Greenville, N.C. – East Carolina University and ECU Health are launching an initiative to increase the number of adult gerontology acute care nurse practitioners serving as advanced practice health care professionals in ECU Health’s critical care settings. This effort builds on the collective commitment of both organization to solve the rural health challenges in the region as well as the state.
The effort – conceived by nursing and education leaders from ECU’s College of Nursing and ECU Health – will benefit both the university and the health system, said Dr. Bim Akintade, the dean of ECU’s College of Nursing. An investment of nearly $1.5 million over five years from ECU Health will increase the College of Nursing’s capacity to graduate trained and qualified nurses who can meet the growing need for acute care practitioners to treat the hospital’s sickest patients.

“ECU Health is proud of its close relationship with ECU and the College of Nursing, particularly as it pertains to our efforts to adapt to the national health care workforce shortage,” said Dr. Daphne Brewington, ECU Health’s vice president of nursing. “Our success as an academic health system is predicated on our ability to leverage clinical and academic excellence in order to ensure we can provide high quality health care for the residents of eastern North Carolina.”
Nationally, the aging population is growing, accompanied by the shortage of health care workers. This collaboration not only strengthens the health care workforce in eastern North Carolina but also contributes to improved health outcomes and increased accessibility to specialized care for older adults in the communities of eastern North Carolina.
Through this effort, ECU Health is helping fund the development of a new Adult Gerontology Acute Care Nurse Practitioner Post Graduate Certificate, which will train current nurse practitioners to treat acute care adult patients. The investment also provides funding for a program director who teaches and an additional part-time faculty member as well as administrative support and operational costs.
The program will reserve six enrollments per enrollment cycle for current ECU Health employees, highlighting the importance of providing specialized training that benefits the region.
“Our plan is to take the next few months to work with our partners at ECU Health and find clinical placement sites in critical care environments for ECU Health employees who enroll in the program,” Akintade said. “They need nurses, and training nurses is our business and passion. This collaboration is a win-win and makes complete sense for the University, the Heath System, the region, and the state.
Clinical placements for students employed by ECU Health will take place at ECU Health facilities, which will help to alleviate a major sticking point for training advance practice nurses – finding clinical placements for students in training. It also has the potential to create pathways for those in the program to experience acute care at both ECU Health Medical Center and in ECU Health’s regional community hospitals.
The initiative isn’t limited to the current arrangement and both ECU and ECU Health continue to explore ways to leverage this effort to design innovative solutions that benefit the people of eastern North Carolina.
“Eastern North Carolina depends on institutions like ECU Health and ECU to collaborate on innovative solutions that drive us towards our mission of improving the health and well-being of the region,” said Dr. Trish Baise, ECU Health’s chief nursing executive. “As a health system serving 1.4 million people, we need more nurses at every level in order to meet the region’s immense needs. The College of Nursing is one of the premiere nursing education schools in the nation and our health system is great training ground for developing a health care workforce with a focus on rural health challenges. I am excited to see the benefit this program will have on our patients and team members.”
Dr. Carl E. Haisch, professor of surgery in surgical immunology and transplantation and vice chair of surgical education in the Brody School of Medicine at East Carolina University, has been inducted into the American College of Surgeons Academy of Master Surgeon Educators.
Dr. Carl E. Haisch
Haisch is among a cohort of 63 surgical educators to be inducted into the academy in Chicago this fall.
“Dr. Haisch has contributed greatly to the education mission of the ECU Department of Surgery over many years,” said Dr. Eric J. DeMaria, interim chair of Brody’s Department of Surgery. “We continue to rely upon his expertise and experience as we develop new and better ways to educate surgeons both at ECU and around the world going forward. We are extremely pleased that the American College of Surgeons has recognized him for his many important contributions to education.”
Haisch is a dedicated educator whose experience in the field includes attending surgeon in transplant and trauma surgery. He served as chief of transplant at ECU for 20 years and was a member of the trauma team for 15 years. He has served on numerous local, regional and national committees and served as chair of the board of Carolina Donor Services. He is also a member in numerous transplant and trauma societies and is a member of the Society of University Surgeons, the American Surgical Association, the American Society of Transplant Surgeons and the Southern Surgical Association.
Once inducted, members actively engage in advancing the academy’s programs and goals, which are to advance the science and practice of innovative lifelong surgical education, training, and scholarship in the changing milieu of health care; foster the exchange of creative ideas and collaboration; support the development and recognition of faculty; underscore the importance of lifelong surgical education and training; positively impact quality and patient safety; disseminate advances in education and training to all surgeons; and offer mentorship to surgeon educators throughout their professional careers.
“The Academy of Master Surgeons Educators, a vital and ‘living body’ of the American College of Surgeons, continues its legacy of advancing the science and practice of surgical education. The academy is pleased to induct the 2023 cohort of distinguished and highly accomplished educators. This recognition is a true testament to the unwavering commitment of the college to develop and promote ‘best practices’ in surgical education, with the overarching goal to always improve patient care,” said Dr. L.D. Britt, past president of the ACS and co-chair of the academy’s steering committee.
Haisch’s other activities and honors as a surgeon educator include serving on the executive committee of the Association of Program Directors in Surgery and its foundation. He has served as a general surgery program director, surgery clerkship director, associate dean for faculty development and interim associate dean for student affairs. He has received numerous teaching awards including the Bernard Vick Teaching Award, the Distinguished Professor for Teaching from the UNC Board of Governors and the ECU Achievement in International Teaching Award. He was the honorary first recipient of the Carl Haisch Humanism Award initiated by the surgical residents in Brody’s Department of Surgery.
The ACS Academy of Master Surgeon Educators works to advance the science and practice of education across all surgical specialties. Individuals are selected as members, associate members, or affiliate members following a stringent peer review process. This year’s cohort includes 27 member inductees, 35 associate members, and one affiliate member. The first inaugural cohort was inducted in 2018 and the academy has grown to 358 professionals who represent 10 surgical specialties other than general surgery. Inductees are from 18 states and the District of Columbia. They come from 10 countries including the United States.
The ACS is a scientific and educational organization of surgeons that was founded in 1913 to raise the standards of surgical practice and improve the quality of care for all surgical patients. The college is dedicated to the ethical and competent practice of surgery. Its achievements have significantly influenced the course of scientific surgery in America and have established it as an influential advocate for all surgical patients. The college has more than 88,000 members and is the largest organization of surgeons in the world.
“I was just doing what is right.”
Sheila Grady, Community Liaison with ECU Health’s Home Health and Hospice, has never been one to seek the limelight in her 29-year career. In fact, she’d rather be behind the scenes, helping people and making a difference.
“She has a heart of gold, and she’s going to do whatever it takes to assist and serve our patients and families,” said Sarah Taylor, Sheila’s supervisor and the manager of marketing and hospice volunteer coordinator. “She understands we are a business, but we’re in a people-serving business and that’s our number one goal.”
When Aaron Hair contacted Sheila about having two memory bears made after the death of his father, her drive to do what’s right while serving patients and their families got people’s attention.
“My dad was diagnosed with cancer two years ago,” explained Aaron. “When the decision was made that he would stop treatment, he was admitted to palliative care at the Medical Center, but his doctor and nurses recommended the hospice house in Greenville.”
While his father was in the hospice house for less than 24 hours before passing away, Aaron recognized the hospice team members made a difficult situation easier to bear.
“They made us feel at ease and explained everything,” Aaron said. “From the facility to the staff, they were all top notch.”
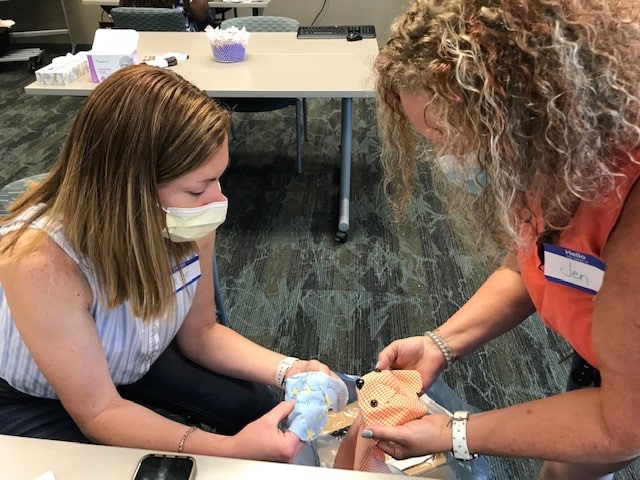
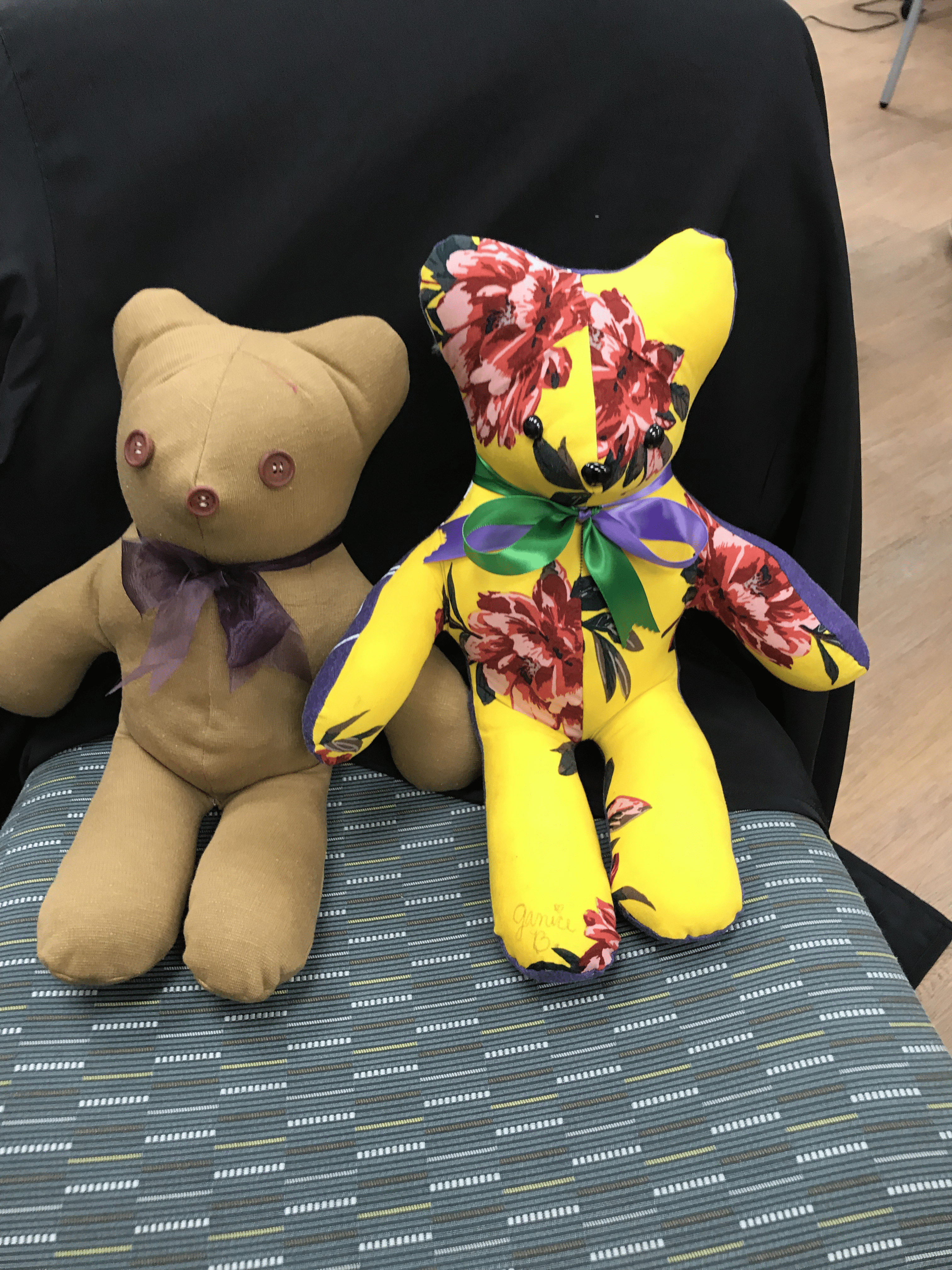
After his father’s death, Aaron and his family wanted to make use of the Memory Bear program, a service of ECU Health’s Home Health and Hospice team that makes teddy bears or pillows using an article of clothing from the family member who passed away. Sheila has run the program for the past two years.
Sarah noted that it was Sheila’s leadership that made the Memory Bear program what it is today.
“Now we have workshops in Greenville and Kenansville, and we’re serving all hospice patients on our service. And there’s a lot of love put into these bears,” Taylor said.
The work, Sheila emphasized, is done entirely by volunteers.
“These are nurses who pick up materials and drop off bears after their shifts,” Grady said. “Some are retired from health care, and some are retired teachers. They come from all walks of life, and they don’t ask for a dime.”
Aaron contacted Sheila directly to request two memory bears, one for each of his daughters. The challenge, however, became how to get his dad’s shirts to the seamstresses.
“I live in Johnston County but was working in Havelock. It would have been challenging to get the shirts to Greenville,” Aaron explained. As they talked, Sheila learned that his commute took him right by her office in Duplin County. “She gave me her personal cell phone number, and I called her when I was on the way so we could plan a meet-up. She didn’t have to do that.”
As for Sheila, it was just an example of her drive to do the right thing.
“He was a young man who lost his father,” she said. “He was an only child, and he was asking for something for his family.”
Once she got the shirts, Sheila realized that Aaron had only asked for bears for his daughters, but nothing for his mother.
“She called me and said, ‘You didn’t mention making anything for your mom,’” Aaron said. “But I only asked for two bears because that’s the limit set on the brochure, and I wasn’t going to ask for more than that.”
Sheila, however, emphasized that the two-bear limit is a flexible parameter. ”We listen to the person’s story and we make what is right for each person. I knew we needed to make a pillow for his mom.”
A few days later, the seamstress working on the project contacted Sheila with another observation.
“She said, ‘This man didn’t ask for a thing for himself,’ and she told me they had enough material to make a pillow for Aaron, as well,” she said. “So that’s what they did.”
When it came time to deliver the items, Sheila again went out of her way to ensure they were delivered prior to a planned trip out of town. When she brought the items out, Aaron learned that not only had the bears and pillow for his daughters and mom been created, but that a pillow had been made for him as well — made from the shirt his dad wore the last time the two of them went fishing together.
“I hadn’t thought about myself,” Aaron admitted. “It was heartwarming for someone to think about that.”
Sheila confirmed that it was common for family members not to think of requesting a pillow or bear for themselves, even when it’s someone familiar with the program.
“One of the nurses who hired me for this job – her husband died suddenly. I reached out to her and told her, ‘I want to make a bear for you,’ and the nurse said she had never even thought about it. We made her a bear, and later she sent us a picture of her in bed with the bear made from her husband’s pajamas,” Grady said. “Below the picture she wrote, ‘I still have him with me.’ That’s what the Memory Bear program is all about.”
After his meeting with Sheila, Aaron knew what he wanted to do.
“When I left the parking lot that day, I went home and called my brother-in-law, who works for ECU Health, to get Mrs. Grady’s supervisor’s name so I could let them know what she had done,” Aaron said. “Mrs. Grady is a loving and caring lady who I feel I have known my whole life.” He ended up writing an email that garnered a lot of attention.
“I had no idea he would write that email,” Sheila said. “I don’t do this for the recognition.” She was recognized, however, at a surprise gathering in her Kenansville office on Oct. 9. “I was shocked, and it’s difficult to surprise me,” Sheila laughed. “When I saw my husband and family in my office that day, I knew something was up.”
However, she is quick to pass credit to others.
“The team makes this happen,” Sheila said. “The nurses, PTs, aides, OTs and social workers. The chaplains. The seamstresses who make the bears. They’re the real heroes.”
That her home office in Kenansville has won multiple Patient Choice Awards this year bears that statement to be true.
Sheila also emphasized that the ECU Health hospice service, which is made unique by the Memory Bear program, is deeply important.
“I wasn’t sure I’d like the hospice setting when I was first hired,” she admitted. “But I want to make a difference in people’s lives, and that’s what we do. Now I educate people about our home health and hospice services and assist with referrals, and I love it because I know I am making a difference.”
Her supervisor, Sarah, agreed: “We can walk the journey with these patients and their families, and Sheila is the type of person who is going to make sure the family is OK and she can bring them some peace.” Sarah also noted that the Memory Bear program has gained a positive reputation in the community: “Now we have people say, ‘Oh, you’re the hospice with the memory bears?’ and that’s awesome.”
Sheila has plans to retire in mid-November, although she’s not retiring from the Memory Bear program just yet.
“I have another grandchild on the way, so I’ll be spending time with my family, but I come from a long line of people who believe work is a good thing,” Grady said. “I’ll volunteer with the Memory Bear program for sure.”

Dr. Michael Waldrum
For those of us fortunate enough to be involved in rural health care, the third Thursday of November is a special time to pause, reflect and look forward. Designated as National Rural Health Day in 2011, this particular Thursday has served as an important moment to honor the contributions of rural health care workers, including the 14,000-plus ECU Health and Brody School of Medicine at East Carolina University team members who care for eastern North Carolina.
You don’t have to look far to see the impact of rural health care. All around us are doctors, nurses, allied health professionals, professors, students and others who make high-quality health care possible here in eastern North Carolina. Today is a day to celebrate them and their tireless dedication to serving a region of 1.4 million people.
ECU Health’s vision to become the national model for rural academic health care is necessitated by the shared challenges rural communities across America face. An estimated 62 million people call rural America home, and they all experience health care in similar ways: fewer resources, higher burdens of diseases like diabetes and heart disease, difficulty accessing care and a higher number of under and uninsured people when compared to urban communities. Eastern North Carolina is no different.
These are undoubtedly complex challenges, but they can be solved through innovation and ingenuity. For example, the American Association of Medical Colleges estimates a shortage of more than 124,000 physicians by 2034, a reality that will disproportionately impact rural communities. We can anticipate the impending shortage, understand the disproportionate impact it will have on our communities and utilize the unique resources available at our academic health system to address these challenges.
Studies show that family medicine residents who spent 50% or more of their training time in rural settings were at least five times more likely than residents with no rural training to practice in a rural setting. Brody and ECU Health together launched the Rural Family Medicine Residency program in 2021, and the results are immediately evident with multiple residents already committed to continue practicing in one of ECU Health’s rural family medicine clinics.
There are countless other examples like the Rural Family Medicine Residency program that showcase the value of an academic and health care delivery system. When we created ECU Health, the vision was to create a premier academic health care enterprise that could serve as a national model for other rural health systems to learn from. We are on our way to realizing that vision, and I am proud of our work so far. Our progress would not be possible without the incredible team members who have dedicated their careers to improving the lives of others.
I encourage our community members to thank a health care worker this week. Our lives are better because they choose to serve here in rural eastern North Carolina.
Resources
Rural Family Medicine Residency Program
Rural Family Medicine Residency Program takes unique approach to training physicians
Dr. Audy Whitman is an eastern North Carolinian, through and through. He was born in the farming town of Seven Springs – a town of roughly 80 people – in Wayne County.
Like in many towns in eastern North Carolina, its citizens struggle with poverty and access to health care. It is there, in Seven Springs, where Dr. Whitman’s rural upbringing helped him discover a love for medicine that influences his work today.
Today, Dr. Whitman is a family medicine physician for ECU Health and clinical assistant professor at the Brody School of Medicine at East Carolina University, but back in Seven Springs, he was a helping hand in the tobacco fields, braving the eastern North Carolina heat and humidity.
“There is no more powerful motivator in the universe, in my humble opinion, than standing in the middle of a tobacco field in the late summer with 99 percent humidity, no shade and it’s 100 degrees outside,” Dr. Whitman said. “Your hands are caked with tobacco gum. The nicotine is soaking through your skin, so you feel nauseous all the time. Those long days taught me a great work ethic but they were also powerful motivators.”
Rural health care realities
Americans who live in rural areas make up 20% of the United States population and residents in these areas face a myriad of challenges: shorter life expectancy, higher mortality, higher rates of poverty, fewer local doctors and greater distances to travel to see health care providers. Only 10% of U.S. physicians currently practice in rural areas.
Physician shortages are no secret across the country, with the Association of American Medical Colleges estimating a shortage of up to 124,000 physicians by 2034, and rural areas are at an even greater risk.
The Brody School of Medicine was founded over 40 years ago to train primary care physicians to provide care for rural eastern North Carolina. These challenges inform the medical school’s mission and its proven track record is best represented by the fact that Brody is No. 1 in North Carolina and No. 2 in the United States in the percent of graduates in the last decade who chose careers in family medicine.
Programs like the Rural Family Medicine Residency Program take that work a step further by focusing on initiatives that help place providers in rural areas. Studies show that family medicine residents who spent 50% or more of their training time in rural settings were at least five times more likely than residents with no rural training to practice in a rural setting.

“Rural health care is under duress, and our rural communities need solutions,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine. “The Rural Family Medicine Residency Program is another great example of ECU Health and Brody understanding what the community needs are and creating new pathways to educate physicians to meet the community’s needs and improve the health and well-being of those communities.”
Setting a path forward
After Dr. Whitman was approached to create and administer the program, things moved quickly. A “national guru for all things family medicine” made a visit to eastern North Carolina to consider the best locations for residents to begin their rural training. Dr. Whitman and team reached out to other universities and health systems with established programs and traveled to learn about rural organization structure and rural curriculum best practices. Two years later, the Rural Family Medicine Residency Program had its first cohort ready for training.
The first year of the program features training at ECU Health Medical Center, a Level I Trauma Center, and helps set the residents up for success when they get to the rural environments in their second year.
“Anything and everything you can imagine seeing in residency training, you’re going to see at the medical center,” Dr. Whitman said. “We provide this very intense, inpatient-heavy first-year experience for these rural residents where they get to see really sick, really complicated patients with lots of resources at their disposal so they can learn how to take care of these really complicated patients. After their first year of training, when they’ve taken all of these lessons learned, they can go out into these rural communities and apply those lessons learned where they’re the only show in town.”
Dr. Whitman added that while Greenville and eastern North Carolina are rural, the more than 1.4 million patients served through the ECU Health system creates a high volume of patients at ECU Health Medical Center, and the exposure to so many patients during their training is also hugely beneficial for the rural residents.
“An institution like ECU Health boasts a 974 bed, Level I academic medical center where residents train alongside some of the best and brightest health care minds in the state,” said Dr. Jason Higginson, executive dean at Brody. “Medical residents can then serve in our more rural hospitals to apply that knowledge to underserved populations, building a connection to the community in which they serve and making a real difference in the lives of patients.”

Dr. Zeel Shah
Drs. Zeel Shah and Jim Jaralene Porquez were part of the inaugural cohort for rural family medicine residents. Dr. Shah practiced and trained at Roanoke-Chowan Community Health Center in Ahoskie and Dr. Porquez at Goshen Medical Center in Beulaville, both of which are Federally Qualified Health Centers (FQHC) that serve at-risk and underserved rural populations. The mission and vision of these FQHC organizations align with the mission and vision of ECU Health. Together, they seek to augment scarce health care resources in rural communities, improve the health metrics of the communities they serve, and encourage the residents that train in these rural communities to establish roots and continue serving these rural communities after graduation from their residency training program.
Dr. Shah said the year in Greenville was a great experience before continuing her residency training with a focus on serving the rural community of Ahoskie.
“In Greenville you have a lot of resources, but it’s a learning curve to rotate through the different specialties,” Dr. Shah said. “In Ahoskie, the challenges are different. Social determinants of health care, such as finances and distance, play a significant role, and you don’t have the same resources. You learn quite a lot about how to make your limited resources go a long way by relying on creative strategies while using medical expertise you picked up in Greenville.”
Now, as graduates of the program and full-time physicians with ECU Health, Drs. Shah and Porquez feel established in their respective communities and have built trusting relationships with patients, families and fellow team members. Both said the community aspect and truly knowing their patients are among the most rewarding parts of their rural experience. For Dr. Porquez, feeling love, trust and appreciation from her patients has made her time in Duplin County special and a place that she plans to call home after her residency.
“What really drew me into my community clinic in Duplin County specifically, is that my patients are very appreciative of what I do for them,” Dr. Porquez said. “They care so much about my time, my effort and my expertise, and I think in just a couple of years I have built that strong trust and relationship with them. I feel like I don’t just treat them with their disease, but I go further than that. I treat them as a whole, and I get to know their whole well-being. I see them as a whole person and not just the disease that I treat.”
Early milestones

Dr. Jim Jaralene Porquez
For Drs. Shah and Porquez, the personal connections built through the program are so strong that both decided to practice in eastern North Carolina following the completion of the program in 2024. Their graduation, along with the other residents in the first cohort, represent a significant milestone in the program’s short history and help ensure rural communities have access to specially trained, high-quality rural family medicine providers.
Dr. Whitman said he’s proud to see two members of the first cohort choose to stay and make a difference in communities like the one in which he was raised. The successful launch enabled the team to think bigger, and the program now features a new site in Halifax County with an expanded class size of nine residents. The program in general will grow from its original size of 10 residents to a total of 27 residents by 2026.
“Moving forward, I see nothing but growth for us,” Dr. Whitman said. “We are truly doing mission-driven work and trying to bridge the chasm of health care disparities of urban centers and rural areas here in North Carolina.”
Dr. Waldrum agreed and said he sees the program as the beginning of something special for eastern North Carolina and rural medicine.
“My hope is that we can take the knowledge gained through the Rural Family Medicine Residency Program and apply those lessons towards other specialized clinical areas of expertise in the near future,” Dr. Waldrum said. “We are proving that we can be highly successful in creating rural residency tracks and our historic success training rural providers who go on to practice here in North Carolina is a further testament of our ability to create unique solutions that meet the needs of those we serve.”
Resources
Greenville, N.C. – Coastal Plains Network improved care for more than 27,000 Medicare beneficiaries in eastern North Carolina and saved Medicare $13,220,162 by meeting quality and cost goals in 2022, according to recently released performance data from The Centers for Medicare & Medicaid Services (CMS). Coastal Plains Network consisted of ECU Health clinics and hospitals as well as Rural Health Group during the performance period.
As a Shared Savings Program Accountable Care Organization (ACO), the Coastal Plains Network – a company founded by ECU Health – reached a record number of savings and earnings in 2022. ACOs are groups of doctors, hospitals, and other health care providers who decide to collaborate and provide coordinated, high-quality care to people with Medicare. Under this collaboration, patients are less likely to need repeat medical tests or unnecessary medical services, have extra help managing chronic diseases, more preventative health services, additional recovery support when coming home from the hospital and care in more convenient ways such as home-based care or telehealth services.

When an ACO succeeds in both delivering high-quality care and spending health care dollars more wisely, the ACO may be eligible to share in the savings it achieves for the Medicare program, also known as performance payments. The Coastal Plains Network received more than $5 million from CMS to invest in improving patient care and outcomes.
“ECU Health and the Coastal Plains Network are proud of the providers who helped bring record savings to the Shared Savings Program, which improves the quality of care, care coordination, accessibility and lowers health care costs for Medicare recipients,” said Todd Hickey, chief strategy officer, ECU Health. “With the savings, ECU Health plans to reinvest in population health efforts aligned with our mission to improve the health and well-being of eastern North Carolina.”
Patients enrolled in the Medicare Shared Savings Program see lower out-of-pocket spending on avoidable health care utilization like emergency department visits because the ACO has better coordinated their care.
“The Medicare Shared Savings Program helps millions of people with Medicare experience coordinated health care while also reducing costs for the Medicare program,” said CMS Administrator Chiquita Brooks-LaSure. “CMS will continue to improve the program, and it is exciting to see that Accountable Care Organizations are continuing to be successful in delivering coordinated, high-quality, affordable, equitable, person-centered care.”
The Medicare Shared Savings Program saved Medicare $1.8 billion in 2022 compared to spending targets for the year. This marks the sixth consecutive year the program has generated overall savings and high-quality performance results. This represents the second-highest annual savings accrued for Medicare since the program’s inception more than ten years ago.
“We are encouraged and inspired by six consecutive years of savings and high-quality care, with 2022 being one of the strongest years of performance to date,” said Meena Seshamani, MD, PhD, CMS Deputy Administrator and Director of the Center for Medicare. “The Shared Savings Program is Medicare’s permanent, flagship Accountable Care Program, and we look forward to continually improving and growing the program, expanding the reach of participating ACOs, and addressing critical health disparities across the country.”
Lung cancer is the leading cause of cancer-related death in the United States and is the second most common cancer in both men and women. In eastern North Carolina, where risk factors for the disease are higher than most other areas in the country, screenings are helping save lives.
“We’ve known since the 1990s that using CT scans at a very low dose can actually save lives,” Dr. Mark Bowling, a pulmonologist at ECU Health Medical Center, said. “Now you can do low dose lung cancer screenings once a year if you meet certain criteria.”
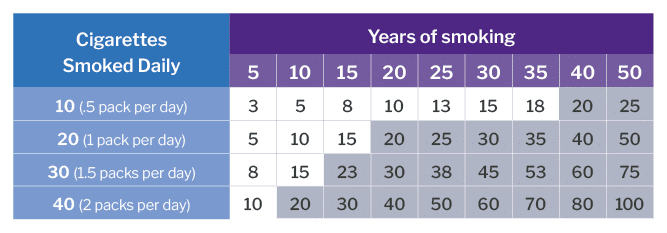
The criteria includes: being between the ages of 50 and 80, having a 20-pack smoking year history – which equals a pack a day for 20 years or two packs a day for 10 years – and having no signs or symptoms of lung cancer.
While low dose CT scans are always available across the system for the insured, a grant program allows ECU Health to offer a once-a-month clinic in Greenville for the uninsured who meet the criteria and have received a referral from their provider.
Jennifer Lewis, Cancer Center outreach coordinator at ECU Health Medical Center, helps run the clinic. She said raising awareness for lung cancer screenings is crucial and can lead to early detection.

“We’re all aware of mammograms for breast cancer screening and colonoscopies for colon cancer, but not a lot of people realize that there’s a screening for lung cancer,” Lewis said. “If we do find something abnormal, we want to find it in its early stages when the outcomes are better, when there are more options for treatment. With lung cancer being a leading cause of cancer-related death, by the time someone starts manifesting lung cancer symptoms, it’s typically very advanced at that time. You have fewer options and your outcomes aren’t positive so our goal is to find cancer before someone begins to have symptoms.”
Lung cancer symptoms are often non-specific, including shortness of breath, coughing up blood, chest pain and inability to move arms among others.
Lewis said she is also passionate about advocating for patients and helping to eliminate stigmas around any cancer, particularly lung cancer.
“We’re here to let people know, if you smoked, if you still smoke, that doesn’t define who you are as a person. We just want to get you screened,” Lewis said. “We’re not here to judge whether or not you smoke. We’re not here to berate you. We will ask if you’ve been educated about smoking cessation, but that’s not why you’re here. We try to make people feel comfortable and feel valued. Your family still loves you and they still want you around so let’s get you screened and make sure you don’t have anything going on that we need to worry about before it becomes a problem.”
Courtney Johnson, Thoracic Oncology Program coordinator at ECU Health Medical Center, has been with the system for 10 years. First, she worked as an inpatient cancer care nurse in the Eddie and Jo Allison Smith Tower at ECU Health Medical Center for about four years and she said it was a rewarding and special time for her.
That led her to her current role in which she helps track and manage at-risk patients through the screening process. She said the best part of her current job is playing a part in early detection.
Recently, she said her team caught cancer in a patient they’d been taking through screenings for about five years. The screenings showed a change in known nodules for the patient and they were sent to surgery to have the cancer removed. Since it was caught in the extremely early stages, the patient did not have any need for chemotherapy and they’ll just have to follow up with future scans for the patient.
“That’s the greatest thing in this position –I can’t prevent everything, I cannot predict outcomes, I can’t prevent what could be the inevitable, but I have a hand in hopefully early intervention,” Johnson said. “I enjoy spending more time with the preventative side of medicine and hopefully allowing our patients to stay out of the hospital. Instead, they come in and we can be proactive with this rather than having to scramble when the patient is in an advanced stage.”
Johnson also shared that radon exposure is a risk factor for lung cancer. She said radon testing kits are available through North Carolina Department of Health and Human Services.
Resources
GREENVILLE, N.C. (November 1, 2023) – ECU Health and Acadia Healthcare held a ceremony today to celebrate the start of construction on its previously announced state-of-the-art, 144-bed behavioral health hospital in Greenville, North Carolina. The event occurred on the site of the new hospital – located at 2820 MacGregor Downs Road, Greenville, North Carolina 27834 – and celebrated the joint venture partnership between ECU Health and Acadia Healthcare, which will own and operate the new hospital together.
Slated to open in Spring 2025, the hospital will be a center of excellence situated less than a mile from ECU Health Medical Center. It will offer comprehensive inpatient and intensive outpatient treatment for adults, seniors, children and adolescents who struggle with acute symptoms of mental health such as anxiety, depression, bipolar disorder, post-traumatic stress disorder (PTSD), as well as treatment for co-occurring disorders. Thomas Construction Group is the general contractor, and Stengel Hill Architecture is the architect for the project.

“Too many people, including children, in North Carolina get stuck in emergency departments when they urgently need short-term and high-quality behavioral health care,” said North Carolina Department of Health and Human Services Sec. Kody H. Kinsley. “This new hospital will create lasting change in this region by making behavioral health services easier to access when and where they are needed.”
The new hospital will also serve as a teaching hospital for psychiatry, social work, nursing and other behavioral health professionals. This will address the shortage of clinical behavioral healthcare professionals in the area, training students and residents from the Brody School of Medicine at East Carolina University, many of whom will go on to practice in eastern North Carolina and carry forth ECU Health’s mission to improve the health and well-being of the region.
The hospital will include 24 inpatient beds specifically for children and adolescents with behavioral health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
“The shortage of mental health resources is a critical challenge in North Carolina,” said Dr. Michael Waldrum, chief executive officer of ECU Health and dean of the Brody School of Medicine. “We are pleased construction is underway for our new behavioral health hospital, and this moment marks another milestone in our effort to improve access to behavioral health care for the region. It will provide the hope and healing residents of Greenville and the surrounding communities need when dealing with complex behavioral health issues.”
Prior to the pandemic, nearly one in five North Carolinians were experiencing a mental, behavioral or emotional disorder, according to a report from the North Carolina Institute of Medicine’s Task Force on Mental Health and Substance Use. In the past three years, national data indicates a growing trend of depression and anxiety symptoms. This partnership demonstrates a commitment to addressing mental illnesses and substance use disorders, normalizing and treating them with the latest science and medicine in appropriate care settings.
“This new hospital will provide North Carolinians with expanded access to quality behavioral health services and treatment from specialized clinical teams in a carefully designed environment,” said Chris Hunter, chief executive officer of Acadia Healthcare. “We are so proud to be affiliated with ECU Health, working together to address the strong need in this area and building upon their legacy and commitment to behavioral health services. This hospital will be a strong member of the Greenville community, collaborating with all organizations, hospitals and first responders. It will be a beacon of hope for patients and families in eastern North Carolina.”
To learn more about the partnership between ECU Health and Acadia Healthcare, visit ENCBehavioralHealth.org.
Each Halloween, patients, families and team members at Maynard Children’s Hospital at ECU Health Medical Center get a chance to break away and enjoy the holiday.
Parade floats from team members and community groups flowed by the Children’s Hospital on Halloween afternoon, giving the children a chance to see some of their favorite characters, like Barbie and Ken, Minions, and floats from Toy Story, Trolls and Encanto. Even the Mystery Machine, a Jeep full of sharks and a pirate ship appeared – all to help make the day a little brighter for the youngest patients at ECU Health Medical Center.
Amanda Jones, a child life specialist at Maynard Children’s Hospital, said there is always a lot of planning that goes into the event, but it’s worth it each year to give the children something to look forward to during the holiday.
“This is a really fun event where they can still celebrate Halloween even while they’re here at the hospital,” Jones said. “It allows kids to be kinds while they’re in the hospital. It’s something that they would normally be doing if they weren’t in the hospital so it kind of brings a little bit of that holiday spirit to the event here.”

For parents, it can also bring a source of comfort. Angela Blanton’s 8-year-old son, Chance, is a patient at the Maynard Children’s Hospital and has a rare condition called Walker-Warburg Syndrome. Blanton said Chance could not be outside for the event, but she still wanted to celebrate Halloween – her son’s favorite holiday – while at the hospital.
She shared photos of past Halloween costume contests he had won and reflected on what this event meant for her. She wore an inflatable chicken costume, worn earlier this month at a Halloween party with her son dressed as Colonel Sanders.
“He would love to be down here, but he can’t be. So I think it’s amazing for the all the children that can be here,” Blanton said. “Seeing them light up, and even me, in this silly costume. Some of the kids wanted to take a picture with me, and I thought that was awesome. To see the smiles from the kids and parents and know how important it is for everyone. Not just the children, but the moms who have been there by the bedside.”
She shared that these events mean a great deal to the patients and families looking for a piece of normalcy in a challenging time.
Patients across the hospital receive goodie bags with art supplies and toys after the event, whether or not they could come. Jones said the event is important for team members
“This is a great event for team members that participate in the parade and for those that come out and watch it,” Jones said. “It’s enjoyable to be able to step away from the bedside and spend time with patients on events like this. I think it’s really uplifting for everyone.”
Ahoskie, N.C. – ECU Health Roanoke-Chowan Hospital hosted a community celebration Tuesday to proudly commemorate 75 years of dedicated service to eastern North Carolina.
Established in 1948, the hospital is dedicated to providing exceptional health care services to its community and has expanded and evolved to meet the changing health care needs of the region.
“We are immensely proud to celebrate 75 years of serving our community,” said Brian Harvill, president, ECU Health Roanoke-Chowan. “Throughout the years, we have strived to provide high-quality health care services with a patient-centered approach. Our commitment to excellence and compassionate care for our community has been the driving force behind our success and continues to positively impact those we are proud to serve.”

Situated in Ahoskie, this 114-bed hospital has been a cornerstone of health care, offering comprehensive services to nearly 40,000 residents spanning Hertford, Bertie, Northampton, and Gates counties. ECU Health Roanoke-Chowan Hospital offers a number of specialty services, including behavioral health, cancer care, pain management, wound healing, sleep services, pediatric asthma management and an ECU Health Wellness Center location in Ahoskie. The pediatric asthma program at ECU Health Roanoke-Chowan Hospital helps children in Hertford and Northampton counties miss fewer days of school, participate more fully in physical activities and look forward to a brighter future.
“Over the past 75 years, ECU Health Roanoke-Chowan has been dedicated to providing exceptional health care services, and this milestone marks a testament to its unwavering commitment to the well-being of the community it serves,” said Jay Briley, president of ECU Health Community Hospitals. “These achievements reflect the hospital’s dedication to improving the overall health and well-being of the community. Today is a day to celebrate the contributions of our current team members and those that came before them to help build a legacy of quality, compassionate care.”
Since its founding in 1948, ECU Health Roanoke-Chowan Hospital has continuously evolved to meet the changing health care needs of the community. On Oct. 24, 1948, the original 40-bed hospital celebrated with a community open house, officially welcoming patients on Nov. 1, 1948. ECU Health Roanoke-Chowan Hospital holds the distinction of being the first hospital licensed by the Medical Care Commission, still bearing license number 1, marking it as the first hospital in the nation constructed using federal funds provided by the Hill-Burton Act. In 1952, the facility expanded with the addition of its first wing, accommodating 25 additional beds, followed by another 34-bed expansion. By 1975, an extra 50 beds, 10 intensive care units and a third floor were added. In response to the growing community’s needs, the original structure was replaced, culminating in the dedication of the present-day hospital in 1992.
“As we celebrate 75 years of service, our hospital’s commitment to clinical excellence remains unwavering,” said Dr. David Lingle, chief of staff, surgeon, ECU Health Roanoke-Chowan. “Our legacy is built on a foundation of dedicated health care professionals who continuously strive to reach the highest standards of care, ensuring that every patient receives the best possible treatment, and making each year better than the last. It is an honor to serve alongside such a great team of professionals.”
ECU Health Roanoke-Chowan has achieved numerous milestones throughout its journey, including recertification as a primary stroke center by The Joint Commission and the American Heart Association/American Stroke Association, Get with the Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll and earning accreditation by the American College of Surgeons Commission on Cancer as a Community Cancer Program.






