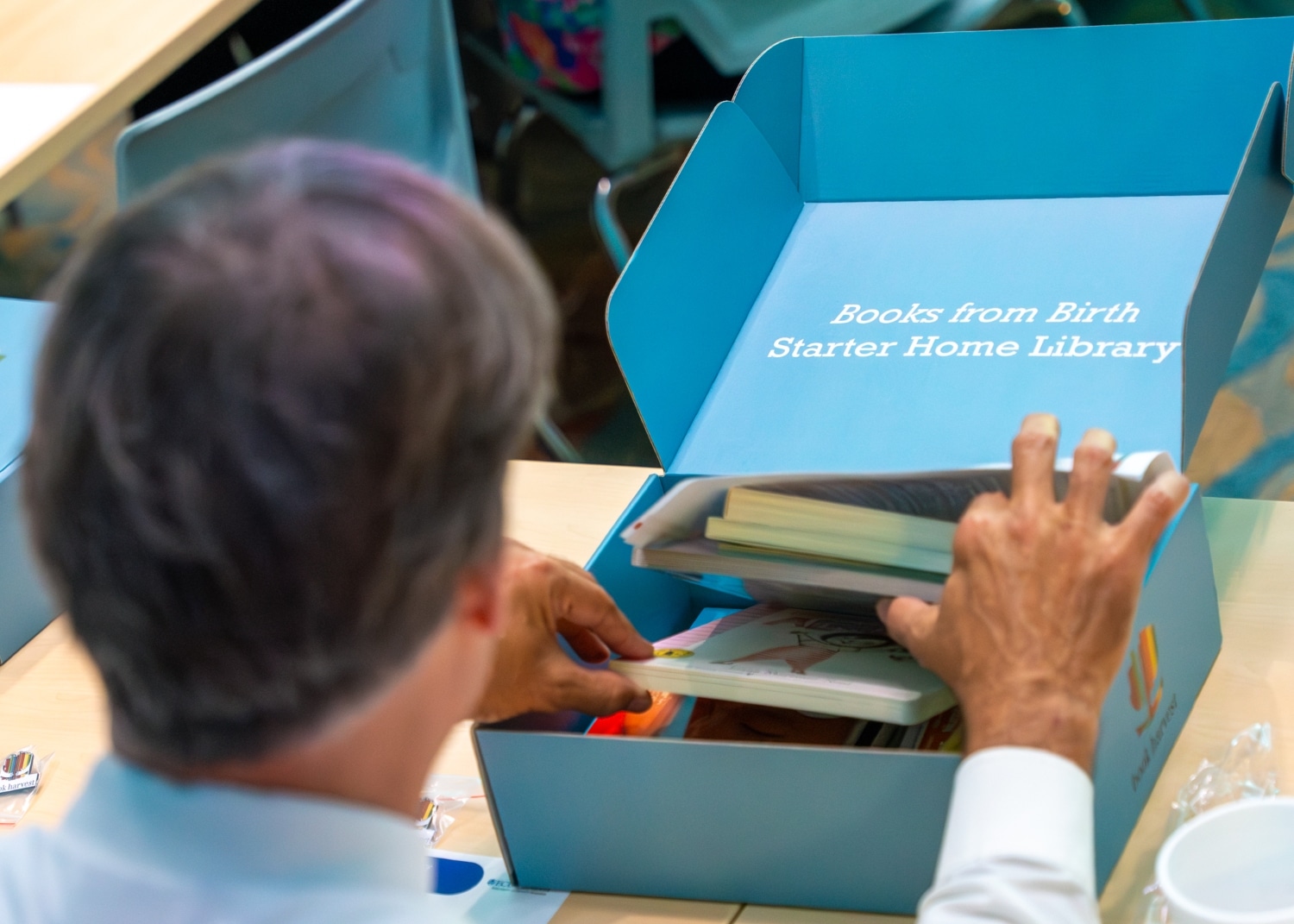
Books from Birth, a Book Harvest program, will begin providing children’s books to families of babies born in Maynard Children’s Hospital at ECU Health Medical Center starting in summer 2024. The books will help families foster early language and reading routines from a baby’s first days.
In preparation for the upcoming go-live, ECU Health hosted an event to educate team members at Maynard Children’s Hospital on Friday, June 14. Team members learned about Books from Birth, how these books can help families bond and improve early childhood education.
Book Harvest is an organization based in Durham that provides ongoing literacy support and an abundance of children’s books to families.
By partnering with Maynard Children’s Hospital, this collaboration will provide families and children in the East with the support and books they need to foster early language and reading routines at home from a baby’s very first days.
“The Books from Birth program is really designed to bridge early education and health,” said Book Harvest Chief Operating Officer Jeff Quinn. “Early literacy lays a foundation for life-long learning and healthy development. This program is meant to give children the opportunity to be what they want to be in life. We could not be more proud to help serve Pitt County and eastern North Carolina through this collaboration.”
N.C. House Rep. Tim Reeder, MD, District 9, secured funding of $500,000 for the project in the North Carolina State Budget. Rep. Reeder thanked Book Harvest and ECU Health for their willingness to partner on this important initiative. With his medical background in-mind, Rep. Reeder detailed the importance that early literacy has on the development of children as they grow, as well as the importance of improving access to education in eastern North Carolina.
“As a practicing physician, I see first-hand the benefits of early childhood literacy in terms of creating success in the classroom and in children’s behavior,” Rep. Reeder said. “Per data released from the state, about 50% of the children in Pitt County are not reading at grade-level. Early intervention and early reading is critically important to setting our children up for success. These books will help set families on a path to literacy that we know is really important to long-term development. I was proud to advocate for this funding and I am excited to see the impact this partnership will have.”
The Books from Birth program will provide a box of 10 board books, helpful reading education materials and a onesie for families who deliver babies in the Maynard Children’s Hospital.
“The benefit of giving these books at birth is that they help form loving and bonding relationships between babies and their caregivers,” said Dr. Matthew Ledoux, pediatrician in chief, ECU Health, chair of pediatrics, Brody School of Medicine at East Carolina University. “As a rural academic medical center serving a third of the state, it is incredibly valuable to get these books in the hands of families throughout eastern North Carolina. For that, we are very grateful.”
According to Tara Stroud, vice president, Women’s and Children’s Services, Maynard Children’s Hospital, the program will provide around 4,300 boxes of books to patients and families.
“This is our chance as a health system to change what it looks like for literacy in eastern North Carolina starting from the beginning,” said Stroud. “Our goal is that we demonstrate for our families the importance of books as a way to connect and bond with their child and improve their development.”

For Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center and Safe Kids Pitt County, the message she wants to get out is simple: “Never leave a child, senior or pet alone in a car, even for a minute.”
Walston’s message was amplified at a Hot Car Safety event in June hosted by ECU Health in partnership with the Pitt County Sheriff’s Office, Pitt County Health Department and the Martin-Pitt Partnership for Children, to demonstrate how quickly cars heat up.
The event included a demonstration with temperature gauges and s’mores roasting in a vehicle on hot, summer day. During an overcast, 88-degree day, the interior of the van rose to 113 degrees within 15 minutes.
The s’mores demonstration showed how quickly things can, quite literally, cook inside of a car when left alone. Volunteers handed out the s’mores to shoppers to explain the demonstration in a fun, interactive away.

“We host these types of events to raise awareness so parents are realizing how hot cars can become,” said Walston. “A car can heat 20 degrees in as quickly in 10 minutes. In our display today, it is already 113 degrees, and it’s only 86 degrees outside.”
According to Walston, about 17 percent of hot car fatalities occur in children intentionally left in the car. During this time, parents or caregivers are often running into the store or running an errand for a few minutes, thinking that will be fine.
“A lot of times, people think ‘I’m just going into the store for a few minutes,’ but anything could happen inside, from losing track of time to becoming distracted and forget the child,” Walston said. “There is a misnomer that if you crack a window and that will offer some less heat, but that really is a myth. It doesn’t affect the temperature of the car or cool the temperature down.”
Walston said it’s dangerous for anyone to be left alone in a vehicle because of how quickly they can heat up, but especially for children.
“Children’s bodies heat three to five times more quickly than adults,” Walston said. “They all have a smaller amount of body surface so they can’t cool themselves very quickly. A small child, like the families we’re serving today, they can’t verbalize when they’re thirsty if they’re under a certain age.”
More than 50 percent of child deaths from hot cars are children forgotten in vehicles, according to Walston. She said children can be forgotten when routines are broken, and leaving something like keys, a cellphone or a briefcase in the backseat next to the child or setting an alarm on your phone are extra safety measures one can take to ensure the child is not left in the car.
Walston encouraged attendees to call 911 if they ever see a child, senior or pet alone in a call.
“This is something parents really need to take seriously,” said North Carolina Insurance Commissioner Mike Causey. “It’s year-round, not necessarily just during the hottest months of the summer. We have had children die in November and other months outside of June, July and August.”

Keeping patients safe while they receive high-quality compassionate care is at the heart of what ECU Health does for eastern North Carolina. This is especially important to Dr. Teresa Anderson, ECU Health’s senior vice president for Quality, who recently celebrated her induction into the East Carolina University (ECU) College of Nursing Hall of Fame.
She joins a number of colleagues, mentors, friends and former classmates in the Hall of Fame, which recognizes the accomplishments of ECU’s exemplary nursing graduates and faculty members.
When Dr. Anderson enrolled at ECU, nursing school was not the path she thought she’d take. She started out in education but after a semester of tutoring, she realized it was not her passion. She started on her nursing course work and never turned back.
“I always had a heart of service,” she said. “Then I got into nursing school and on we went. I actually started at [ECU Health] Medical Center in 1996 as a nursing assistant while I was in nursing school. I hit 28 years of service this May.”

Over those 28 years, Dr. Anderson has worn many different hats. From the nursing assistant role to a bedside nurse and working in various medical roles before taking on management and administration, she believes her varied experiences have helped her be successful in her current role in Quality.
Along with the variety of her work and the mentors she has learned from, Dr. Anderson said it’s the patients and ECU Health’s commitment to improving the health and well-being of eastern North Carolina that keeps her coming back each day.
“Our mission and the population that we serve are special and important to me,” Dr. Anderson said. “We serve a very complex population. I know that we’re doing so much good for our patients and our community, and there’s so much more we can do now alongside the Brody School of Medicine. There’s just going to be so much more that we can do with population health and making sure that people get all the services and access to care that they need.”
Dr. Anderson is a three-time ECU graduate with her bachelor’s, master’s and doctorate degrees from the university. She’s also been recognized as a Great 100 nurse in 2016 and received a Leadership DAISY Award in February of 2021.
Dr. Amy Campbell, a quality nurse specialist at ECU Health and an ECU College of Nursing Hall of Fame inductee last year, submitted the nomination for Dr. Anderson to be admitted to the Hall of Fame. In the nomination, Campbell noted that Dr. Anderson is an outstanding role model and mentor who influences positive change while recognizing her team’s accomplishments.
“Over the years, she has served in many leadership and administrative roles that have led to improvements in patient outcomes. In addition, she has served on numerous community boards and enhanced the lives of Pitt County Residents,” Campbell wrote in her nomination. “On a personal note, Teresa has been a mentor to me personally and professionally over the last 14 years. She encouraged me to go back to school of my Ph.D. and was an active member of my dissertation committee. She has walked with me through tough times and give me priceless feedback to help me grow. I cannot think of anyone more deserving of this award.”
Dr. Anderson said she was humbled and grateful to have been nominated and accepted into the Hall of Fame. Hall of Fame members, new and former winners along with family and friends, attended a ceremony and had their nomination letters read before they were presented with a plaque to honor their induction.
Members of the Hall of Fame help fund a scholarship for the next generation of nurses and Dr. Anderson said this was one of the most special parts of the recognition for her.
“They showed a video from one of the recipients of the scholarship money at the event,” Dr. Anderson said. “She talked about how much it meant to her and it was very nice to know that the money collected goes to a great cause and to fund students in need. She talked about making ends meet and paying rent and all of her work in school. I remember those days, so it feels great to give back to future nurses.”
Resources
Greenville, N.C. – ECU Health is partnering with Food Lion Feeds, Sodexo and the ECU Health Foundation to provide free meals for kids, teens and people with disabilities as part of the Summer Meal Program. Meals will be available in Greenville, Bethel and Ahoskie. The selected sites this year were chosen based on the need in each county, existing partnerships and the social vulnerability index at each location.
During the school year, many kids and teens receive free or reduced-price meals. When schools close for the summer, those meals disappear, leaving families to choose between putting the next meal on the table or paying for other necessities like utilities or medical care. While over 57% of students in North Carolina receive free or reduced lunch, 66% of Pitt County students and over 90% of Hertford County students receive free or reduced lunch.
Meals will be available until food runs out each day at the following locations:

- Greenville: English Chapel Free Will Baptist Church – 11:30 a.m. to 1 p.m., Monday-Friday from June 10 to Aug. 23. The location will be closed July 22-26.
- Ahoskie: Calvary Missionary Baptist Church – 11:30 a.m. to 1 p.m., Monday-Friday from June 10 to Aug. 23. The location will be closed June 19 and July 4-5.
- Bethel: Bethel Youth Activity Center – 11:30 a.m. to 1 p.m., Monday-Thursday from June 17-July 17. The location will be closed July 3-7.
ECU Health has offered the Summer Meal Program since 2021, providing nearly 12,000 free meals to kids and teens during the summer months. In 2023, 51 ECU Health team members served more than 2,800 meals to kids in need.
No registration is required. For more information about the ECU Health Summer Meal Program, please email [email protected].
Greenville, N.C. – Project SEARCH, an educational program offered at ECU Health Medical Center, is proud to announce nine students recently graduated from the program: Camarion Allred, Jordan Bell, Kevin Caudle, Caitlyn Ferry, Region Jenkins, Nicholas Tripp, Xavier Vaughan-Holliday, Eric Williams and Maxwell Wilson. Project SEARCH is a one-year internship program for students with developmental and intellectual disabilities during their last year of high school with the goal of providing real-world practical skills and increasing the chances of competitive employment.
“ECU Health is very proud to host Project SEARCH to bring educational opportunities to everyone in the East,” said Doris Hill, Project SEARCH coordinator at ECU Health. “This program gives students the opportunity to learn job skills that can be applied after graduation and brings diversity to our organization and the local workforce. We are proud of the tremendous growth of our nine graduates throughout the program, and we are all very proud of their accomplishments.”

The Project SEARCH program at ECU Health Medical Center began in 2015 through partnerships with Pitt County Schools, RHA Health Services and the North Carolina Division of Vocational Rehabilitation Services. Students complete internships in various departments at the hospital, including the ECHO Lab, Endoscopy Center, Environmental Services, SurgiCenter, hospital cafeterias, Hospitality and the Neuroscience Intermediate Unit.
“Project SEARCH gives our students support to transition into the workforce through skills development and a customized job search in the second half of the program,” said Katie Houmard, Project SEARCH instructor. “This program grows confidence and independence in all our students, and many of our graduates have gained competitive employment in our community. I am so proud of all our students and am excited to see them continue to grow and become employed.”
The employment rate for youth with disabilities is about 60 to 70 percent less than youth without disabilities, according to the Office of Disability Employment Policy. Project SEARCH has proven results with a 65 percent employment and 90 percent retention rate nationally.
Students who participate in the program are enrolled at various Pitt County high schools including J.H. Rose, D.H. Conley, South Central, Farmville Central, North Pitt and Ayden-Grifton. This is the ninth graduating class.
The Project SEARCH program began in 1996 at Cincinnati Children’s Hospital Medical Center (CCHMC) and was developed as a means to meet entry-level employment needs at CCHMC, support their diversity initiative and partner with schools and community services agencies. Project SEARCH is now an international program with over 716 program sites in 48 states and 11 countries.