Eight students in the Brody School of Medicine at East Carolina University have been named to the North Carolina Medical Society Kanof Institute of Physician Leadership’s 2024 Future Clinician Leaders College (FCLC).
Noor Baloch, Nolan Davis, Michael Denning, Charles Johnson, Hannah Rayala, Emmalee Todd, Ben Wise and Michael Wright will join students from other colleges and universities across the state who are interested in leadership and professional growth.
“The FCLC program provides us with a unique, structured ability to engage with our future colleagues on community-level projects that address the varied landscape of health, health equity and health care,” Denning said. “Gaining intense leadership training alongside other health professions students will allow me both introspection and outward reflection on my future role, as well as mechanisms to ensuring our patients are excellently and compassionately cared for.”

Prospective students are referred and nominated to the program by faculty, mentors and others at their respective colleges. The 2024 class includes 27 students representing disciplines including medicine and pharmacy from ECU, UNC Chapel Hill and Duke, Campbell, Wake Forest, Western Carolina and Wingate universities in North Carolina, as well as St. Georges University in Grenada.
FCLC is a partnership with North Carolina Area Health Education Centers (NC AHEC) to provide opportunities of leadership in an interprofessional health care environment and networking across institutions. The one-year program is designed to enhance health care experience through advocacy, change-driving and individual leadership skills.
Baloch said she wants to be a leader when it comes to ensuring proper care for her patients.
“I felt that in order to be the best leader I could be, I needed additional training alongside other health care professionals to really understand my role as a physician in a health care team as well as establish how I can best serve my patients in that way,” she said. “Through this program, I am able to understand my own leadership style as well as my faults so that I can work on them and ensure I am self-aware regarding how I lead interactions with my patients.”
The program emphasizes leading in interprofessional health care environments and networking across institutions. The interactive learning format encourages participants to engage with their peers and program leaders, faculty and speakers. They also participate in a project that gives them exposure to some of the major health policy challenges relevant to North Carolina.
“This is an incredible opportunity for these eight students to work with other interprofessional students across the state to develop the skills necessary to be a leader in health care tomorrow,” said Dr. Amanda Higginson, Brody’s associate dean for student affairs. “We know our Brody graduates go on to do amazing things; this wonderful program will further develop these students to both improve the health and well-being of the region, but also to augment the already great training they receive here to prepare them to become physicians who will meet the health care needs of the state, both critical mission goals of the school.”
The students will have hands-on experience cultivating leadership skills including team-leading, communication and career development.
“The purpose is to build leadership that centers on self-awareness and fosters authenticity that allows each student to act in alignment with their core values as a leader, encourage and assess information from different perspectives, and balance transparency,” according to the program website. “With the individual core as a foundation for leadership development, this course prepares students for the leadership journey, allowing the individual to establish a strong sense of purpose and understanding of who they want to be as a leader.”
Todd said the nature of medicine as a “team sport” necessitates the ability to collaborate with other health care professionals at any given time.
“In order to do this, it’s important to understand your own teamwork preferences and leadership style and be able to refine them to better suit your purposes,” they said. “I believe my participation in FCLC is providing me the opportunity to do exactly that, which will hopefully lay the groundwork for not just my own success in residency and beyond, but the success of the health care teams of which I will be part.”
Todd said the unique experience to explore a current health-related policy issue in North Carolina is valuable because it gives students a chance to propose potential solutions.
“So much of what impacts our patients’ health are factors that we can’t necessarily do anything about within a half-hour annual physical — their housing situation; the ease of their transportation to work or school; the accessibility of nutritious food, clean water and green space where they live,” they said. “Working towards policy change is one way that physicians can make an impact on these broader societal factors, and it’s something that I would like to be involved in throughout my career. FCLC is equipping me with the experience and skillset I need to begin to pursue this goal.”
Read more from ECU News Services.
Like many health care organizations across the nation, ECU Health is facing an immense challenge: solving the growing health care workforce shortage.
Through community partnerships, the health system is doing its part to grow its workforce, starting right here in eastern North Carolina.
More than 200 high school students from Pitt County, Duplin County and other surrounding communities spent the day learning about various rural health care career opportunities at ECU Health’s Health Sciences Academy career fair Tuesday, March 5.
The event featured 30 hospital departments and exhibitors from partners including Pitt Community College and Beaufort County Community College hosted interactive and creative booths to educate students on different health care careers.

“It is such a joy to host these students and to expose them to so many interesting and important health care career opportunities available to them right here in eastern North Carolina,” said Nancy Turner, workforce development program coordinator, ECU Health. “Our students are our future workforce at ECU Health and partnerships like this are essential to ensuring we can care for our region. There are so many exciting and fulfilling opportunities to make a difference right here in their community, and we hope that today served as inspiration for them as they make important decisions about their future.”
The career fair is another representation of ECU Health’s commitment to growing health care talent locally. Through the Health Sciences Academy, ECU Health partners with public schools to provide eastern North Carolina’s youth with the education and resources to pursue exciting and fulfilling futures in health care. During high school, Health Sciences Academy students complete a minimum of six courses that expose them to potential health care careers and prepare students to pursue college-level health science programs upon graduation. They participate in job shadowing, mentoring, internships, medical research opportunities, career exploration and volunteering.
The Pitt County Health Sciences Academy is a partnership between ECU Health, Pitt County Schools, Pitt Community College, East Carolina University, the Brody School of Medicine, Colleges of Allied Health Sciences, Engineering and Nursing at East Carolina University, School of Dental Medicine at East Carolina University, the Eastern Area Health Education Center and the Greenville-Pitt County Chamber of Commerce.
Resources




Greenville, N.C. – ECU Health Medical Center has been nationally recognized in Becker’s Hospital Review as the top hospital in the country for patient experience, according to a new ranking from PEP Health. PEP Health analyzed more than 30 million online patient reviews from hospitals across the country in 2023.
According to Becker’s, PEP Health extracts behavioral insights data from patient comments shared on multiple social media and review platforms. Hospitals with at least 300 staffed beds and at least 250 patient experience comments were assessed across seven domains: fast access, effective treatment, emotional support, communication & involvement, attention to physical and environmental needs, continuity of care, and billing and administration.

“At ECU Health, creating positive patient and team member experiences is at the heart of who we are as a mission-driven organization,” said Dr. Julie Kennedy Oehlert, chief experience officer, ECU Health. “Our continuous journey toward excellence in patient care is informed by the perspectives of our patients and driven by the hearts of our team members. Our patients know that ECU Health team members are here to care for them with compassion and respect. It is gratifying to know our intentional focus on creating safe, healing environments is affirmed by the feedback of those we are honored to serve. We are incredibly grateful to our patients for their honest review of the care we provide.”
ECU Health’s commitment to creating positive patient experiences can be seen across the health system. The Outer Banks Hospital achieved 5-star status in overall patient experience in 2023 and ECU Health Bertie Hospital met requirements for 5-star status as well from Centers for Medicare and Medicaid Services (CMS). The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) utilizes these star ratings to summarize the patient experience, which is one aspect of hospital quality. The ratings are based on surveys that patients fill out after their inpatient stay and are designed to help patients choose excellence in health care. The HCAHPS survey captures the patient’s experience of communication with doctors and nurses, responsiveness of hospital staff, communication about medicines, cleanliness and quietness of the hospital, discharge information, transition to post-hospital care and overall rating of the hospital.
ECU Health’s providers also play an important role in supporting excellence in patient experiences. In the clinic setting, 99% of ECU Health providers are rated by their patients as 4.0 or higher out of 5 stars, with 96% of those providers being 4.5 stars or higher, according to Press Ganey LLC. ECU Health’s providers’ overall ranking as a medical group for excellence in care is 4.7 out of 5 stars based on patient reviews from Healthgrades, Google, WebMD, Wellness, Vitals and more.
“I am proud of the doctors, nurses and all team members who work tirelessly to deliver highly-reliable, human-centered care to eastern North Carolina,” said Brian Floyd, chief operating officer, ECU Health. “The experiences we create within our health care settings can leave lasting impressions on those we serve. I am fortunate to witness ECU Health team members in action every single day, and their role in compassionately caring for our community members – often during their most difficult moments – is central to our mission of improving the health and well-being of eastern North Carolina.”
According to the Centers for Disease Control and Prevention, colorectal cancer is the fourth most common cancer, apart from some kinds of skin cancer.
While colorectal cancer is common, early detection and prevention can be lifesaving. Of those ages 50 to 75, only about 7 out of 10 adults in the United States are up to date with their colorectal cancer screenings. Screenings can be done in a variety of ways, some of which include colonoscopies and fecal testing. When cancer is detected through preventative screenings, treatments can begin earlier to increase the chance for positive outcomes.
No one knows the importance of screenings more so than Stephen Braddy.
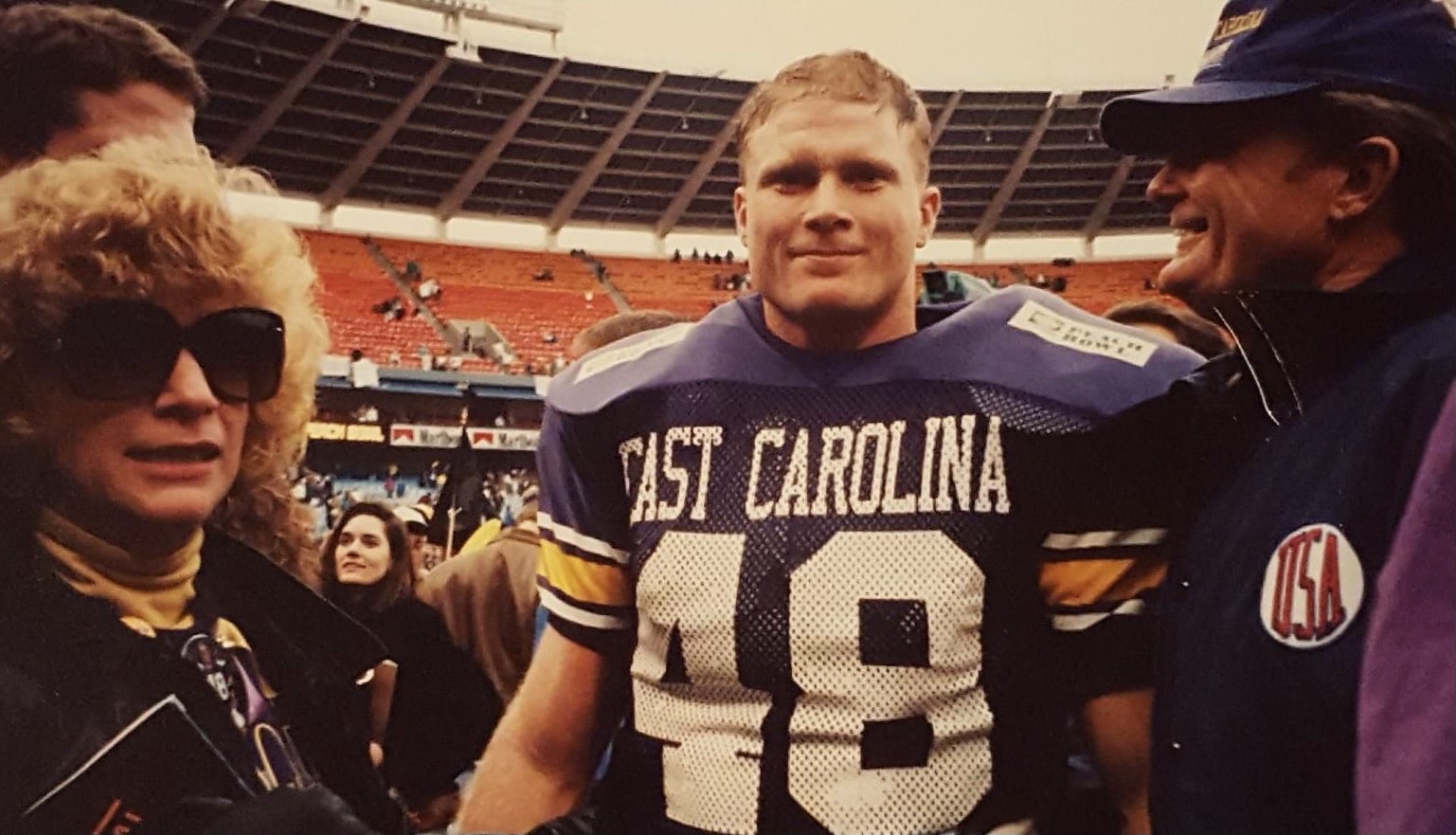
Braddy grew up in eastern North Carolina and played various high school sports before going on to East Carolina University to play football as a linebacker, even playing in the 1992 season that led the Pirates to the Peach Bowl. Now, Braddy is retired and works at Washington Montessori School. He also spends time advocating for the importance of colon cancer screenings.
This cause is important to him because in 2022, after encouragement from his family and friends, he scheduled a colonoscopy at ECU Health which led his doctors to discover a mass in his colon.
“I woke up from the procedure and the doctor comes in with this look on his face and says we’ve got some issues,” says Braddy. “We couldn’t finish the colonoscopy because there was a tumor the size of an egg in the way. I was immediately sent for blood work and scans.”
Braddy was quickly scheduled for surgery on July 12, 2022. During the surgery, doctors removed part of his colon, the mass and 19 lymph nodes, as well as did a colon resection. Following the surgery, he went through four sessions of IV chemotherapy with chemotherapy medication in between.
As a former college football player, Braddy has always been an active person, and he wasn’t going to let treatment keep him from staying active.
“I wanted to show cancer up and beat it,” he says. “Right after my first chemo treatment, I got home and went on a run. I continued to work out through all the sessions.”
In addition to staying active, Braddy also fasted for 68-72 hours around each chemotherapy session. He credits both fasting and staying active as helpful in controlling his nausea and fatigue after treatment.
Since his diagnosis, Braddy has become passionate about talking to others about the importance of colorectal cancer screenings.
“If I could rewind things, I would have no hesitation to get a colonoscopy done so much sooner. The colonoscopy procedure is easy and well-worth the effort it takes to get one. A lot of people, including me, think ‘this will never happen to them.’ Screening could have prevented me from surgery, chemo and bills,” he says.
Regular screenings for colorectal cancer are recommended to begin at age 45. If you’re eligible for a screening and do not have one scheduled, take time during Colorectal Cancer Awareness Month in March to talk to your primary care provider, obstetrician-gynecologist or gastroenterologist about scheduling an appointment.
Now, Braddy is cancer-free, and continues to stay on top of his appointments to take preventative measures to stay healthy.
“If there’s one thing I would say to people it would be that just because you feel good doesn’t mean something might not be wrong,” Braddy said. “Colon cancer is very treatable if caught early. If not for yourself, schedule a screening for your family and loved ones.”
Learn more about screening locations and scheduling information on our Reminder page.
The 2023 North Carolina Governor’s Award for Volunteer Services were recently announced, and four volunteers with ECU Health have been recognized. The award honors the true spirit of volunteerism by recognizing individuals and groups who make a significant contribution to their community through volunteer service. The ECU Health award winners this year are Shantell McLaggan, Gaddamanugu Uma and Ed Chambers. Chad Tucker won the North Carolina Governor’s Award for Volunteer Service: Paid Volunteer Director.
Shantell McLaggan and Gaddamanugu Uma
Shantell McLaggan and Gaddamanugu Uma are third-year medical students at the Brody School of Medicine at East Carolina University and North Carolina Schweitzer Fellows who have led the effort to train more than 60 health professional and undergraduate student volunteers to serve as doulas in ECU Health Medical Center’s Labor and Delivery Department.
Although the program had some initial growing pains, patient feedback about the program has remained appreciative and positive.
“Patients are always recommending our services to others who will give birth at ECU Health,” McLaggan said. “An unfortunate number of people go through the birthing process with little to no support, and our doulas have stepped up to alleviate that issue.”
Word of the program has spread, and they are receiving an increasing number of requests for doula support from mothers across eastern North Carolina.
“Our first cohorts of volunteers have grown into incredible role models for our newer doulas,” Uma said. “Now Shantell and I are focusing on securing the long-term sustainability of our program. We’re actively brainstorming innovative methods to enhance and optimize our services, aiming to amplify our impact and facilitate safe, empowering birth experiences for families in our community.”
Both McLaggan and Uma were surprised to be recognized with this award.
“Receiving this award was unexpected and humbling. It was nice to be recognized for our hard work and dedication to this community. Uma and I have always been passionate about women’s health and racial and social equity, and creating this program has meant a lot to us,” McLaggan said.
Uma cited the vast impact the program has made in a short time.
“When we began, our goal was to support 50 patients in a year, and we’ve far surpassed that expectation; in just 12 months, we trained 67 volunteers who supported 262 birthing patients!” This is an important achievement, Uma said, because of ECU Health’s wide reach to patients across the region. “ECU Health Medical Center is the sole provider of high-risk prenatal care across our 29 county region, so many of our patients have to navigate countless barriers to even make it to our hospital.”
Both McLaggan and Uma emphasized that their efforts would not have been fruitful if not for the support of administrators, classmates and fellow volunteers.
Ed Chambers

Ed Chambers is a patient escort volunteer at the Medical Center, where he has garnered over 5,000 hours of service in the 23 years he’s volunteered for the system. The Pennsylvania native grew up on a dairy farm before being sent overseas to Okinawa, Japan for service in the Air Force. He eventually moved to Goldsboro, North Carolina, where he met his first wife. She passed away in 1997, but he remarried in 1998.
Chambers worked for 30 years at DuPont in Kinston and Charleston, South Carolina before retiring, and in 2000, his wife came home and told him she applied to volunteer at the Medical Center.
“I asked her if she got me an application, and she said, ‘get yourself one.’ So I did and we worked together for about seven years until she had a knee replacement,” Chambers said. “I’ve just enjoyed it ever since and keep right on getting into it.”
Chambers has been recognized as the Volunteer of the Year for the hospital, and he enjoys training new volunteers. He primarily works in the North tower and in the Cancer Center, and while he can only work one day a week, he hopes to continue volunteering for as long as he’s able.
“I’m hoping I can get 30 years in at the hospital,” he said.
Chambers’ favorite part of volunteering is the people.
“Over the years, I’ve enjoyed getting to know the other great volunteers and the patients,” he said. “I enjoy meeting people and helping them out. It’s been a pleasure.”
Winning the award was a “great honor” for Chambers, and it was special that his daughters, one of whom has also volunteered at the Medical Center, attended the award ceremony.
“I know there are a lot of people deserving of this honor, and I hope their time comes,” Chambers said.
Chad Tucker
Chad Tucker is the director of the Volunteer Services Department at the Medical Center, where he oversees the recruitment, training and quality assurance for all volunteers in the Medical Center. He’s worked at ECU Health for nine years, and in addition to his work at the Medical Center, Tucker serves as the vice president for the NC Hospital Volunteer Professionals and volunteers with his fraternity, Alpha Phi Alpha, where he’s serving as the Area Director.
Tucker attended East Carolina University where he got two bachelor’s degrees and a master’s in public health with a health care administration concentration.
“I thought I wanted to be an attorney,” he said. “I took the LSAT and realized it wasn’t my passion.” Tucker said he “fell into” his role and he’s loved it ever since. “This isn’t a position; it’s my passion.”

The best part of his job, he said, is seeing the volunteers interact with the patients, team members and guests.
“I enjoy seeing the impact they make, whether it’s a teenager, a college student who wants to go into health care or someone who is retired wanting to give back.” For Tucker, he doesn’t do the work for recognition. “I just love seeing the organization flourish,” he said. “It’s amazing to see our volunteers’ work and hear team members or patients who are grateful for their service.”
During his tenure, the number of volunteer programs has grown.
“We’ve grown our pet therapy program and our doula program,” he detailed. “We’ve added some people for art therapy, and we’ve had some people do music therapy, as well. Our teen program is one of the largest in the state for VolunTeens, ages 15-17. We’ve added our family medicine clinic and volunteers at the Wellness Center, as well.”
Those experiences have made his time with ECU Health rewarding.
“I’ve loved the opportunity to interact with so many different team members, volunteers, patients and staff, but I’ve also loved the professional development to grow,” Tucker said. “I like to volunteer in the community, so it’s a great marriage of me volunteering and professionally managing volunteers.”
When Tucker attended the Pitt County Commissioner’s meeting to recognize McLaggan, Uma and Chambers, he was surprised to learn he’d won the North Carolina Governor’s Award for Volunteer Service: Paid Volunteer Director.
“I was in complete shock,” he said. “I’m honored to be of service as a paid volunteer, but I also love engaging with volunteers who want to serve in the hospital and community.”
Jennifer Congleton, the administrator of pastoral care and volunteer services, hired Tucker and has enjoyed watching him grow into his role.
“To see him recruit and retain volunteers and become a director – it’s been a tremendous feat,” she said. “It’s been a privilege to work with him, mentor him and see him develop into a leader.”
Congratulations to the winners and thank you to all of the volunteers and team members who serve eastern North Carolina at ECU Health. To learn more about the NC Governor’s Award for Volunteer Service, to nominate a volunteer or to see the full list of the 2023 winners, click here.
Tony Parker has always been an active runner and has long supported the Greenville running and biking community. When he collapsed near the finish line of a 5K road race due to cardiac arrest, quick action saved his life.
Tony was scheduled to run the half marathon that morning back in March of 2021, but backed down to the 5K after his knee started bothering him. It also gave him the chance to run alongside his wife, Delia. It turned out to be a life-saving choice.
“If it weren’t for Delia and the fact that she knows CPR, I wouldn’t be here today,” Parker said. “And if it weren’t for the city of Greenville and the rescue paramedic squads with their AED (automated external defibrillator), I wouldn’t be here today.”
He said he remembers running ahead of his group, including his wife, in the last stretch of the run since his knee was feeling better than anticipated. He patted a young runner on the back to encourage them and then he collapsed.
Delia, a dental assistant with the Department of Veterans Affairs, was required to take CPR courses every three months as part of her job training. That morning, her training paid off in a way she never imagined.
“I got up to the corner and I heard somebody shouting, ‘Man down.’ And when I turned the corner, I was like, that’s Tony,” Delia said.
Delia yelled for someone to call 911 and checked her husband for a pulse, but found none. So she started CPR.
“No one tells you when you’re training on a mannequin that you’ll hear crunching. No one tells you on a mannequin that it’s a different feeling when you’re pushing on somebody’s chest. And it was a little freaky when I first did it, but I was able to stay where I was and to do the compressions,” Delia said. “Someone, ‘Angel,’ as he liked to call them, came up and said, ‘Can I help you?’ They took over and I did some breaths for him.”
Tony and Delia still have not been able to track down the mystery “Angel” from that morning who helped them with CPR.
Shortly after, paramedics arrived and took over. They told Delia that Tony had been revived and he was on his way to ECU Health Medical Center. Paramedics could quickly identify Tony and his wife because he was wearing a road ID, which gives paramedics information on a person, should an emergency event occur. Tony and Delia said they encourage people in their running and biking groups to wear a road ID for these situations.
Delia met Tony at the hospital and some tension was relieved when Tony greeted her with his nickname for her – “Hiya, toots.”
Tony spent about a week at the hospital while the care team ran tests and navigated next steps for the Parker family. They said their time at the hospital and in clinics since has been reassuring and helpful as Tony adjusted to his new normal.
“The care there was incredible. When I say care, I mean that as the word of choice. They really care about what they’re doing and they make sure that they take care of you,” Tony said. “For somebody with a personality like mine, they make sure I don’t try to overdo it right away. The follow up has been spectacular. They stay in contact with my primary care doctor so we’re all on the same page as to what’s going on. ECU Health has been incredible.”
Dr. Christopher Gregory, an interventional cardiologist with ECU Health, said cardiac arrest can come on with no symptoms in some patients and out-of-hospital cardiac arrests are very uncommon to survive due to how quickly care is needed in these cases. Though they may seem similar, Dr. Gregory said it’s important to know the difference between a heart attack and cardiac arrest.
“Heart attacks are when the blood flow to the heart, because of blockages in the arteries, generally speaking, that feed the heart, is impaired,” Dr. Gregory said. “That causes the heart muscle to be stressed, strain or even die – that’s a heart attack. Cardiac arrest is when the heart itself stops. Sometimes heart attacks cause cardiac arrest, but they are completely different.”
Today, Tony is back out walking, running and biking as often as possible. He’s involved in groups of athletes that have experienced heart attacks, cardiac arrest or other heart health challenges and he said this has given him a great perspective on his own journey. As an advocate, Tony meets with groups around the state to stress the importance of road IDs, greater access to AEDs and the need to stay active throughout your life.
“I would rather be an active participant in life than a passive participant and I’ve seen the difference it’s made in the lives of people around me,” Tony said. “My father was very active and his quality of life was excellent. He did have a stroke that impacted him, but he was still walking and getting out there. He played senior games basketball at 86 years old. So when you see the difference, you understand.”
Learn more about ECU Health Heart & Vascular Care.
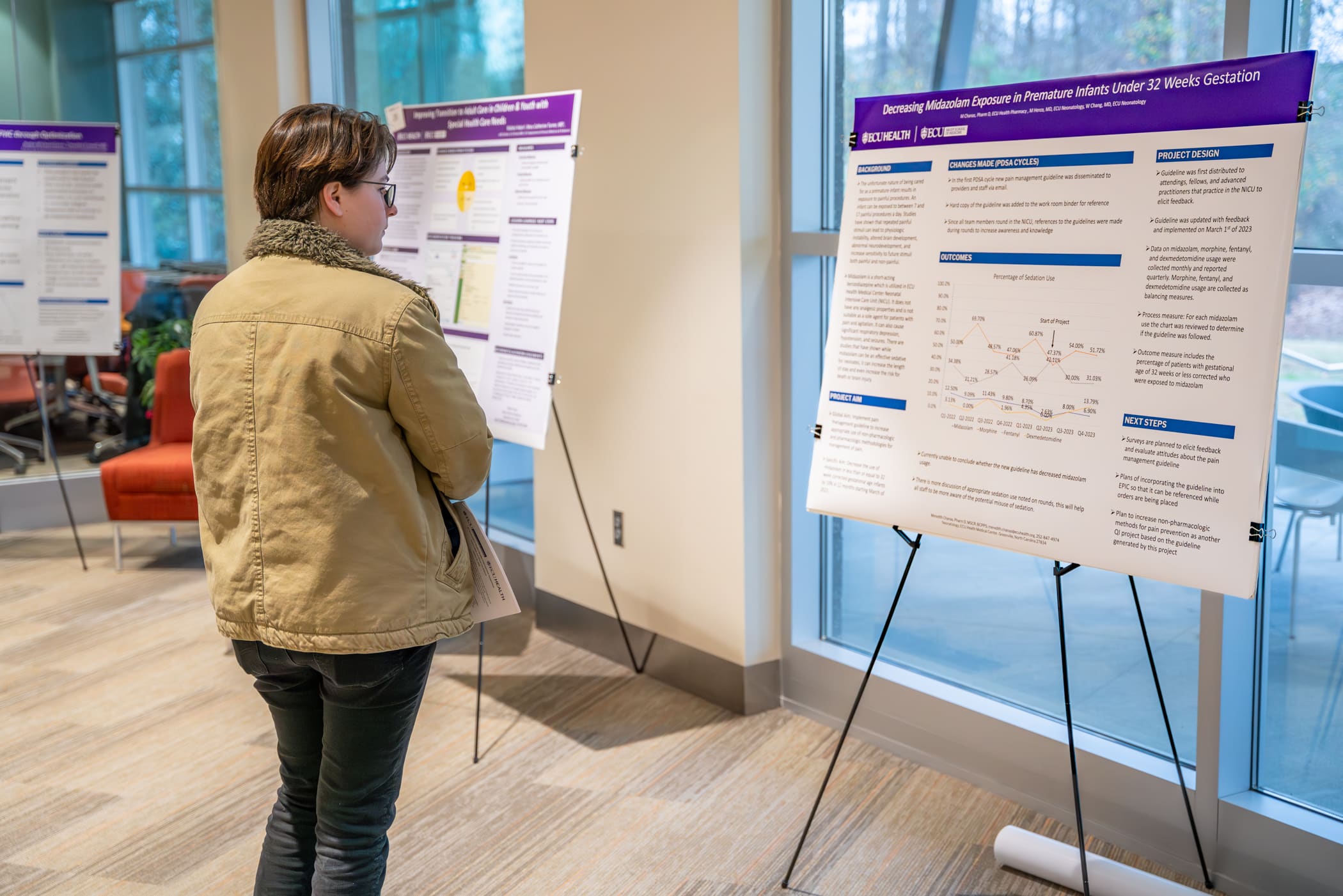
Each year, the ECU Health Quality Improvement Symposium brings together a diverse group of academic and community physicians, health professionals, health care teams, residents, fellows and students from the Brody School of Medicine at East Carolina University to present their work to an audience of peers and health system leaders.
On Wednesday, Jan. 31, ECU Health and ECU’s Brody School of Medicine hosted the eighth annual event at Eastern AHEC. This year’s event was held in-person and virtually, and showcased more than 40 projects related to quality improvement, patient safety, population health and interprofessional practice.
The day kicked off with opening remarks from Dr. Mike Waldrum, CEO of ECU Health and Dean of Brody School of Medicine. After welcoming attendees to the event, Dr. Waldrum expressed his pride in the symposium’s contributions, highlighting the collaborative efforts of teams in addressing regional challenges.

“When I look at these posters and our presenters, I see multidisciplinary, diverse teams coming together to educate, engage in dialogue and drive quality improvement for ECU Health and the patients we serve. I am incredibly proud of our team members and students for their commitment to addressing the immense challenges we face as a region,” Dr. Waldrum said.
Following the opening remarks, selected presenters who were chosen from an application process that took place in late-2023, shared their work with the audience of 178 in-person and virtual attendees.
Presentations were categorized into podium presentations, poster presentations, and works-in-progress poster presentations. Awards for the top three podium and poster presentations were announced in the early afternoon.
PODIUM PRESENTATION:
- Outstanding podium presentation: Erin Atwood, MD, MEd, Department of Pediatrics, Division of Endocrinology, Brody School of Medicine, “Increasing Counseling about the Risk of Hypoglycemia Associated with Alcohol Consumption and Insulin use for Adolescent Patients with Diabetes at the ECU Health Pediatric Diabetes Clinic”
- Honorable mention: Jennifer Stahl, MD, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Brody School of Medicine, “Right Care at the Right Location: Tele ICU Project”
- Honorable mention: Benjamin Copeland, MD, Department of Pediatrics, Brody School of Medicine, “Improving Mental Health Access for Children in Foster Care in Eastern North Carolina”
QUICK SHOT PODIUM PRESENTATION:
- Outstanding quick shot podium presentation: Juan Guillen-Hernandez, MD, Department of Pediatrics, Brody School of Medicine, “Reducing Unplanned Extubations in the Neonatal Intensive Care Unit”
- Honorable mention: Juli Forbes, MSN, RN, ECU Health Beaufort Hospital, a Campus of ECU Health Medical Center, “Improving Efficiency and Staff Satisfaction in the Operating Room Through a Revised Block Scheduling Framework at a Rural Community Hospital”
- Honorable mention: Titilola Babatunde, BS, MS4, LINC Scholar, Brody School of Medicine, “Improving Documentation of a Pediatric Early Warning Score in the Electronic Health Record”
- Honorable mention: Kate Knowles, MSN, RN, CNL, Management, ECU Health Duplin, “Back to the Basics: Hand Hygiene”
POSTER PRESENTATION:
- First place: John “JC” Rowe IV, MD, Department of Obstetrics and Gynecology, Brody School of Medicine, “Optimizing Outcomes for Patients with First Trimester Bleeding”
- Second place: Gabriella Boccia, MHA, Administrative Fellow, ECU Health, “Improving Sick Visit Clinic Access at ECU Health Physicians Adult and Pediatric Health Care”
- Third place: Stephanie Smith, MSN, RN, ACM-RN, Maynard Children’s Hospital, ECU Health Medical Center, “Improving Fall Risk Identification in Pediatric Patients”
With a total of 15 podium presentations and 29 poster presentations, symposium attendees gained insights into a variety of Quality-related projects. Dr. Waldrum emphasized the importance of what these presentations can offer.
“These presentations cover complex health care problems and this symposium enables us to think deeply about how we can tackle important issues facing our region,” Dr. Waldrum said. “It is always gratifying to see our team members and students come together to demonstrate their expertise and showcase the passion they have for the work they do.”
The symposium closed with two concurrent education sessions led by ECU Health team members:
- Patient Safety, Reliability Science and Root Cause Analysis Application presented by Susan Ingram, MSN, RN CPHQ, Director of Patient Safety
- Fostering Psychological Safety for Team and Quality Outcomes presented by Randy Cobb, DSL, ACC, CPCC, Director of Organizational and Leadership Development
To learn more about the symposium and view a list of presentations, click here.
Dr. Niti Singh Armistead, the chief quality officer and chief clinical officer at ECU Health in Greenville, keeps making the right career choices.
In college at George Mason University, she switched her major from engineering to physics and pre-medicine after she discovered that there were loans available to pay for medical school. “I appreciate what programmers do every day, but I realized that my own joy was working in the medical field,” she says.
After graduating from the University of Maryland School of Medicine, she specialized in anesthesiology, thinking her physics background would be helpful. She switched to internal medicine because she found the long-term relationships with patients more enduring and satisfying.

Now, at ECU Health, she’s focused on acute care and still sees patients on a regular basis. She took on administrative roles in 2018 and 2019 before the start of the COVID-19 pandemic, successfully helping steer the healthcare system during a challenging time.
“None of us knew what we were in for,” says Armistead. “For me, it all just kind of came together. How do you support an already underserved population? How do you rise to the occasion as the only healthcare system east of I-95 with an academic arm to do it all, to build the infrastructure for the testing and to educate the community? Those were the kind of interventions I got to lead.”
Read the full story in Business North Carolina.
ECU’s clinical laboratory science students — who after graduation run the nation’s medical labs in hospitals, for public health offices and in the pharmaceutical and biotech industry — got a huge boost recently with the acquisition of a new device that automates the process for identifying blood types.
Funding for the new system, some $6,600, came in part from the American Society for Clinical Pathology and the ECU Medical and Health Science Foundation’s CLS Priority fund.
The instrument, known as the Ortho Clinical Diagnostics workstation, replaces a laborious process of mixing blood samples with reagents by hand to allow laboratory professionals to quickly and accurately establish blood types and identify donated blood that can be safely transfused to a recipient.

Traditional blood analysis methods, which ECU’s Department of Clinical Laboratory Science chair Dr. Guyla Evans and her faculty peers still teach their students, involves mixing drops of blood with antibodies that register specific blood types. The process also registers Rh factor, proteins on the surface of some people’s blood cells that affect who can receive blood donations from whom.
Using the established test tube method is a time and attention intensive process.
“It can be kind of hard to teach students how to read the tubes because it’s subjective. You have to read the tubes right away, and there are a lot of steps,” said Michael Foster, a senior from Roanoke Rapids, who already works in the blood bank at ECU Health Medical Center in Greenville.
Using test tubes to identify blood samples is a tricky business: laboratory personnel must identify cell reactions by eye and they have a limited time to observe and interpret the results.
“The name of the game in blood banking is accuracy, but it’s also speed. You want to get it in the centrifuge and as soon as it’s ready to come out of the incubator and get it going,” Evans said.
The new system uses a cartridge, which requires less blood in the sampling process and has the advantage of leaving the sample readable by technicians for up to 24 hours. This allows laboratorians to double check their work or have a peer review their results.
An added benefit for the cartridge system is baked-in surety of the testing chemicals.
“You don’t have to worry about adding the wrong reagents because the cards are color-coded and the reagents are already added in,” Foster said.
Each cartridge may cost up to $25, which isn’t cheap, but Evans and Lorie Schwartz, a research technician and CLS instructor, both agree that the new system is at least as cost effective as traditional testing methods due to labor costs and the intangible benefit of assurance that the results are valid.
The new system is less mentally taxing for the medical laboratory scientist, Evans explained.
“In the blood bank, everything has to be carefully documented. Nothing is ever assumed or taken for granted—blood bankers trust no one, they believe no one,” Evans said. “If I’m going to do a cross match for two units, and the antibody screen and the blood typing, that’s 12 to 15 tubes that I have to label every time. It’s a lot faster to label one card or a couple of cards, depending on what testing you’re doing.”
The CLS department received the equipment in December, just a bit too late for the current class of students, including Foster, who will graduate in May. The seven graduating students were able to train on the gel microcolumn system during clinical rotations with ECU Health and Nash UNC Health, where they got hands-on experience.
Evans said the COVID-19 pandemic made teaching blood banking techniques very difficult because, while theory is crucial to understanding lab work, getting hands-on training is critical for learning.
Students who learned during the pandemic were dropped into the deep end during clinical rotations in working labs and had to put theory into practice, both with traditional test tube methods and the gel cartridge system.
“During clinicals, we went through quite a number of cards trying to figure out what antibodies were present in the blood because they would give us unknown samples and we would spend the entire eight hours trying to figure out what the sample was,” said Bryce Glover, a senior from Fayetteville. “If we went down the wrong path, that was one card wasted.”

Because they are eligible to work in clinical labs once their clinical rotations were completed, Foster, Glover and the other members of their cohort already have jobs in area labs.
“ECU Health and ECU’s commitment to incorporating the latest technologies into both health care delivery and hands-on training for our future workforce not only benefits students during their academic journey but also equips them with valuable skills that are highly sought after in the health care industry,” said Carolyn Merritt, ECU Health lab scientist.
“Keeping students up to date on the latest technologies, such as gel testing, is crucial for optimizing their limited time during clinical rotations. Our goal is to help prepare the next generation of high-quality health care professionals, and hands-on experience with innovative technology ensures our students are well equipped to provide important services once they enter the workforce,” Merritt said.
The advances in high tech equipment, combined with severe staffing shortages, have exacerbated what Evans sees a worrying trend — laboratory professionals aren’t seen on the hospital floors or interacting with nursing staff.
Being squirreled away in a windowless lab the majority of the workday means that medical laboratory scientists and technicians are often disconnected from their peers. Evans counsels her students to be part of the hospital and medical communities they will eventually be part of.
“They must make an effort to be seen as part of the hospital team because they usually aren’t seen,” Evans said.
While medical laboratory scientists might not be as visible as other members of the health care continuum, their role in diagnosing and treating patients can’t be overstated. With an expected need of nearly 17,000 more medical lab scientists nationwide by 2032, the critical skill set that Pirate graduates bring to hospitals and clinics is invaluable.
“When our students get into the clinical system, that’s when they really see the workflow and that last piece of their education comes together,” Evans said. “We’ve been really fortunate that our clinical sites, even though they know they’re dealing with personnel shortages, are taking students on which is extra work they don’t get compensated for. They’re doing it because they know it’s important and that is invaluable.”
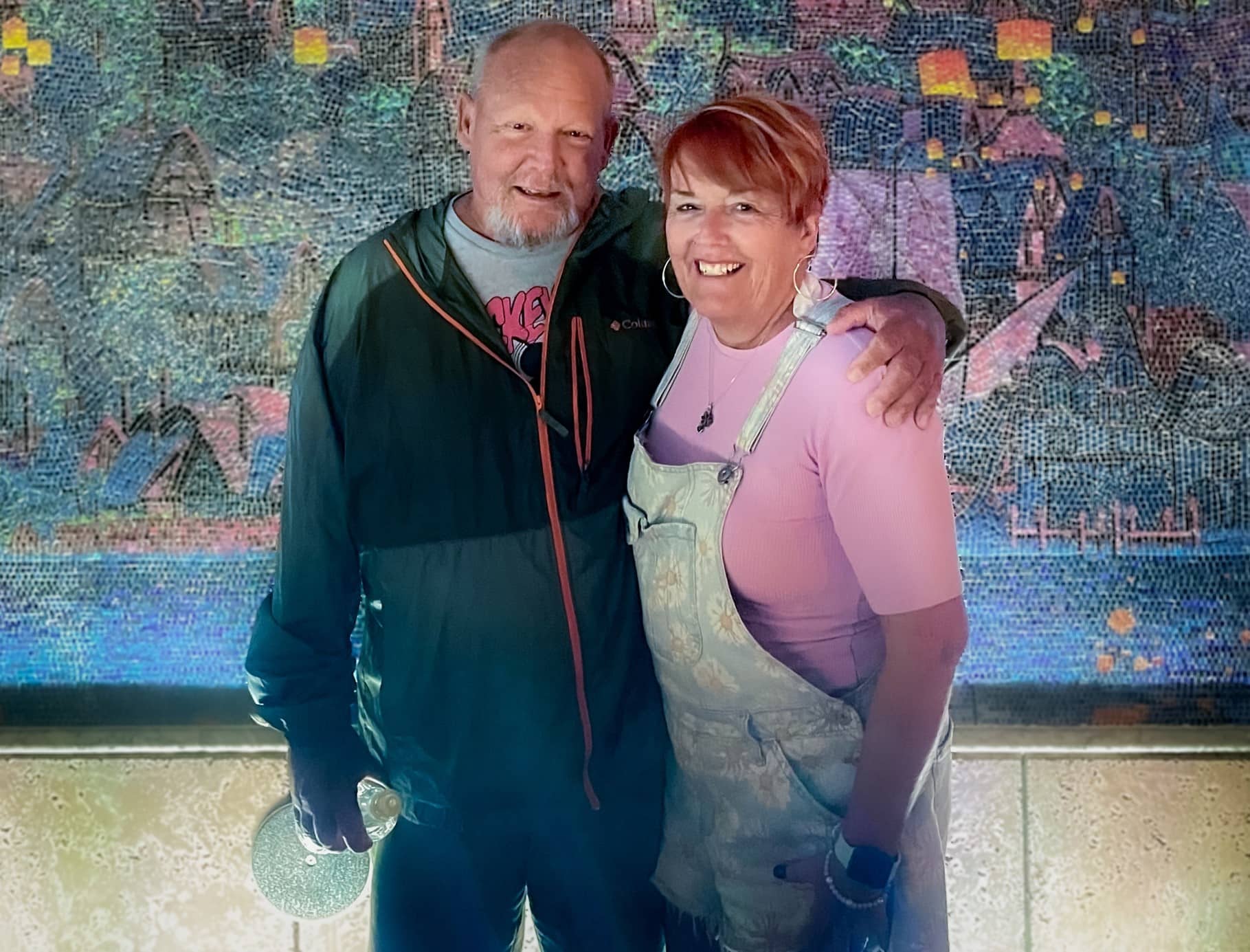
Sharon and Steve McNally of New Bern have been married for more than 40 years. Now, Steve carries a little piece of his wife Sharon with him everywhere he goes.
Steve is diabetic and in 2015, he went through his first round of transplants at a hospital in their then-home state of Pennsylvania.
“It was supposed to have been a kidney and pancreas at the same time,” Steve said. “When they got me on the operating table, the pancreas wasn’t viable. So they said, ‘We’re going to do the kidney alone and we’ll get you a pancreas.’ What happened then was the hospital eventually became decertified and couldn’t do pancreas transplants anymore.”
Then, they joined the transplant list with a health system in Maryland and Steve received a pancreas transplant 30 days later. In the meantime, the new kidney had been damaged due to the lack of a functioning pancreas, but Steve said it was largely working fine until mid-2023. By that time, the McNallys had moved from Pennsylvania down to New Bern.
With Steve’s kidney function worsening, there was little time to spare. He could join another transplant list that may take eight to 10 years to find a donor, start dialysis or personally find a match to donate a kidney.
Sharon said she knew she had to step up for her husband and get tested to see if she could be a match.
“It wasn’t really hard for me because a lot of people say, ‘Oh my gosh, you’re so amazing’ or so this and that but I don’t really feel that way,” Sharon said. “I feel like we’ve been married 40 plus years. We have grandkids and kids together and how could you watch someone get more and more ill and not do something if you can? So I didn’t really think about it.”
Testing started for the two in June and preparation began right away. They found out in October they were a match and an ECU Health team performed the transplant on Nov. 7.
“I’m glad that this was something I could do,” Sharon said. “There’s a lot of people that probably couldn’t have, even if they wanted to.”
For Sharon’s part, she went home the next day while Steve stayed a couple extra days for monitoring before heading home. While they each needed some help early on after coming home, they were both happy to support each other, as they’ve been doing for more than four decades.
Dr. Margaret Romine, transplant surgeon at ECU Health, and Dr. David Leeser performed the transplant along with other members of the ECU Health transplant team. She said she was most proud that the team could take on a case like the McNallys, especially given Steve had been through a kidney and pancreas transplant previously.
“They had already been through a lot before even coming to us but they had such great attitudes and were great patients to care for,” Dr. Romine said. “We have such a great team and that really sets us apart from other programs. It’s not just about what the surgeon thinks – the nephrologists play a huge role. Our coordinators, nurses, pharmacists, social workers all play a huge role. We can’t do what we do without the entire team. Whenever we make a big decision to take on a patient like him, it’s done as a team.”
Steve and Sharon both said they were happy with their experience at ECU Health and shared appreciation for the care team that helped guide them through the process and into recovery.
Now, they are looking forward to a spring working outdoors, something they both love but missed out on last year.
Sharon said if she could share one message, it would be on the importance of organ donation.
“Organ donation is just such a wonderful thing. I mean, three different times it saved my husband,” Sharon said. “You know, a lot of people don’t want to do something like that even after they’re gone because it just it seems weird to them. But honestly, I think it’s a wonderful thing.”
