ECU Health leaders, in association with Triangle Healthcare Executives’ Forum of North Carolina, recently hosted a C-Suite Round Table to discuss everything from workforce development to artificial intelligence in health care.
ECU Health Chief Operating Officer Brian Floyd, Chief Clinical Officer and Chief Quality Officer Dr. Niti Armistead, Chief Nursing Executive Trish Baise and Chief Strategy Officer Todd Hickey served on the panel for the discussion while ECU Health Beaufort Hospital President Dennis Campbell II moderated the event.
Floyd said the COVID-19 pandemic and the years that have followed created many financial challenges in health care, especially for rural hospitals and health systems like ECU Health, which already operated on thin margins.
“Most things cost less to operate in a more rural environment, except health care,” Floyd said. “By the sheer nature of us having to spread our resources so far around communities that are less densely populated, we are perfectly designed to cost more to operate than a health system of similar size in an urban environment.”

He said these circumstances made the ECU Health system come together to design improvements that help create efficiencies within the system to better serve team members, patients and families.
Talent and workforce development is a key piece to creating a more sustainable model of delivering health care in a rural community like eastern North Carolina. Baise said it’s been crucial to connect with team members and potential team members in different ways to recruit and develop high-quality nurses for the region.
“When we’re looking at cost savings, recruitment and internal programs to develop team members is a big part of that. We’re constantly evolving and looking at things differently,” Baise said. “We’re not a large metropolitan area, we don’t have significant population growth so we have to grow our own. That means academic partnerships, ensuring that we’re creating an environment that the students we’re working with will appreciate. On the back end, that also means making investments in our nurses.”
She said at the height of nurses leaving health care across the country, ECU Health experienced a 23% turnover rate of registered nurses. Thanks to the investment the system has made in nursing, the turnover rate is down to 12.6%. The investment from the system in nursing, Baise said, has gone beyond a financial investment but also includes capturing the voice of nurses, professional development and overall culture improvement.
Innovation has been a hallmark of the ECU Health story. Dr. Armistead noted that when the health system re-branded to ECU Health on Jan. 1, 2022, health care was in the midst of the Omicron variant surge from the pandemic. Dr. Armistead noted this was the most difficult month of the pandemic, one that took a toll on the health care workers tasked with treating large volumes of critically ill patients.
Through this, though, Dr. Armistead said the system has grown into an exciting, vibrant place with positivity that’s working to improve the health and well-being of eastern North Carolina.
“Aligned with our mission, we’re very community focused,” Dr. Armistead said. “That’s how we got through the pandemic, was with very strong community partnerships. Now, we’re shifting the focus of those partnerships to deal with our other challenge, which is the heavy burden of chronic disease in the region. We’re being very tactical and I’m so proud of what we’re able to do as ECU Health.”
Hickey said the work that he is most proud of is the health system’s outreach to the vulnerable populations in the 29-county region ECU Health serves.
In an area with a myriad of challenges in social determinants of health – highlighted by the fact that 21 of the 29 counties ECU Health serves are considered Tier 1 counties on the social vulnerabilities index – Hickey said partnerships make all the difference in making connections and helping community members access health care.

“Understanding that the biggest indicator of health outcomes is transportation, being able to get to an appointment, access to food, those things that we know have a much greater impact on someone’s health and health status is crucial,” Hickey said. “So we put a system in place in our community hospitals and we deliver on the promise of ensuring that we are meeting our patients where they are. I really think COVID helped drive that home in a different way, too.”
Hickey also said initiatives like the Community Health Needs Assessment are important avenues for patients to provide feedback to the health system.
The Round Table brought together leaders from around the state to hear from ECU Health and gain insight on how they are looking at shaping the future of rural health care in eastern North Carolina.
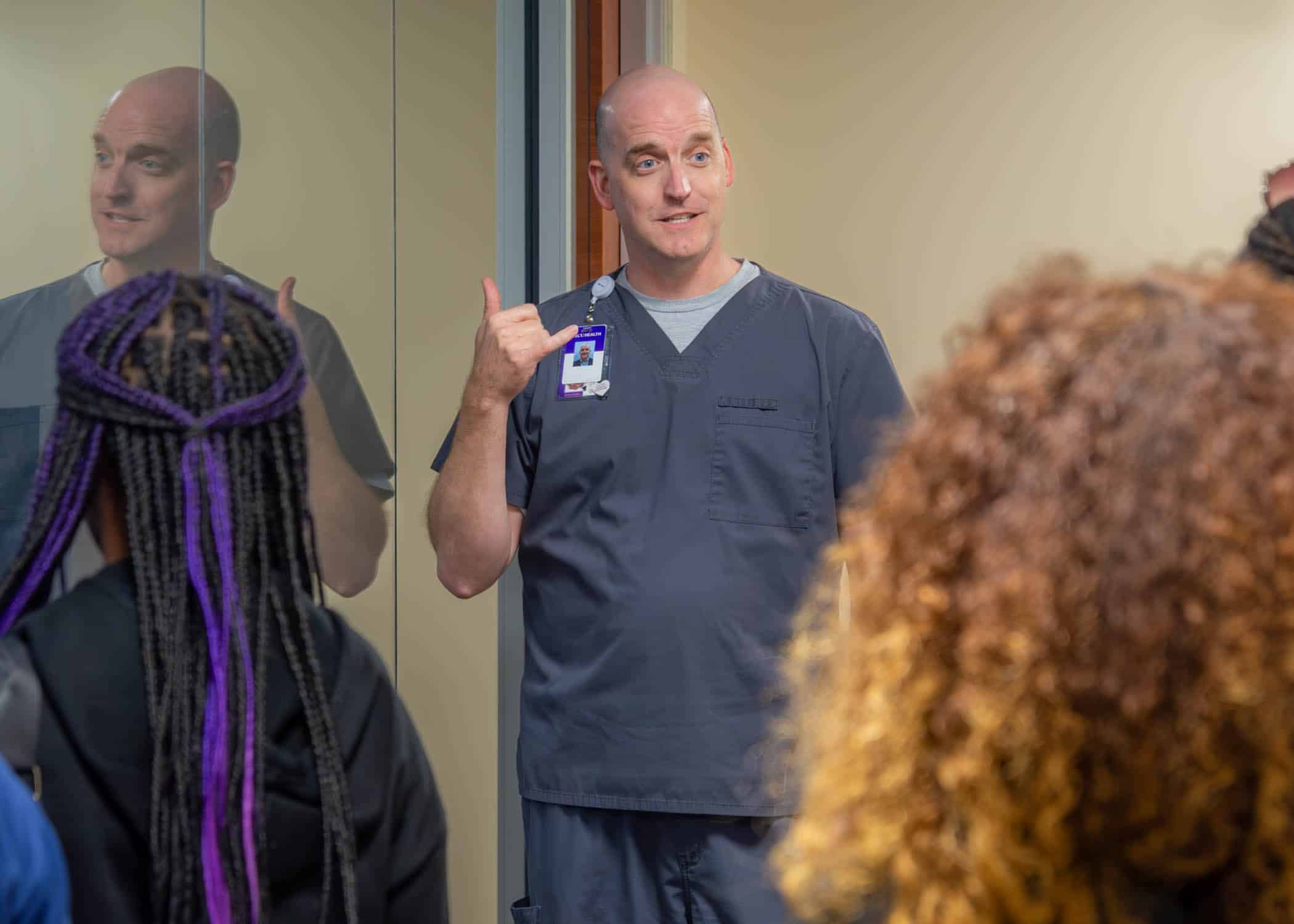
Recently, local middle school students had the opportunity to visit ECU Health Medical Center and learn about careers in the health care industry.
Grow Local, sponsored by Greenville-Pitt County Chamber of Commerce, started in 2018 and is designed to create and unveil career interests, grow the talent pipeline, and connect local businesses to future team members, according to the Chamber.
During the students’ trip to the Medical Center, they visited pharmacies and clinical labs across the hospital, took a tour of the Operations Center, and learned about the role of Organization and Leadership Development.
Nancy Turner, workforce development consultant at ECU Health, said connecting with local students is crucial to let them know of career opportunities available across the health system.

“These events are fantastic for a number of reasons,” Turner said. “For students that aren’t sure of what career path they might be interested in, it’s an opportunity to introduce a new idea and give them some options. For those interested in a career in health care, it’s a chance for us to make that connection for them early. We’re just grateful to have such great community partnerships that allow us to have these opportunities.”
In the Cancer Care Laboratory, students had a chance for a hands-on learning experience as they worked on putting together mock IV medication bags. Laboratory team members walked the students through the process and helped show them a bit of what they do on a daily basis.
Turner said it was exciting to see the students engaging with team members and learning how different team members help patients heal.
“These are things they’re not going to see every day,” Turner said. “It’s a really unique experience to talk to a lab technician, see them in their environment and get to try out part of their job. Having team members willing to take time out of their day and pour into our next generation of the workforce for a few minutes might not seem like much but it could create a passion and career path for a student.”
Another set of students headed to the Operations Center at ECU Health Medical Center, where they learned about the many career options supported throughout the health system, whether at the bedside or out in the community. From Nursing and Pharmacy to Information Technology, Food and Nutrition Services, and more, ECU Health supports community members from a variety of careers.
In the Operations Center, Jacob Parrish, vice president of Capacity and Throughput at ECU Health Medical Center, showed students how a team manages patient movement through a 974-bed hospital.
“As someone who is non-clinical, I think it’s great to show the students that there are careers that are super important to running a hospital that aren’t directly patient facing,” Parrish said. “I think it’s vital to help develop that next generation of folks who are going to serve eastern North Carolina, whether it’s as a care team member or as a support team member. I’m just glad to be a part of this event and if we helped one student realize that they may be interested in a career in health care today, then that’s a great thing.”
Resources
While the East Carolina University (ECU) baseball team is rounding into form as postseason play nears, they’re also taking time out to make a special difference in their community.
After a visit to ECU Health Medical Center last November, as part of a career shadowing opportunity, senior first baseman Carter Cunningham felt compelled to do something to help patients and families.
“I’d been praying for ways to give back to the community,” Cunningham said. “As we’re doing a tour of the entire campus, we walked into the [Maynard] Children’s Hospital and it was like God had smacked me in the face. It was like, this is what I have to do. I didn’t know what it would look like yet, though.”
He said that week, he went back to the team and asked for a small donation from everyone to spread some holiday cheer to patients and families at the children’s hospital. The response was more than he expected.

“We got about $500 and we were able to drop off some presents to the children’s hospital right before break,” he said. “It was awesome. We had about 20 players come in and we hung out in the playroom and had a great time.”
Tara Tadlock, a child life specialist at Maynard Children’s Hospital, said patients and families would subsequently talk about the visit for the next month. The same held true for Cunningham and his teammates, who also went on talking about how special the visit felt.
He said over the Christmas break he took more time to think about what he could do to make an impact for patients and families like those he’d met a few weeks before. Then the idea to start a foundation, Homers That Help, came to him.
It started with a call for donations on social media, one sponsor for each of ECU’s 33 home baseball games in 2024. The sponsor makes an up-front donation to the fund and an additional donation for each home run hit during the game. While he expected to need some time and make some calls to fill every game, the fund was complete after about 15 hours.
“The community here, I can’t describe it,” Cunningham said. “I get goosebumps talking about it because they’re so generous and so supportive, not only of ECU athletics, but the whole community. It was a testament to all the people that are here and I’m thankful and blessed to have an opportunity to be here.”
Because of the outpouring of support, Cunningham opened a “Fund B” for those who were not able to directly sponsor a game but still wanted make a donation. Cunningham is making donations himself as well, contributing $25 to the fund for each of his own home runs. With nine home runs, Cunningham is tied for the team lead and backing up his own efforts.
Along with the funds, which Cunningham and Tadlock recently started to distribute to patients and families, Cunningham and his teammates are continuing to make bi-weekly visits to the Maynard Children’s Hospital. He said taking a step back to give time to others is important to him.
“As a Division I athlete, you get so caught up in the games and practices, the wins, the losses, but every other Monday it’s just eye-opening,” he said. “I’ll never forget one patient, the day before we went to play Campbell, he said, ‘Have fun at your game tomorrow.’ It was so refreshing and offered great perspective. It’s way bigger than baseball. These visits are the best part of my week every time I visit.”
Tadlock said the program has been a great benefit for everyone involved and she’s looking forward to its continued success.

“I’ve been doing this for a long time with scheduling our visitors and working in Child Life and these visits are a bright spot of our month, too. It’s great to see the patients and families so excited, seeing the guys so excited and knowing that they’re making a difference for our patients is huge,” Tadlock said. “Some of the kids that are here are going through really hard stuff and finding out hard news. If they’re able to leave that behind for a few minutes and hang out with the ECU baseball team, it’s really important to try to create those special moments. All we want to do in Child Life is provide some normal experiences for the children. Working with this team has been amazing.”
Though this is Cunningham’s last year at ECU, he said the plan is for Homers That Help to carry on. He’s looking to younger members of the team to pick up the torch and build upon the positive momentum the foundation has today.
Resources
Greenville, N.C. – ECU Health is seeking feedback from community members throughout eastern North Carolina on its current Community Health Needs Assessment (CHNA). The feedback from the CHNA allows the health system to understand what community members see as the most important health issues affecting their communities.
Every three years, ECU Health conducts this comprehensive assessment to provide the foundation for improving and promoting good health in eastern North Carolina region. By soliciting feedback directly from the community, ECU Health can better tailor efforts to promote wellness and address critical health challenges.
ECU Health encourages all community members age 15 and older to complete the CHNA survey and provide meaningful feedback on how ECU Health can continue to improve health and well-being in eastern North Carolina.

The survey takes approximately 10 minutes to complete and all responses are confidential. Your feedback helps ensure health care needs are met in the 29 counties ECU Health serves. The survey is open through June 7, 2024.
The CHNA process involves comprehensive data collection and analysis, including demographic, socioeconomic, and health-related statistics. However, the most valuable insights come directly from community members themselves. The completed CHNA analysis and results serve as the basis for prioritizing strategies to meet the community’s health needs in order to improve the health and well-being of eastern North Carolina.
The survey is in both English and Spanish and can be found at ECUHealth.org/CHNA.
The American Association of Cardiovascular and Pulmonary Rehabilitation’s (AACVPR) Day on the Hill, which was March 4-5 this year, is an opportunity for cardiac and pulmonary rehabilitation professionals to visit Washington, D.C. to advocate for their profession and ask legislators for support for beneficial legislation on Medicare decisions. It was Stacey Greenway’s 10th year participating in this event, a milestone made all the more significant by her recent election as treasurer to the AACVPR board.
Stacey, the director of cardiovascular disease management services at ECU Health Medical Center, wasn’t initially interested in health care policy, but her zeal for her work inspired her to get involved.
“I’m passionate about what I do, and when I realized the impact these legislative decisions make on our patients, I wanted to get involved,” she said. “When the North Carolina Cardiopulmonary Rehabilitation Association (NCCRA), which works on the state level, asked if anyone was interested in participating in Day on the Hill, I thought how cool it would be to help our patients and our programs. After the first time, I was hooked.”

Each year, the AACVPR’s legislative priorities are different, but the goal is the same. “We want to help the legislators see things from the patient perspective and put a face to the people these bills are affecting,” Stacey said. “From that angle, you see the increase in a patient’s quality of life. From a health system perspective, it decreases the rates of hospital readmission. It’s a win-win.”
This year’s priorities centered on two bills: HR-955/S.1849, the Sustaining Outpatient Services Act, and HR-1406/S.3021, the Sustainable Cardiopulmonary Rehabilitation Services in the Home Act. The Sustaining Outpatient Services Act seeks to correct a legislative error from a previous bill that reduces reimbursement for cardiac and pulmonary rehabilitation services when they are provided in off-hospital campus clinics. The reduced reimbursement rate makes cardiac and pulmonary rehabilitation services financially unsustainable and thus eliminates patient access to these resources, especially in rural communities. “Some rural hospitals, which don’t have a lot of real estate on campus, haven’t even tried to open a rehab clinic because of this issue,” Stacey said. This bill would establish an exemption status to certain hospital outpatient services, including cardiac and pulmonary rehabilitation, from that fee reduction.
The Sustainable Cardiopulmonary Rehabilitation Services in the Home Act would allow Medicare beneficiaries to receive cardiac or pulmonary rehabilitation services through real-time telehealth in their homes. This hybrid type of service was very successful during the pandemic, and it allowed more patients to be treated from across eastern North Carolina.
“Think of that 45-year-old patient who had a heart attack and would benefit from rehab services but has also been cleared to work and needs to make an income,” Stacey explained. “This bill would allow that patient to not have to make a choice between income and health; they could do both.”
During her time in Washington, D.C., Stacey and 74 other AACVPR members spoke with their respective House Representatives and Senators to advocate for these bills. Stacey said overall, the discussions were productive.
“I had some good conversations about both bills,” she said. “The telehealth bill was one the legislators could wrap their heads around easier; it was something they were familiar with. That was encouraging.” While more work needs to be done to increase support for the outpatient services bill, Stacey said she felt the needle moved a bit. “This is partly because the government seems to be changing their focus from thinking about the up-front costs of health care to the savings incurred on the back end,” Stacey said. “That means things are changing, and I’m hoping we’ll get a few more co-signatures on that bill.”
As a board member, Stacey said she now has other opportunities to support her profession.
“To represent eastern North Carolina and discuss at the national level some of the things that impact those who practice locally is really important,” she said. Because she was on the board this year, Stacey was also able join the board meeting the day before Day on the Hill and participate in the selection of a new legislative firm. “We met with the firm and prepped for Day on the Hill, but we also strategically planned for the future,” Stacey said. “It was exciting to be involved in that process.”
Stacey’s interest in running for the AACVPR’s treasurer position stemmed from her desire to stay involved in the national organization and escalating care for patients.
“The board is involved in regulatory and government relations, and that’s one of my big interests. Day on the Hill is just one way we stay involved. It’s a way of understanding and supporting initiatives and bringing that back to ECU Health,” she said. “We have six cardiac and pulmonary rehab programs within ECU Health, and I want to make sure those programs are aware of the initiatives the AACVPR promotes to escalate their practice and ensure we’re doing the best we can for our patients.”
Now that the initial conversations with Congress members are over, the next step is to follow up in a few weeks with those representatives still on the fence. “We’ll also bring in a constituent from that person’s district to speak to the impact of these bills,” Stacey said. Some representatives have already signed on to at least one of the bills, including Rep. Don Davis, Rep. Deborah Ross, Rep. Greg Murphy, Rep. Wiley Nickel and Rep. Jeff Jackson.

It’s important to be involved in the policy issues surrounding health care, Stacey said. “You don’t go into health care thinking about these operational or political issues, but when you’re faced with the repercussions in the clinic, you see the impact it has.”
She encouraged all health care professionals to get involved: “Let’s do this for the betterment of the patient experience,” she said. “For me, this has been one of the highlights of my professional life.”
As part of its commitment to growing a high-quality nursing workforce for the region, ECU Health recently held a New Graduate Nurse Hiring event to connect with upcoming nurses, many of whom will begin their career with the organization in a few months.
The two-day event was hosted at the TowneBank Tower and the Williams-Clark Club Level on East Carolina University’s campus.
The February hiring event featured 301 scheduled interviews with prospective nurses, many of whom are from right here in eastern North Carolina, allowing candidates to interview for various units and connect with nursing leaders within the organization. To date, 96 future nurses have accepted positions across the ECU Health system.
This event underscores ECU Health’s commitment to recruiting and retaining exceptional nurses as we continue to shape the future of rural health care.

“The New Graduate Nurse Hiring event was really a great turnout,” said Trish Baise, chief nursing executive, ECU Health. “The opportunity to connect with future nurses was priceless. It was beneficial to engage in a casual environment before interview day and it allowed our team to speak with them informally. Every year it gets better. New graduate nurses are an important part of our workforce pipeline. It’s important for us to make sure that those who have grown up in eastern North Carolina and/or have been educated here, have a wonderful clinical experience with us.”
The hiring event spanned two days, with Friday dedicated to networking and allowing candidates to interact with recruiters and nursing leaders from several ECU Health entities, and Saturday dedicated to interviews.
“The key message that resonated well with the nursing candidates was ECU Health is the land of opportunities,” said Dr. Kamilah Williams, administrator for Professional Practice Development & Clinical Education at ECU Health. “There are so many opportunities for launching nurses’ careers in every specialty of nursing practice across ECU Health.”
If you’re interested in reading about our new graduates and their experience at ECU Health, check out the People of ECU Health articles on Brianna Cavaliere and Samantha Nichols.
“Jim will be very humble and tell you he was in the right place at the right time,” Dr. April Quidley, pharmacy supervisor, critical care/emergency medicine and PGY1 Pharmacy Residency Program director, said about Dr. Jim Worden’s impact on ECU Health and in his community.
Dr. Worden retired on March 22 after working for ECU Health for 41 years. During his retirement reception, however, he was surprised to learn he’d also won the Order of the Long Leaf Pine award, the highest honor North Carolina’s Governor can bestow on a person for their contributions to the state.
Dr. Worden, a Tennessee native, moved to Greenville, North Carolina for his first job out of his pharmacy residency to work as a clinical coordinator. “I’ve been here [at ECU Health] since August of 1983,” Dr. Worden said. During that time, he held a few different roles, including assistant director of clinical services, the director of pharmacy and most recently, the systems service line administrator for pharmacy.
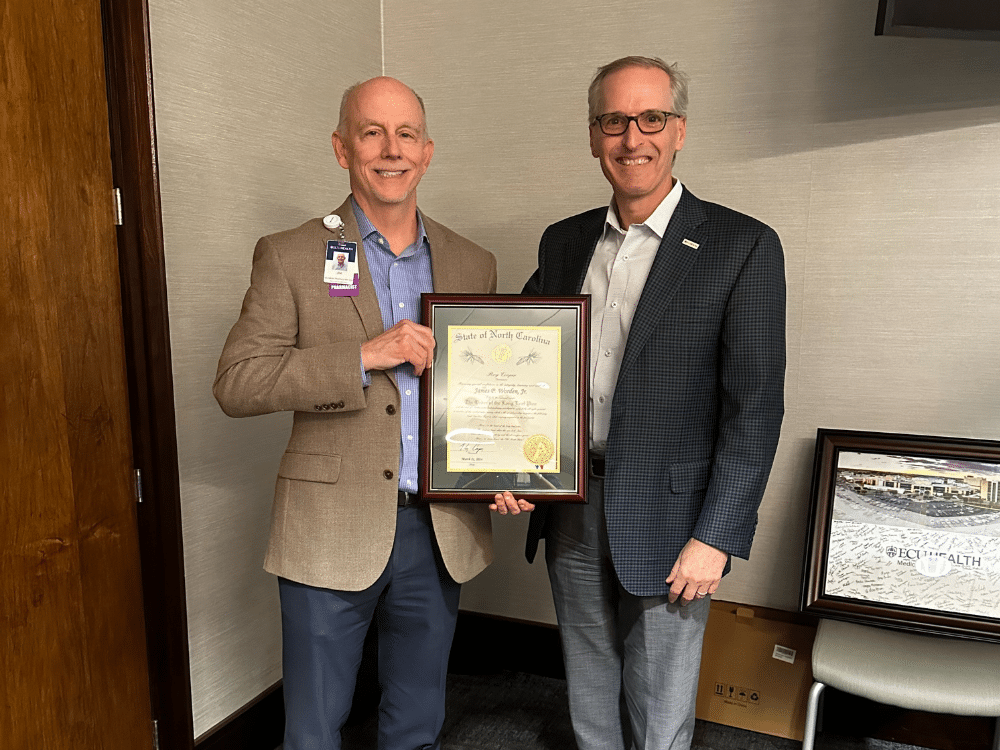
During that time, Dr. Worden was instrumental in setting up ECU Health’s pharmacy services by “working closely with physicians in a direct, bedside patient care role” and by founding the Drug Information Center, which, according to Dr. Worden’s award nomination documents, “served as a resource for all health disciplines in eastern North Carolina in the time that evidence-based medical practice expanded.”
“When we think about pharmacy services at ECU Health, Jim is the guy who gets all the credit,” Dr. Quidley said. “He worked hard to form those interdisciplinary relationships with physicians and to advocate for patients. He is the founding director of our residency program, the Pharmacy Practice Residency, which is one of the oldest in the country at 30 years old.”
He went on to develop additional pharmacy residency training programs for critical care, emergency medicine and infectious diseases. “He’s been on the cutting edge of everything we do in pharmacy,” Dr. Quidley said. “He’s done exceptional things for the department.”
As a result of his dedication, ECU Health’s services represent a leading practice in pharmacy care, especially for a rural region, and he’s helped expand services to improve the medical and pharmacy care across all of eastern North Carolina.
On March 22, a retirement reception was held to celebrate Dr. Worden’s more than four decades of service. Little did he know, however, that there was an ulterior motive to the event. “We surprised him with the Long Leaf Pine award at the event,” Dr. Quidley said. “Dr. Mike Waldrum, Dr. Herb Garrison – also a recipient of the award – and Brian Floyd were there to present the award to Jim, and it was a great surprise.”
The Order of the Long Leaf Pine award is among the most prestigious awards conferred by the Governor of North Carolina, and it is awarded to persons for exemplary service to the state and their communities, going above and beyond the call of duty and making a significant impact on and strengthened North Carolina. Nominations can be made for retiring individuals who have 30 or more years of service in North Carolina, and nominations must include documents that attest to the person’s work and service, supported further by letters of recommendation.
Dr. Worden said he knew of the award, but he didn’t think he was the sort of person to win it. “It’s an impressive, austere award, but I didn’t think I’d done anything in my life that was at the level to win it. I was humbled to be considered for something that noble.”
Dr. Quidley and those who wrote supporting letters of recommendation think differently. Dr. Worden has made a significant impact not only at ECU Health, but also in his community. He is on the Board of Directors for the Community Crossroads Center, which is the only emergency homeless shelter in Greenville and Pitt County. He joined the board three years ago after a fellow church member let him know a position was opening.
“I felt like my conscience told me I should apply, that God was calling me to help, so I applied, and they voted me in,” Dr. Worden said.
In the past year, he worked with ECU Brody School of Medicine to restore medical services for residents of the shelter. For his dedication to the board and the shelter, the board elected Dr. Worden to be president next year. He is also actively engaged in Greenville’s First Presbyterian Church, where he has in the past served as the Chair of the Missions Ministry, Chair of the Worship Ministry, a member of the Stewardship committee and twice as an elder on the Session, the church’s governing body.
“I’m very committed to my church,” Dr. Worden said. He plans to continue that service now that he’s retired. “I’m going to enjoy time away from work, but I won’t be sitting around. I will of course be the president of the shelter’s board, and we will have activities that will keep me busy. I will continue to work in my church, and I hope to play some tennis and pickleball.”

Dr. Worden also plans to travel with his wife of 34 years, Tammy, who is also a pharmacist at ECU Health and who helped Dr. Quidley nominate Dr. Worden for the Long Leaf Pine award. “When you’ve been married to someone that long, it is an accomplishment – you need that person and they need you,” he said.
As Dr. Quidley predicted, Dr. Worden remained humble about his contributions to ECU Health and beyond.
“This is not about me,” Dr. Worden said of winning the award. “I’ve started some good things, and I’ve been fortunate to have the resources, teamwork and leadership to do these things, but it really does take a village. I will take credit for some of it, but a leader can only do so much by themselves.”
Tanya Graham, a North Carolina native and Greenville resident, was outside cutting her grass when she started to feel very tired. That night, she experienced what felt like an asthma attack, so the next day she visited an urgent care clinic. “I do have asthma,” Graham shared, “but I’ve never had an attack.” The doctor ran a few more tests, and after an EKG, he decided to send Graham to the hospital.
“The cardiologist at [ECU Health] Medical Center said, ‘You are in heart failure,'” Graham said. “I didn’t know what he was saying, I was so shocked.”
Dr. W. Douglas Boyd, a cardiothoracic surgeon, told Graham she needed surgery, and two weeks later, Graham found herself back in the hospital recovering from a double coronary bypass. She was told later that her initial ejection fraction, which is the amount of blood your heart pumps each time it beats, had been 10 percent. A normal ejection fraction is 50 percent or higher. “After the surgery, they did another echocardiogram, and now it’s up to 35 percent,” Graham said.

Graham knew that once she was strong enough after the surgery, she wanted to participate in cardiac rehabilitation. She had heard about the option from her neighbor, who also had recently suffered a heart attack. “I also have two sisters who are nurses,” Graham shared. “One of them works for a cardiologist, so I talked with her about cardiac rehab, and all of my siblings agreed it was a good idea.”
Cardiac rehabilitation focuses on the “what now” after a cardiac event. Stacey Greenway, the director for cardiovascular disease management services at the Medical Center, hopes that cardiac rehab will become the immediate program associated with cardiac recovery.
“A multidisciplinary team works with the patients to establish and achieve goals to improve their health, quality of life and functional ability,” Greenway said. “We develop individualized treatment plans for each patient that includes exercise, nutrition, medications, stress management and other components.”
For Graham, therapy started slow, but she said she immediately felt comfortable. “The team is so smart, and they are in tune with each individual person,” Graham said. “It made a huge difference because I learned right off that I could trust them. It made me want to go.”
It also helped to have others around her going through the same experience. “It didn’t matter if they were a man or woman or what race they were – we were all there for the same reason. Our bodies had broken in some way, and we were all there together for the same purpose of trying to survive and extend our lives,” Graham said. “I drew strength from them, because when I saw them working hard, it made me want to do the same.”
The experience didn’t just provide Graham with the chance to get stronger after a major surgery. “The one thing I came away with,” Graham said, “is hope. Hope that I’d live a longer life.” Graham said that it wasn’t just the exercise that encouraged her and helped her get better; it was also the classes they offered. “I learned quite a bit from the classes, which covered things like diet and coping with this diagnosis,” she said. Something Graham didn’t expect was having access to support from a therapist. “I’d had a hard experience with my surgery, so they put me in contact with Dr. Kari Kirian, and she worked wonders. I can’t say enough positive things about that experience.” Dr. Kirian is a cardiac psychologist embedded in the heart failure program – a critical member of the care team as it is not uncommon for patients to experience anxiety or depression after a cardiac event.
While she wished she could have participated for longer, Graham graduated from cardiac rehab with the ability to do the things she needs to do. “It allowed me to come home and do the things you take for granted, like clean the house or roll your hair,” Graham said. She also immediately joined a gym and signed up for personal training to continue her progress. “I left cardiac rehab on a Friday, and that following Monday I was at the gym,” Graham said. “It wasn’t mandated, but the cardiac rehab team provided me with information. My sister goes to a gym, so I decided to go there, and now I go every weekday. I will continue to exercise, think positive and eat right.”
Because she’s feeling so much better, Graham said she has plans for the future. “I’m going to work on making one of my bedrooms a storage space, and in the spring, I plan to paint a shed in the back yard,” Graham said. She also hopes to visit her daughter and grandchildren in Phoenix, Arizona next winter. In the meantime, Graham said she’s cleared it with her doctors to serve as a volunteer in the cardiac rehab unit. It’s one way she can share her experience and give back to the amazing Cardiac Rehab team for impacting her life in an incredible way.
“I don’t care what I do. I just didn’t want to leave there,” Graham said. “I love people, and I thought maybe if I was around people going through what I went through, I could tell them my story and help them.”
The Eastern Carolina Injury Prevention Program (ECIPP) at ECU Health Medical Center partnered with volunteers from Greenville Police Department, ECU Health Police Department, Pitt County Sheriff’s Office, ECU Police Department, Pitt County Schools and nurses at ECU Health to fit 100 fourth and fifth graders at South Greenville Elementary School with bicycle helmets to encourage safe biking. Funding for the helmets was provided by Children’s Miracle Network and the North Carolina Department of Transportation.
“It is incredibly important for parents to ensure their children know how to safely ride their bikes including wearing a helmet, bright colors and reflectors, riding on the sidewalk or in the same direction as traffic and being aware of their surroundings,” said Ellen Walston, injury prevention coordinator, ECIPP, ECU Health. “Wearing a helmet is the best way to reduce head injuries, and we are incredibly grateful to our community partners including law enforcement officers and physical education teachers that are willing to teach bike safety to their students.”
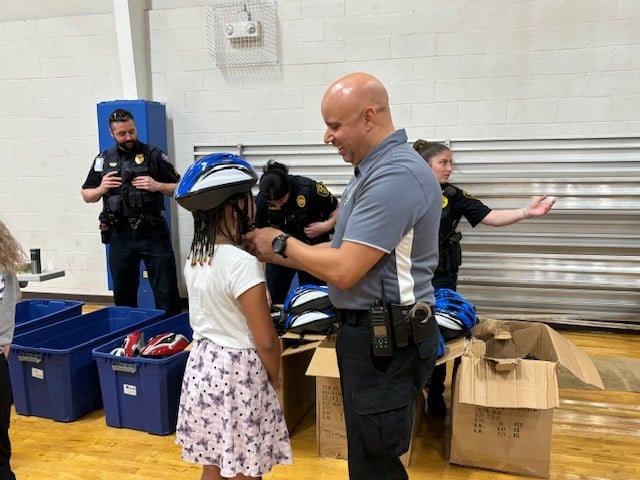
According to Safe Kids, properly fitted helmets can reduce the risk of head injuries by at least 45 percent, yet less than half of children 14 and under usually wear a bike helmet. In 2020, there were 136,753 emergency department visits from children with bicycle-related injuries across the country. ECIPP aims to reduce the number of children harmed in eastern North Carolina and beyond by encouraging safe bicycling practices and ensuring local children have access to helmets. These partnerships not only facilitate the distribution of helmets but also enable law enforcement officers to engage directly with children, emphasizing the importance of wearing helmets and adhering to traffic regulations while biking.
“While ECIPP may provide the logistical and often the boots-on-the-ground operations, none of our work would be possible without the strong partnerships that we have with our schools, law enforcement and many others throughout the region,” said Sue Anne Pilgreen, manager, ECIPP, ECU Health.
Haley Behm was completing one of her first rotations in the Brody School of Medicine at East Carolina University at an outpatient clinic when Cleve Smith showed up for a routine check-up with his father, Emmett Smith. Cleve, a wheelchair user, has seen his fair share of medical students come through the clinic throughout his visits over the years but this was his first time working with Behm.
As a medical student with limited patient interactions, Behm was nervous about how she would connect with one of her first real patients, let alone her first patient with a disability. But when she met a lighthearted, humorous father-son duo in the patient room, she felt a little more at-ease.
“I was running through a depression and anxiety screening, and I got to a question where it asked ‘Have you ever been so restless you couldn’t sit still?’” Behm recalled. “I felt so bad even having to ask him that question.”
A question that Behm initially dreaded having to ask turned in to the start of a punchline for Cleve and Emmett, and it’s one they’ve practiced more than once.

“Haley has been really sweet, and I haven’t forgotten her since the first time we met,” said Cleve. “I could see that question really bothered her because I laughed and she didn’t immediately. So I wanted to assure her everything was fine.”
Added Emmett, “Through the years we have met many medical students at the clinic, and the one I remember is Haley. She had such a kind, caring demeanor. She really cared about Cleve’s feelings and what she could do to help him.”
Behm’s connection with the Smiths was just one of the powerful stories shared at ECU Health and Brody’s fifth annual Legacy Teachers Celebration on April 5. At the Legacy Teachers Celebration, third-year medical students share their experiences in the forms of short stories, poems or videos that honors patients who taught them valuable lessons – the type that can’t be learned in the classroom but can last a lifetime. The event also provides an opportunity for students to reunite with their Legacy Teachers and honor the special connection.
“The stories we hear at the Legacy Teachers Celebration are really emblematic of the types of experiences our students have here at the Brody School of Medicine and ECU Health,” said Dr. Jason Higginson, executive dean, Brody. “Medical students learn so much important information in the classroom and on clinical rotations, but sometimes the most impactful lessons they learn come from those they have the honor of caring for. It’s so gratifying to see our students reconnect with the patients who left a lasting impact on their journey toward becoming a physician.”
For Behm, her experience with the Cleve and Emmett gave her a different perspective on her role as a patient advocate, especially for patients with disabilities who may face difficulties accessing the care they need.
“Patients with disabilities have various accessibility needs, which may not be evident before a visit. It is important to be flexible and modify plans, exams and surroundings,” said Behm.
In total, 22 medical students shared their stories at the Legacy Teachers Celebration, which featured gift baskets, a photo station, lapel pins and remarks from ECU Health and Brody leaders – all designed to create a memorable experience for students and their legacy teachers.
Dr. Michael Waldrum, CEO of ECU Health and dean of Brody, provided remarks at the celebration along with Dr. Higginson. Like the students, they shared their deeply personal stories of important lessons they learned as students.
The speakers shared common themes around the importance of positive, trusting relationships between patients and care teams.

“The relationship between a physician and a patient is a sacred one,” said Dr. Waldrum. “Each patient we interact with provides us an opportunity to reflect on who we are and why we do what we do. For these medical students, who are driven by their passion to make a lasting difference in the lives of others, this event provides them with an opportunity to reflect on the legacy teacher that made a difference in their educational experience.”
While Cleve, Behm and Emmett were able to reunite at Legacy Teachers and share their story and learn of other stories, Behm expressed how important the Legacy Teachers Celebration is to reflect on the lessons learned from patients.
“The biggest part of Legacy Teachers is I have something to learn from all of my patients,” Behm said. “And some make the lessons easier than others.”