Students from the Brody School of Medicine, ECU College of Nursing, and Department of Physician Assistant Studies participated in the Interprofessional Triage and Emergency Assessment and Management (ITEAM) Day mass casualty training event hosted by the Brody School of Medicine’s Emergency Medicine Interest Group Saturday, Oct. 14. The training provides a unique opportunity for students from different health care disciplines to collaborate and gain hands-on experience in managing emergency events.
Experts from the ECU College of Nursing, Brody School of Medicine, Department of Physician Assistant Studies and ECU Health EastCare gave students interactive instruction in procedural skills, such as basic airway management, hemorrhage control and triage techniques. Students then applied these skills during a mass casualty simulation at the Interprofessional Clinical Simulation Center at the Brody School of Medicine.

“ITEAM Day was beneficial to promote collaboration and interprofessionalism among different health care providers,” said Stephiya Sabu, first year Brody School of Medicine student. “Doing this in the setting of a mass casualty event was important as they can be very stressful, and having this experience beforehand will help in the future if we are ever in that situation.”
This year’s simulation was a mass shooting incident. The Office of Clinical Skills Assessment and Education provided simulated patients, portraying symptoms and behaviors consistent with injuries sustained in a mass shooting, including confusion and panic.
Adding an extra layer of realism to the exercise, the ECU School of Theatre and Dance lent its expertise in moulage and makeup to create lifelike wounds on the simulated patients. The ECU Student Government Association provided funding for food and materials.

Students participating in the simulation were coached by a multi-disciplinary team of experts who provided feedback throughout the training. Chuck Strickland, outreach coordinator with EastCare, served as an instructor and provided invaluable insights into the role Emergency Medical Services (EMS) plays in a mass casualty incident. Students were educated on EMS’s initial response, patient management and treatment strategies.
“It is important for students to know the role EMS plays in initial patient triage and how we would request resources and determine patient destinations,” said Strickland. “EMS identifies the volume of patients and their acuity levels, then gets nurses, physicians and physician assistants to do on-scene care for high acuity patients. Students also learned the role of critical care transport and how those professionals would be engaged.”
Nursing students, medical students and physician assistant students shared their respective expertise while working together to promptly triage and treat patients. Both students and instructors underscored the significance of applying classroom learning to simulated real-life scenarios, highlighting the practical value of such experiences.
“Recent events in our community emphasize the unpredictability of mass casualties and just how terrifying they are,” said Lachlan Younce, first year Brody School of Medicine student. “As a medical student, I seek to understand my role as a medical professional in those situations. Participating in this mass casualty exercise exposed me to vital skills like patient triage, resource-efficient care and the importance of teamwork when working alongside my health care colleagues, including PAs and nurses. I am thankful for how this ITEAM training experience helped me develop my readiness as a medical professional.”
Greenville, N.C. – ECU Health is pleased to announce Jenny Markham as Chief Legal Officer for the ECU Health enterprise. Markham officially began her new role serving both ECU Health and the Brody School of Medicine at East Carolina University on Monday, Oct. 16, 2023.

Jenny Markham
“Jenny Markham’s appointment as our Chief Legal Officer is a transformative moment for ECU Health and Brody,” said Dr. Michael Waldrum, CEO of ECU Health and dean of the Brody School of Medicine. “Her experience navigating complex health care transformation will bring tremendous value as we continue to build ECU Health and work toward our mission of improving the health and well-being of the region. We look forward to her expertise, leadership and partnership in achieving our collective vision of becoming a national academic model for rural health care.”
As Chief Legal Officer, Markham is responsible for overseeing the ECU Health Office of General Counsel and all matters within the framework of the joint operating agreement between ECU Health and the Brody School of Medicine, including the health system and Brody. She will report directly to Dr. Waldrum in his dual role as CEO and dean.
Markham brings a wealth of health care legal experience to her new role, having previously served as system vice president and deputy general counsel at UNC Health. Markham earned her J.D. at University of Richmond School of Law, and has experience working as a health law associate for a large North Carolina law firm. Her deep understanding of the intricacies of health care transformation will undoubtedly add significant value to ECU Health as it continues to evolve and strives to enhance the health and well-being of the region.
“It is an honor to join ECU Health as the chief legal officer,” said Markham. “It is immediately clear to me during my brief time here that ECU Health is rooted in service to a mission that has profound impacts on a rural communities across the region. I look forward to contributing to the collaboration between rural health care and academic medicine as we work together to make a meaningful difference in the health and well-being of our community.”
Doctors, nurses and support teams in the ECU Health Medical Center emergency department understand the importance of being prepared for any scenario. That is why the Medical Center ED and Trauma Department teams took part in a mass casualty disaster drill Sept. 7 in an effort to test and improve knowledge of triaging, EPIC documentation, response roles and more as part of the American College of Surgeons accreditation process.
“The more prepared we are now, the more lives we can save,” said exercise director Dr. David Trisler, critical care surgeon at ECU Health Medical Center and clinical assistant professor of trauma and surgical critical care at the Brody School of Medicine at East Carolina University. “Our community depends on us to be there for them during the most difficult circumstances. These types of exercises ensure we will be able to meet that need.”
Mass casualty situations can be difficult to imagine, especially ones that happen here in our local community.
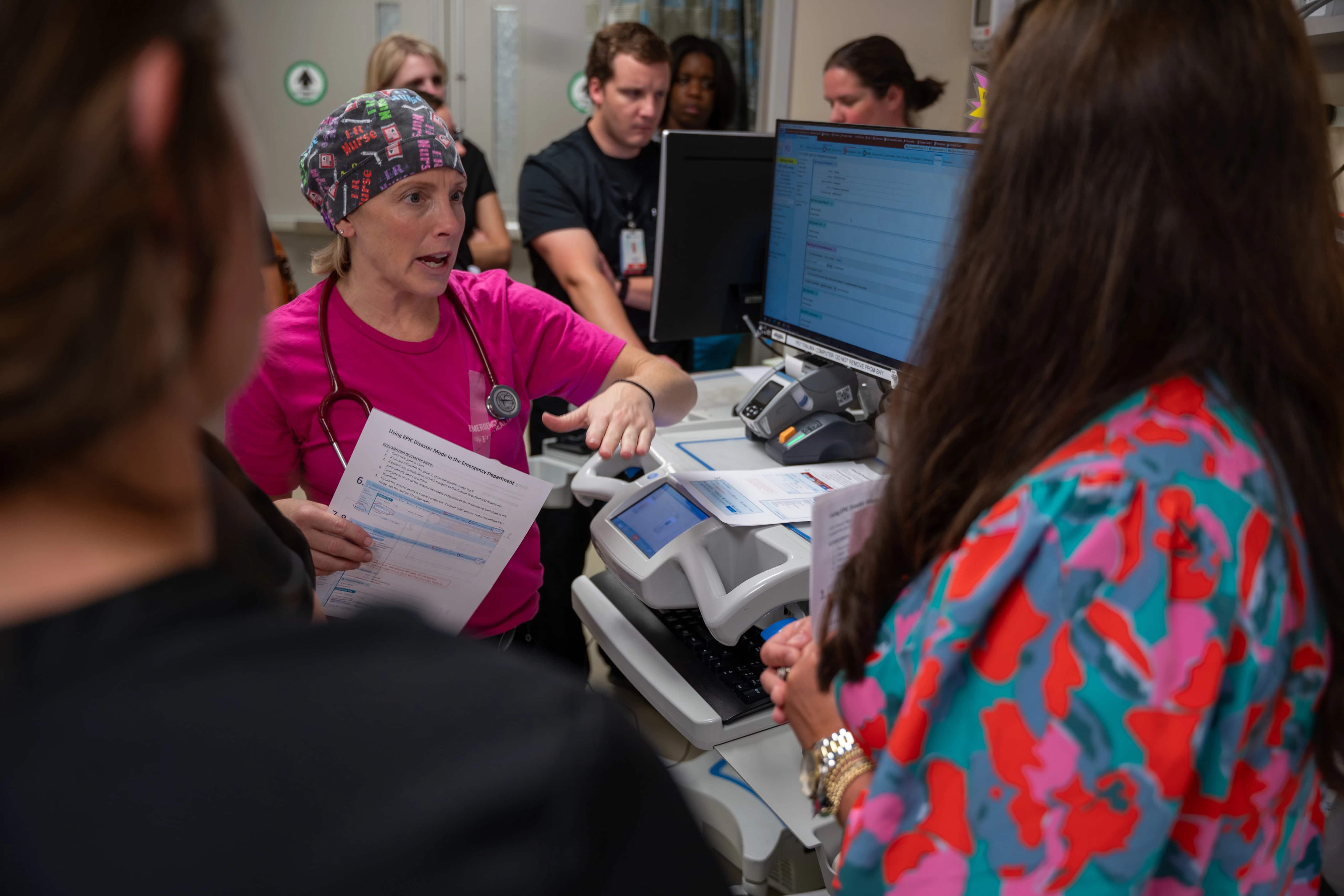
With the use of inflatable mannequins representing the both children and adult patients, the disaster drill consisted of 30-40 casualties brought to the ED following a simulated mass shooting at a local event. Drill participants worked through triaging the patients based on their medical status and moving them through the emergency care and surgical process, using real-time information like numbers of ORs and beds in use during the time of the drill.
For Dr. Eric Toschlog, chief of trauma and acute care surgery for ECU Health Medical Center and Brody and the rest of the emergency department team, preparing for those situations comes with the territory of working at the only Level I Trauma Center in eastern North Carolina.
“The ECU Health Medical Center emergency department serves as a hub for 1.4 million people who live across the region, which highlights the importance of being prepared for any circumstance imaginable,” said Dr. Toschlog. “The more we work to improve our process and understanding, the better prepared we will be to save lives.”
Those involved met immediately following the drill to debrief on the exercise, closely examining strengths and weakness, as well as plans for improvements, all in an effort to ensure the Medical Center emergency department team is well-positioned to provide high-quality care to the community during a time of dire need. The common thread throughout the event and debrief was the direct correlation between preparation and lives that could be saved.
“This was a great opportunity for us to test our knowledge and we certainly learned a lot of valuable lessons that will serve us well,” said Dr. Trisler. “I could not be more proud of the entire ED team for taking the time to participate in this disaster drill.”
Greenville, N.C. – Members of the U.S. House Committee on Ways and Means visited Beaufort and Pitt counties Monday, Oct. 16, 2023, to engage with the community, tour ECU Health Beaufort Hospital and ECU Health Medical Center, hear from community care leaders and discuss the challenges facing rural health care in America. The committee visit consisted of Rep. Greg Murphy, Chairman Jason Smith, and Reps. Adrian Smith, Kevin Hern, and Claudia Tenney.
“Whether it’s in my home state of Missouri or eastern North Carolina, rural communities are facing a health care crisis,” Chairman Smith said. “Today we heard from health care providers and local leaders about the struggles their communities face ranging from patients traveling long distances to receive emergency care to health facilities finding and keeping a quality health care workforce with the scarce resources available. On our current path, access to health care for a huge portion of America will continue to erode, putting the health of millions more rural Americans at risk. The Ways and Means Committee will take what we learned today from patients and doctors on the frontlines of this crisis and use it to inform the best way to expand access to health care in rural communities.”

Committee members and county leaders started the day by visiting Belhaven before touring ECU Health Beaufort Hospital, built in 1957 under the Hill-Burton Act that provided federal funding to support rural hospitals. There, committee members joined a roundtable conversation with ECU Health leaders and Beaufort County community leaders about the importance of finding collaborative solutions to the complex rural health care challenge.
The day concluded with committee members visiting ECU Health Medical Center in Greenville, a state-of-the-art academic facility that delivers high-level care to residents of eastern North Carolina. ECU Health Medical Center is the only Level I trauma center east of Raleigh, showcasing ECU Health’s unique system of care that serves as a national model for providing high-quality rural health care.
“Chairman Smith has been gracious enough to organize field hearings in the country this year on various issues,” said Rep. Murphy. “I am glad to have him and other members of the Ways and Means Committee spend time in eastern North Carolina to look at rural health care. We had the opportunity to witness firsthand the efforts of clinicians striving for quality in medicine while ensuring access to care for all.”
Throughout the tours, lawmakers walked through the emergency departments, intensive care units and labor and delivery units and engaged in conversations with clinicians regarding the challenges faced by rural health care, the aging infrastructure and the difficulties associated with sustaining essential services. Leaders discussed the importance of preserving services such as labor and delivery units within ECU Health, which are a lifeline for expectant mothers, providing essential access to safe and skilled maternity care, often in regions where other health care options are limited. Maintaining units like these ensures that rural families do not have to endure the significant burden of traveling long distances to access critical services.
“ECU Health has long advocated for solutions at the state and national level to combat the intensifying rural health care crisis facing America,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University. “We are pleased legislators not only recognize the need to explore solutions to maintain rural health care, but also recognize ECU Health as a leading voice on this important topic. The visit to Beaufort County and Greenville gave us an opportunity to show our mission in action, and we are deeply appreciative of the committee for spending time with us discussing rural health care.”
![§êÌ4 VYz½5Ñkã$¿òq³'Ô[¢veÐÆï¤DB³§ÍÐW28ø`Ò1ñMçÚíäuÓ@£CND£1-æ!^ÆÞkÝõW_N1´c§¨kO½Fa îÒú4¶
æÒÉöµTñÕx|9d!ÞÊ"Q¸m^ÚNmtx9* ô" NÙ$ßáÝ£MG*ðn@Ò|NÎ9*º··¿e´Jy¿#@ÁAb+ïLÇÕ
Q2¼×Íú3AtÆÅY-áªÛíäøåXynÇ4wÙ :üñÆ©RGFVé_[á¡ÿÖU¿.`tæ0ñ_ã,KÏ|ýes§kQiz|+Ís=NåØòýe$M'KÐN5YÒ;pL¬~Ñ¥@Rx|Ãåv9;(ãl£ÈúGÔ4·´îK V«/"U·§ÚæX.¼H¶ÑóRêYAøØ(B3Õ¸DÈÈö¦Y×$nåXøÅs&V(±)SRkkdI¤M*H
Y~t#¶S>lâU~¦é**Àl<r²È1åó74ëK{(áµAgÉÞI#äKP¨¯*{e' %Ø)æõK3ë[Å2TW&Ë!H¥Ó¦Iã¡Ûy?æºÍ¯ssÉé7²¸åô×12`â2ý.F<ÕQ®lf/0k¯ª=^2Æ1â(ÁJyoϦðÀ7|C³ H_ILE׿ßùæ®bÛwK¢ó&¿q¨Maos@HqÀµ7© wË#K)ÄsD¿4-ÊÅqºìyãZmCL£µn±%½²9-ÌOõÈXM"ó(Ì8üPTøä±â]"cÓv/uí[ñ¡ã¦Ï(wjPWímøµä¹³Ý¥^ZEÁÓþ59dy|ÃmF=9d/ á@Ì:åpÕBÏÙ.ÒîmfÄûàZC-ÅØ°4?:ò²L)ÛÉþ!¢ãÐõÉHòoÅV:°??*VNÎÐ+w5¦dc<L3a1×µ{ÚÎÚ^ÚÔBÑÆܨ§L8¨nQÕOÿ×}ªß}pZâQ³ÇǹíPs:ZQÍ×EkÚJùÙ3z(0Iô
M[5ú%#¨èÊL6s#[м¤Íyk4ìÆBÒ¸æv¨SÄ~2áË+>l
lW¾Q -õ86)Z£ü¬¤@ÓÂq£ ]>":¬¯O dOÔËøS¨£BMk½r¹óH^a^2²Ì0^ÿêZúÁY7§"§ÃžéBzµÓÆC·Ãb°´
!»D v éDP§]2L(¥d.ôÅ:b~bÚÂöWìT3#Eĸ5^FbæêÛêkß-i1ÝÁYçXÌãÈ19D£éG¥dN¹M6Çt8y¾ýiMäýiXóý!Óº°%'â|ÎÁ¢Ã&´F< ñú¢ÇµKÍBö[Û빺ÕåsSOࣲ¯Â¹¶§TM¥RÆÖ¬~d%ij'ùÒÎÅô ¾e·6!Uû@þñsW³±cþ:çÃ_¿ø¤ÃT×5mPúß¹Cö6áÑÛ½ßÿÐù×ÍóhÓ[gPyË)ÐúÍL<l[ϯ/äÔ¦ÊUfÚGU new)é~MÊÚ¬m7Z!ÏÕy]ÆXzwâ5ªÊëýâ·üy@â!»e9̼bº|iäãõÐÊyDÛmºäLX6HÛdU%~½Ì~¬ZäiØ-{M'êÈ©ð§l²/~¹ sHyGæuÓWz=
ÙÚ0#ýÐÉãñÿkíxdKt");ü°o0i×Zl³Q¬]f?ÅDí·óWøå"¨R¢l$×þqÔtZîæ-FHÄ=O#BKMò¹nYOMò®uÝ'N¼Bfæ[yÈ'º'¦Ôʧµ2wég]°´°_?¥tÍHÿëLÇÏȳÃõ=Ç×t8S¬Tñôù-GÏ*#Ò@ÛÚÿ¤ÇQ±9PíìÁou]#Í׳TG$íâ+ñ7WîËñs,rdÐOÝÔsÄA¢R¬;G5]¶lEÉìáÍ¥²^^ê6²AÊÆÖ{¾U$ÙÄdÿ¨9¾ÿðþ|ÞvV qKù¡ÂÖd1vðÌ¿6y£Ì`êºMª´è#û*йR9þÏÚ9N ¾g_¡ùßTÒì¿@ÉtÇC¸9&½ í$uû ûÅû-ö¾×Ú®Pú¬"Ãmæ©5·ú«pEÎ0 !¤PXÐ|&µ4Z¸GL¤G¿Ódñý êÞe·]fÓHk«K{%#-ÁûM²9NÑâ þ&P÷2þkÐuÏ?ÛùGË$EgÕf-´/Ñ@3IàgöÛáÍîÜéòß5y_[ÛëËÉîòåÜ]ÊwbRÿ*Ï4nÓÏ&ù¿UÓR[b7¸²°lĸ|~8öÿegJ% zd£/úªzæ&³®ÌI_®?ÝEö#E²*ñí¶npÆPu9 <ÒöÔç/kX×õÈi'®VY
rTÔ¬²O4]JVs m¨¯b3(mÆ_ÿÑåk¹kú3o¬Ê½Ê/à¹3r%¢á1ëPûäJSXG)=;0MÞÇ¢Î2169«ùkÏ6÷¢ÂjÆöÞVäÔGï,2/òÇ!@ÿ³pÊ"AÿU¿)<@sú¿£'¡¸øÌ°ÃrJëjAgb''¹sePyfho&UÒåNcýzdIl«j]§ þ¤ò?v¦U(KFëÆ´È Ý_1ëz§¯æI§äY¥jíË érFÛ3ïÉ]yí<ÙqjÌU.m%§J£ÐýcæÃ''j¼qÉ3ÊJÈ*»Ðnj2¶W³Ù¿ 59[OôxîZdcÝÌ,¦Ô^°¼P¼Rº?kß+¶MÄyÿµ}?êÚ6U ©âMTÐ7NlÄ=a1E·¦1ÖËñȤ'øÊj«21ØR}dy<§Í0¥Ï%Inn¹óÓ ÔaRúC%7vZU·`ÖX+ƵÜBv&¯íG)#ÎRámÒKJG¢Où»æ?ðç,¼±jôÔu gÔåhÆw¿ñþ?ßIN,CDG(U)#üO~æå!v â³¹½K6ÀrM22KÖüÑ®7¼¥mgæB.,Èôû}£OòóAæsþO«úÓþÿÅ;èfü®aûÌÓÿþkÉ }BíaæÅ¥5RI ~ÓÖ¿ñ¶n¡Ø:9HgrÉ5/0ÞjS¸WÄ«yI(¿«2âE²m*FkÈ@·@ÝkC@©u±fåÍ!äyÂþÏß×.Ä:µä^¯Z3 4JH{o1TRyr¹3~¦ùYJe¤Üà«/&ÈsÿÒämhíµíGn6Þ»èd!,Ì DÓ îJUþ$G¾?²N¶ÐôÛ/£[¹Ü@2Àñ5ëÓ+ÈLbHæÛRòzoéÛh,Ù[E¼GuaÌF*9n¨JýVî¥Âù´ô#_ë×zÚö»h°ÔÓ-@!äã,ªßgû)Ù6åÑÕ@ ú²'ÝCõ ò1ã²w^JÈ´æÐõß=LçFF·ë¶ñ7ôã§Âð?Õ=2AÇ1=ÌfòfPú£±øO,³HÝñÈÖϵm{=] ¿S£hÜIý ¶ea¸#(É®©¯®å²óN¬CuFKi:·ÝÎÌsLÐX[Üë%Y-TÕ·:t+[>÷»þKy'_Ó§Z»·úµ¥Ýej£*üÕyW¦bd³0z/ãRñJÓ]²ËqX極½ÕêHÿ^¡PH*½ËNê;æ6|qÜõoÅVDÑB&Ï¡hã$vÙwýx"}!¢²qá
'¬ú^#öÑzÄóÎEÎ/.iÖ1$)ªjÖÑÜøu¬Z©,Q9D¿ÿH±Í2 Gó)ç¯5Mæ8_êåÕKzzvñ|1ö{ÉþÏ6½@ů¤hÚ-÷,?^ ¤2![[ÜyÒk&{ÆZs¢ÔììþÇ(ÕÈf>W§ênÓ@þêUæM[Qó6½uyRÝ "B)!öKÇo)Ãbn«Ps϶þÿ6*hvü»ßónfâ»U6¶y;ÌÄÉÛlº,/J·YaY@6ñ¸%HûmMþjË!#äÆR
Ô$+HòDýOðÌE«Çs°ñ$ÒÒµ½ÈuÛ%Ú%V,iQ÷ä¢Ç*,ÂÞ[åd²Ltuå3V{ääÙoÿÓåÿvù¥½9%¼ZtõQ¿98µF|DéË)Zw]ËdÂÓPT´¼©$knÿËûÀdéOµW%Å|ÑîDé÷$I$ÇÐiJ¡9ƽía[¤Ì}aç¼Ñæ·µyM±;"6<ùÄÒHåðû´ÿdßäãÆ@:Ä·äÆb"zLqEª@§P¸QÈ;(è;3×æË ÐèqDâ! õH^gþz?õÌÌdþqsÍ÷eMîé{NÌÛÈ^hòõç ±Ò¹ÓY-æâÄHÊUç@fõQþ3c$-F'@Éy×Ìi¬ù½(âT².!RuST¯Òî}>ÖdÝ$7_(9Bhm¢®«ûÔÜéQ±ÉÒ D¼L>Ì®>ãúÆ ¼cóÿZý©yX»ótîußh} vÿ*UÌ}Dµæ;%!XȽ=mðÛN/,í#´hï8þÔv?~eÄp¹HÜL!´¦¸zásA]éóÊçà ó§ïü·æy4[×æÐÃÄÒ£àOÿ¢ËP°$`ÙrUÙëÜ(¥®LÂÎùYdè*Û8#½øóݲ/ÿÔäs×#Öõ»R(M¼s¤Aab ^(î=Æg4F$ØܱñqEì+÷bè«JiÀñZÓ¬¿ËRÛêw:mêÒé²YÚÌ×/»TzËéDárR>>¹®Ê9JGéÙÂG68cV>/ô¿ÂõA>:Èéy%ÅÇr`hÔ°©'lÐë! HÏð»)"#ÃÉ'ó]ü¯} (T·/³ÛlÂÓâGúÎNrx¹çþOý";fë[ÁᯱÕi¼QvüÁ¹ºW+úZmØøåý,'úÍ*Ê?ªÁ^Y§y%K$ z£áOPñ^Göy6EÕݧ>Y§ÖôÛZFææy4`8F§_Ùm± E¦£O´t«H¬tûk(+hÒ$g5b¨(*E3Zåpm°¡á¿~m¸ÈË4ëéÙ^)üFbäæ¬DÐzÑ®nUA:Ð$ïL9QR¶Ôɧ#jýù2¤'"@êèp0ÿç!tÍOVóMÕcåm¤i]ÝÊkÅ¿*WùØGð®ei2ñçÑZþÕ>{æÀqÐ>lXH¬vNCY´=bÏC×µ©àhíÁdF^_"W°âE>#_ÙûY9ÇüN~r<RûW§þ%ÝÌW)ɨÿ¦ì;ì¤C$G%{¥»±3DI¡¹òYÇäVjx1»¶2;&zµåO©Z©ÝHÞ¹<»53/ʨ[éZÏîxÇueÊ8¥xÀ1Ú²}øÁ2$Û³ÒDQ=ÌG_×õ1jÒëz³î.(¾+Â5éð 9±Çºu*¢Ó¸ãï±1S»·¾<ÒwÀT4ªYÀI¦S&qe¤PD!or@Ìkm§ÿÕás3Mé§Pîݼ>YcZáCLiWðä¤c%£òÓK¿´óïjðúð³Bd]N%OLÑöQ,fñ;®ÎÅ(dõôþ§§Ä@yþqÿÐϽÊf¶+μüknz·~-gbÜëÐó=®}þhý*:^OË¿0_ºÊoC8ªG§HTl]å2o$ÿ7ýóÅB¿¥ùsgëù»AE&ò'úó?äô¢?Sëø[á_Í;l(ycµ¹óôn¼I¤©îadúË>¦4`íiv¸1²ÍÀ1âM:áD¥FÂÑ'Õ¥ÃÛjc1ljÂ|²y¤z"0e4øR85 %T¡å_ø.Y9©³.£®ôýYE5¼Ñ´¡KsP¿:Ó24Ó¾Y¡=jSóD7ÓiãI¸æÝÌ|3éµý-×ífôån´@Ý=3Eü²Ó,4M4kÞ¡kÎW?²¯+eÿ)TÚÌs+-£ÌÎ/ÊrýÚ_(Å1ëéûÿÅñ³æk(Ë]ÄÒRõíã'Svcæh CËô Æ×Ì·Ýbâ¤Ò´®ù Ù#`º+yáÛd²2¼áÒ, ¯×½3/Í¢ye úK^¦7Åuùx_sA7ï`0%¹lGHÄ(%a{Éô/ééd·ImÉHV@ݺ×ÍiW2ÔQó{HÞ@!?ݳ%¯bGÅ2Ë+ÙÉ8õJnü¹u<wRFn¥5=iO÷êÌØrMô[hÕj{dk#uÑùqCWÕð8miº@nÿÆÑH{Í.që+Ô+Jÿíeº©_¥§nc?t?KÑ ´º½=ÁäHOÊÓýÕÂYü<RÿsêvØ2pcâû¿CåéA©H¿³îµöW#7úÑAf·ÛxÌÁ Âäxûk_Ãa´.28uEAðømúï%<äú
$N.:2î§øØqVÅÄ«Ý¢@hõelÁMc©)ZSz|ò5Ñ<][1
ÆjOÉDéïéÎÓÇÄÄÈvo#¡äFÃáÐÿÿ×ä_òBbÕ?+}Ê¿Epê
ÀÓ¡ dæOé=ìïð BÈäxþ×NMKUAÄw`¨ I=®òX£t^ÞKYï,n-àhd'E%ÜËÖ¹Xª'ȳÈéGï{o=ózÀT¢÷¬?â+Ù+á«ó9Qí`½¶y²×z#<§ÍnüÏtõ·Ä¦µ@~ë4c}Ï/¬7WË~ÓþP¶xtØát1²ÆëÄYµþ®ÔúOOõGêÌ#ÉÊêÊ-Y~¯ÿ!VkÜ5ÜîÓL®L¢F±dQ·r0!¯¯ZýêÁR¸êv¬«
êº
¼ª«~À~ÉÓs-¹;q#½ì1&Ì[+EA_ǦdåjÇ+.)*þ#¸Ëþbk2ÜYÙØÀ4v9@Áòª8£)èËþ)ÚáiLåÅçý1ÿ|ùãÏ$Ú-õ¤ß¹Ô-EЮôríÈoþIL¾98÷ºøiÅ<s3TùCØ2!ml$«P|N<@Þ(³Í8±Dhçd)¦Êµ§ãiż¦÷©Æe#äs;/0ãcä[qD¨9gF´<jDORÈÒ[=0Q®LÂè¨Ç`EkáQyžÓé5;Ï)'Gaá[hÿÐàeÌ×@#/ð«ÕÛlÉ!eÌ!E¸UQ¹' s°ùÉÖÚ=º^^F²j;Aý÷þfÌlâ÷2ý¡2 3ö
GãJ,ÁI|ÍäHî¯4Y&;µ©7_
½¾ÎRqǸ9ÔËaÇÊÚb4aI ®PrDtsÞ×GäË×qX[c]ã?ǬÓÌÚe¶ÜG¬1ÕArà³'&¦5N¯Úí´^ð/òY>«áàâfó¯Î0Çg£Ü¡·&ÝÜvG¯û(Êåzy¬ÏHy,¯J£¶e8Ìà:Tø+"ókQ·/Ëðbv/Bógí<µsi¦Ûô8eV5ç3ý¹píz77&'}H=ó7&î<wɳü«)Ûj; 4i,Ùr¹2%Ik*ê§1æ,6ÇGõPU¶ÌqoÏÿÑä^sò¾[Ö@(_N¸~vïA½Lu?áýOMN;ýIÍUÑ3ò·Zês`µjBC)ïþÀ~9~YíM@=J ëê[Nô 4òq±2G}tDEFöøZ@[J9mÝå5nl+íMPõ»ô"ÃÚÖ¿!Ôå4òÛëÞ[þÒn?0N©+ÖÀZ´k@)áQUäâ@ÎÞÁeujmô;ñ?Ó1ñE¶eåhߣ¼ós¯-½ºiaAeW£uç»W2É@Dêúmõµå¤wÕx¤è}ÆÄf)³u§i!à;`BâF0¬õ[Ýr*³Õ~ø¤ò·"+_U-Õg1+hǪþÓoòsc§¥ÃÊwGh5½+m#ÖGù·öfyqH+h upæI_âD5Øffè6_©çºL©?õiuÀTqßüÌé@õppg<`úKú^÷ª?:×B£9cõÎ6òO1ù_VÒP·1¯¦àG©V²XÏq9vHòÆ´?êô¦ß~7U¤dJB×sM².Imh.e.â5b(M7ö9i²1)K'ï)Ú+tÛÿÒçíPó ÂÐÁ(¹ü¸©{që×5}L!.nË>H ô4éZuµ
P1$SmËoüÇ6²$V[1'$S«sÂ?|¼lÍFÝ^Áf??isYwQPãeZíáÓ)rú'mÿ6
Ðh¸õýõ¿ßËx5ð´æ`HãJtÉD© g,xÈî:à[ÁH"¢$R¶À¨K¹ l0Rä)×|PWÚ
Aup±s¨N[VpR@'Õ|ÿ¢ÙÜ ^S?°ã1~Lüæ§mæ]:ÿPµ?ZN39!M?-FNgæËbáÃ÷¤jvþôíÀg$¤z¡®Zhë˲²×è9²Ä=!ÁÉvóémmc×nµ8'KÉ¡BÔ²AíÆ^|æQáîFGe9,H/Ôu[»2êÕËAâ¤uÌhósä<HÔ7ÍuLlmJ§
dt?ª¹Ld6}Qä@]ùwIºÿZÂ[æPWñÄìXôBùÛJêkdrDÁÖ#údL-/såZÇ-¸<ÅVQ³)ùÊy× 63}äM6 Kr;})fêÄbèË*A#¨fjç¦Z÷ýÆw*éZFês5©c¹ûÏL¥õBIù42::§eùü+ÿd°ÆíSTÂ82ÉVï×èï»M¿ÿÓ-óÜH°§#ñRiß-:lCCsä«)·/ 鶱(Smj¼Í7¬òû_ì²ÌâÌbl°JÐCSl(QbPåS;&«_M¶±
uWDÅk¿~¦È wX¶ãÌzXÜJHÿUBßÌÚh;sû¿®C?N+±àa³-ÑÑy¡Ù[~½*ÃøbT|Çv÷AD(µ=jNq'ë«Üð ñ ÃKn:¥Å*@ößêwŨ³;A!òíó9öär5²mr¬|$¨zFè`Ã$&Ò{+M¨/gàvxкË|AüØËùÅ»m?Nâa²ÝÐ"PoAÇP8¯©ëzÕÐku+|±>f¿ªÏ.q.CúÌÚÃJV,å¹5ù×-CFÔuM=-ìn.nc8ÝRÀëâïfó-8KFBÚXËeÒäÊZ&£ÉLs<ñ|=Agg¿àrX'ë!Ǥ¼þR]#éßñPòVQú³"|ÚC%ó!õ µ¸äø!"xVA¹C¿Ëý¬¸rAPÚ*z It`:`ºZ´-3-½½º¤<L´«Gìÿ.äiy:ÓL*F«ÉÇÙ}ÏóS&Cy·æ0â¦Z#7ùgàaËQ©Ö¡CXÿÔê°ù?È×zj¶öM2Eë¡ÝIB¼¾É4éGJEEy§@Òοqé¼½#¿¦´ü3UªÔçj1¸ÿ9ÎÓàÅ()z»ÔÒáCĶÚÆ.vû=ëCmfÚà
§|)2M4ß/ê÷ñLKG£HhHñËãEÇ¢1óoRòÆ£dD¬X þñ*h|¥FHã1a"·µ¸1;x|'+
RÇKÔ~°¯è=+âñÉVJ¤tXNÇÜP¨~²&É©âÀ~¬[ý§)Úß2OëÂoê*v1áðÝsè6¡xéÔk%X¦§ }^V2FÎ@â1d¶ü^þoÑïèÏ@«!@ûW²øl¾2y5zsy44]Oò]T°çé'¥®ýÐÉñqxãáqægÕ+òÛ_¸ZÜ-µÌ¼ÏûÄX@ê׿@ÊdòZwåõÝ
íôRgk¸f0Drjâøä6þl®#vÁ|4Yoä^«¾VÍim.dYS¸ÒEÿfT¤ÕLó_ô?`áÒÄs@HámÚ3Ñ·1ª¢è:|H¡*Ôí!mR! ;1¤¢¡2Ä8ZM¾À¹ÉIáÞhWó>¥ëyë¶þÔái"Ç KçÝSØæAAÿÕë¾ToWÉv15¨}S®fä;óh½Ø.½|_̺³ðÛ´éDDeFÒ_ÒrV©©ØüÆDPYËÇRNXÒKw<P<duSò'|ÇÍ:³lýt9L<ÁéVoëK·ØéñLÛ )½hÿNgipØâ.«5zBkÅhAÌÒ+GE8n~ã±È¤IÒZ,^îÑFbdÁÜåâÔt((õ^ÝFb¹vÅ#W«yÝð¡ -}CC¾*¤Õ¿Ómû}تÉ)Z{ãhPâÝE¾¥VO^ǪÁXAARK´ØpsݧL*ÄõÍ[pexÑ£ý6&¿êSL3QX` ^p(Q6¯~ äÁ¾¬àcÔ%:ÝÖ©$QXS'ð·*²Ût(Þ°ÓËK-y4õVK]AD+PÕ¬M¿^,J³Ì¸j£!G
G(ÙÕªRM.CÝ8ÄfXäáucdý¡¸ú2Ðæ}EØ8û²Â«¾PÜÀÅô øPäaÍ2;#n8â<æãaÓ®Jex÷æ% ÍLê(.-áò·Sÿpóc+óÌ¢ÒÿÖ](https://www.ecuhealth.org/wp-content/uploads/2023/10/12-Edit.jpg)
By North Carolina Health Care Association
North Carolina’s hospitals and health systems provide more than just healthcare services. They also blend medical know-how with community engagement and technology to help prevent and manage chronic conditions and to address factors affecting health like access to healthy food and transportation. Learn how health systems and hospitals work with local employers, schools, faith organizations and other partners to build healthier, vibrant communities.
Five rural healthcare leaders from across the state recently came together for a virtual town hall to discuss how their hospitals and health systems are creating healthier communities. This program is part of a series hosted by the North Carolina Healthcare Association.
Here are some key takeaways from the conversation.
Hospitals help support the livelihood of rural communities.
Hospitals are pillars in their communities and support economic development by providing education and employment opportunities that create stronger, more resilient citizens. “Our approach here at Northern Regional Hospital is to be engaged in all areas of community life. We recognize, like most hospitals, that we are the largest employer in the city of Mount Airy and one of the largest in the region,” said Chris Lumsden, President and CEO of Northern Regional Hospital. Lumsden emphasized that hospitals engage in a mutually beneficial relationship with the surrounding community. “If the hospital is healthy, the community [members] in a rural community will be healthy, and vice versa.”
Penney Burlingame Deal, President and CEO of Onslow Memorial Hospital, also touched on the relationship that hospitals share with their community. “In rural settings, hospitals play a part in community resilience,” expressed Burlingame Deal. Communities can support and sustain quality health and social services by attracting and retaining well trained healthcare professionals. This can then lead to a stronger economy, which in turn supports a stronger local healthcare system. “It’s recognition of that link between rural healthcare, economic strength, and overall vitality…it’s kind of this self-perpetuating feedback loop.”
John Green, President and CEO of Iredell Health System discussed how every hospital and health system is driven by a mission and vision statement, and while each is different, they all guide people towards optimal health. More importantly, this is not always done within the four walls of the hospital. Often times, hospitals are working outside of their brick-and-mortar establishments – directly in the communities they serve – to accomplish their goals. “We do that throughout the whole community, and we do it based on the needs of each part of that community,” said Green.
To that point, Annie Carpenter, Assistant Vice President of Community Engagement at Mission Health added, “We go beyond the hospital walls with our community approaches, and not just because we serve the community, but because we are the community.”
Hospitals invest in their communities to address the unique and diverse challenges they face.
Every community is unique, so it is important that hospitals listen to the needs of their community members when developing programs and initiatives. Patrick Woodie, President and CEO of the NC Rural Center, and the moderator of this conversation, shared a saying from his years of work in rural health, “when you’ve seen one rural community, you’ve seen one rural community.” This underscores that each community is characterized by its distinct array of challenges, and they must be addressed in their own unique ways.
Todd Hickey, Chief Strategy Officer of ECU Health mentioned how ECU Health is always assessing how they can invest back into the community. They do this by donating funds to support community partners, developing initiatives aimed at improving health, and through other avenues. “We see that as a role of a good steward of healthcare in a community, but also recognizing that it’s our partnerships that really connect our services to our patients, and if you will, our population,” said Hickey.
Hospitals also play a big role in strengthening the local workforce. Chris Lumsden noted that 85 percent of Northern Regional Hospital’s employees were raised and live within a 25-mile radius of the hospital. In addition, 85 percent of high school students that leave this area for work or college, do not return. “The message is, we have to grow our own. And that’s a theme that we have created through education assistance scholarship programs,” expressed Lumsden. To combat this, Northern Regional Hospital has stood up multiple programs that encourage students to not only pursue careers in healthcare, but to also stay and serve in their community.
Hospitals in rural communities use innovation to expand their reach and build more accessible health care.
Hospitals and health systems in rural communities are evolving with the changing landscape of health care. They are overcoming barriers to care and expanding access to care through innovative solutions, emphasizing a focus on maintaining good health for all.
Telehealth has blossomed as an accessible option to care, but internet connection can be sparse in some rural communities and hospitals are creating solutions to bridge the gap. “Working with our civic partners, counties and townships, trying to build out and create the funding through grants, through alignment of federal funding to help expand that [broadband] is a big deal,” said Todd Hickey. Hickey connects the availability to broadband with a greater opportunity for people in rural communities to get preventative care and early intervention for serious conditions.
Related to telehealth, Penney Burlingame-Deal said, “it is a great way of really thinking outside of the box and using innovation to make things happen that wouldn’t happen otherwise”. In addition, John Green touched on a need for stable internet access in all rural communities and technology training, especially for aging populations, highlighting the digital-based resources that will lead the future of health care.
Care options combatting opioid addiction are expanding and improving as well. Annie Carpenter mentioned a pilot program newly introduced to Blue Ridge Regional Hospital and Mission Hospital, where patients can receive medication-assisted treatment within the emergency department, an effective evidence-based practice to disrupt the addiction cycle. According to Carpenter, this care approach can impact the capacity and volume the health system while combatting the rise in opioid overdoses in the region.
“The community has been working together on responses at such a rapid rate to save lives. [The pilot] It’s something our partners in the community have been eager to see as well,” said Carpenter.
Launching more impactful programs that promote better health within rural communities often requires research and advocacy to accelerate the implementation of those programs. John Green mentioned at smaller rural hospitals, a detailed approach is necessary to implement new ideas in order to make the most of time and funding. It may be more difficult to find an effective solution using a trial-and-error approach. To advance new initiatives and programs, hospitals may glean successful ideas from other hospitals in areas with similar populations in communities with similar challenges, implementing what worked in the pilot program as a potential solution for their own community.
“I think research that allows us to see this is going to work, or we believe this should work is a huge difference to us,” said John Green.
Angela Lamson and Jennifer Hodgson began collaborating with Greene County Health Care nearly 20 years ago for an integrated care program to benefit patients in eastern North Carolina and provide valuable practical learning opportunities for their East Carolina University students. This began with one ECU medical family therapy student in 2006.
In the years since then, ECU’s partnership with Greene County Health Care focused on the delivery of behavioral and mental health services, in tandem with primary care visits, has flourished, including a recent high of 18 students across 12 sites.
All of the students who provide services with Greene County Health Care are rigorously trained for their position, ready to meet a variety of acute and complex needs for patients.

Collaboration is also reflected through Greene County Schools. During an appointment, a patient is informed about the integrated care model and asked if they would like immediate services or future services with a therapist on site.
Lamson said the students, in the College of Health and Human Performance based primarily in the Department of Human Development and Family Science and including the School of Social Work, have undoubtedly saved lives. Greene County Health Care CEO Melissa Torres has proof of ECU’s role in Greene County Health Care’s growth.
“For many years, ECU students were the only therapists providing mental health care in our clinics,” Torres said. “Over time, our partnership with ECU helped lay the groundwork for building our own behavioral health team. More therapists means more patients receive care.”
The first funding in 2006 came from the Kate B. Reynolds Foundation in partnership with Greene County Health Care. In 18 years, $4,105,762 has been secured and 154 students have received graduate assistantships to deliver integrated behavioral health care.
Greene County Health Care is celebrating 50 years this year and has five clinics offering medical, dental and mental health care covering a 17-county area.
Lamson, a Nancy W. Darden Distinguished Professor in HDFS and the university’s interim assistant vice chancellor for economic and community engagement, Torres and others have enjoyed seeing an uptick in the dental aspect and effectiveness in Greene and Pitt counties.
“One of our practice managers attributes the increase to three things: the students’ easy-going and approachable personalities, (Lamson’s) excellent rapport with our dental assistants and the students’ flexibility in approaching patients,” Torres said. “Our partnership with East Carolina University is a natural fit. East Carolina’s values are student-centered, inclusive and committed to service. Those values complement our mission and vision. Our mission is to provide compassionate, quality care, every day for all people. … The partnership gives ECU students an opportunity to learn about and serve their community as a whole, providing care to people who would otherwise not get the care they truly need.”
With mental health, Lamson said a major part of the development of student training focuses around an important question to patients — have you had thoughts of whether you would be better off dead?
“If you haven’t received training in how to ask that question and then what to do with the information, that can be really scary for the student and for the patient,” Lamson said. “What I have said time and again is I can promise you that our team is going to be ready to ask that question, and know what to do with the results. People need us to ask that question and many times, they want us to ask that question.”
National mental illness awareness week is Oct. 1-7. This year’s theme is “Together we care. Together we share.”
That is a fitting theme for what Lamson described as attempts locally to continue to reduce the stigma associated with discussing mental illness and suicidal thoughts.
“It needs to be a part of conversation, so we can really begin to make sure we are saving people’s lives,” Lamson said.
In 2005, ECU created the first doctoral program in the nation in medical family therapy. Many graduates have remained in eastern North Carolina for professional opportunities, which Torres said has helped patients of Greene County Health Care receive full care.
Alex Hernandez is a current ECU medical family therapy doctoral student who has embraced and benefited from his role with Greene County Health Care patients.
“Learning how the medical world works and how mental health is integrated into that world, this has been great and I’ve learned a lot, because it’s a huge learning curve,” Hernandez said. “It definitely prepares you. This is precisely what I want is doing therapy in the medical world, understanding that health is not just physical health or mental health. It is all of it together. That is what we practice and that is why we’re here.”
Seeing people collaborate and commit to this integrated care model has brought great pride to the co-creators of ECU’s medical family therapy doctoral program.
“The success of this collaboration and the integrated care services we have delivered across eastern North Carolina could not have been possible without the earliest vision and commitment of Dr. Jennifer Hodgson, and our partners, Dr. Tom Irons and Mr. Doug Smith, along with hundreds of devoted therapists, health coaches and our most current GCHC leadership,” Lamson said. “Most of all, this program could not have been possible without the patients who trusted our team for their care.”
The way Dr. Aundrea Oliver met Abby Coderre was, in Dr. Oliver’s words, “fortuitous.”
Abby was a sophomore at East Carolina University when she needed surgery for a mass in her thoracic cavity. Dr. Oliver’s colleague received the call about her situation, but couldn’t perform the diagnostic procedure on her, so Dr. Oliver was asked to step in.
“We just kept going”
At the age of nine, Abby was diagnosed with Crohn’s disease, so she was no stranger to hospitals. As she grew older, however, she began experiencing unusual symptoms.
In high school, she noticed bruising on her legs, but she attributed those to being a dancer. During the summer before her sophomore year, Abby experienced chest pain, but an initial doctor visit diagnosed her with a pulled muscle.
“The muscle relaxer the doctor prescribed didn’t help, so my sister insisted I go to the emergency department,” Abby said. “They did an x-ray and saw my esophagus was pushed off to one side, so they did a CT scan. That’s when they saw the mass in my chest.”
“Her mass was located next to her pulmonary artery and had invaded her pericardium,” Dr. Oliver said. What was supposed to be a four-hour surgery ended up taking Dr. Oliver eight hours to remove as much of the mass from Abby’s body as possible. “We tried to remove the majority of the mass and basically did a full resection.”
As a result, the doctors were able to correctly diagnose her with lymphoma and provide the right treatment.
That decision, Abby said, saved her life: “Who knows if chemo would have been able to get all of it?”
While Dr. Oliver has performed countless surgeries, she said Abby’s story sticks with her. “She was this young, vibrant college student who could have been my daughter, and her case was hard.” Dr. Oliver knew she wanted to do everything she could to help Abby. “We just kept going – we weren’t stopping until we got an answer,” Dr. Oliver said.
Abby’s recovery was, as Dr. Oliver put it, “slightly miraculous.”
“We cut through her phrenic nerve, so she shouldn’t have a voice at all. She should not be able to cough. But she still has great function.” Beyond the physical recovery, Dr. Oliver said it’s been gratifying to see Abby succeed in life: “To see her become this wonderful, exciting, vibrant caring woman and to go from being a happy college student to a mature individual – that gives in a way that I can only hope for is impressive.”
After surgery, Abby completed a two-and-a-half year chemotherapy regimen. Dr. Oliver was impressed by her commitment to her classes and studies while receiving treatment. “I was really proud of her. Whenever someone has to work twice as hard in order to achieve success, there is a greater depth of value in that education.” Dr. Oliver was doubly proud when she found out Abby wanted to be a nurse. “I was over the moon,” Dr. Oliver said. “She let me know she was interested in doing pediatric oncology, and I told her it was a perfect fit, that she was bright enough and she had the people skills to be a great nurse.”
A struggle worth the effort
Although it was challenging, Abby said it was important to her that she remain in school while undergoing treatment. “I needed to have some normalcy in my life,” she said. It became even more challenging when she transitioned to the actual nursing program. “I’d have to get chemo one day, and then the next day I’d be in the hospital as the student nurse and not the patient,” she said. “Then the next day I’d take a test.” As a result, Abby had to study extra hard and often took her notes with her to study during her chemotherapy treatment. She also took classes and tests online, even taking a few while she was in the hospital. “I took one final exam while I was in the ER, but it helped me get my mind off what was happening and gave me something else to focus on.”
Although Abby said she wondered when her cancer journey was going to be over, she advised anyone out there going through the same thing to remember it won’t last forever. “What you’re working for is worth it, no matter how hard the struggle. Just look at the end goal and do anything you can to make it good.”

Abby rang the bell to signify the end of her cancer treatment in November 2021, and when she graduated from college, she invited Dr. Oliver to the celebration.
“It’s not common to be invited to a patient’s graduation,” Dr. Oliver admitted. “To have someone years later have an important life event and say, I want you there – that means everything to me.”
Bridging two worlds
Now, Abby is a pediatric nurse working at ECU Health.
“When I first started nursing school, I didn’t want to stay in Greenville,” she shared. “But I really fell in love with the hospital. The team I was treated by was amazing, and I saw the impact they had on me as well as other kids. I couldn’t imagine working anywhere else.”
While their professional lives may not intersect much, Dr. Oliver is thrilled to have Abby as a colleague: “Abby is the perfect container for life, and she’s going to give it to a bunch of little kids who are scared life is going to be taken away from them.”
Coderre agreed that bridging the worlds of patient and nurse gives her a unique perspective that has helped her be a better nurse. “It gave me a lot of empathy toward my patients, because I know what they’re going through. I know what it feels like to be on the other side of things. I wouldn’t be half the nurse I am if I hadn’t been a patient also.”
As for Dr. Oliver, she said the value of her work has been solidified. “It’s easy to feel like what you do doesn’t matter or doesn’t have an impact. If I never have another patient like Abby Coderre – if Abby is my one Abby – then my career is complete. That was the best eight hours I could have ever spent.”
Looking back, Abby said she wouldn’t be here if not for her ECU Health team working together.
“I couldn’t say anything better about ECU Health. It’s amazing, with the best nurses and doctors.” She also holds a special place in her heart for Dr. Oliver: “She is just an amazing human being.”
In her ECU Health profile, Abby wrote that her role model is “Dr. Aundrea Oliver, the most amazing surgeon and person that has ever graced my life by saving my life.”
Health and well-being are at the very heart of creating economic vibrancy in a community. That is why Brian Floyd, chief operating officer of ECU Health and president of ECU Health Medical Center, joined a group of statewide health care leaders at the NC Chamber Health Care Conference on a panel titled “Working Together to Create Healthier Communities” on Sept. 14 in Durham.
Speaking to a packed room of health care, business, industry and government leaders from across the state, Floyd spoke about ECU Health’s unique position in eastern North Carolina as both the largest health care system and employer in the 29 county region, and the importance of maintaining high quality and high value care in rural communities.
“Thinking about the NC Chamber and what we’re here to talk about today, it’s important to remember North Carolina is the second largest rural state in the country,” said Floyd. “One-in-three people in North Carolina lives in a rural community so rural health care is a very critical and very personal endeavor. At ECU Health, we take our mission seriously to improve the health and well-being of eastern North Carolina, which is a region with some of the highest levels of poverty in the state.”

ECU Health is a leader in rural health care, Floyd said, and is constantly exploring new ways to improve access to care for rural communities. Speaking to topics such as improving mental health resources, partnering closely with schools, colleges and universities and investing in the health and well-being of team members, Floyd made it clear ECU Health’s role in the East goes far beyond just delivering health care.
“ECU Health is a health care provider, an educator and an economic engine for our 29 county region and we understand that collaboration is key to solving health care challenges,” Floyd said. “When I think about what we do, the reason we have a 974 bed hospital in a town of more than 80,000 people is because of the tremendous burden of disease in the communities we serve. Improving quality and cost is our goal and our clinical care component certainly plays a role in that, but we know that value is created by improving wellness through initiatives that tackle social determinants of health.”
Floyd was joined on the panel by Dr. Art Apolinario, board president of the N.C. Medical Society, Dr. Creagh Milford, senior vice president of retail health for CVS Health and Jennifer Sacks, associate director of the clinical operations program lead for Biogen. The panel was moderated by Gary Salamido, president and CEO of the NC Chamber.
Budget to provide critical funding for rural health care
Statement from Dr. Waldrum

Dr. Michael Waldrum
“ECU Health is grateful to legislators for their commitment to supporting rural health care with Medicaid expansion and other critical funding in the state budget. Thanks to their commitment, eastern North Carolina will receive support to improve access to care, medical education opportunities, funding for the medical examiner’s office and more. In short, this budget enables ECU Health and other rural health care providers to improve the lives of those we serve. This budget also sets the stage for innovation with NC Care which will positively transform health care delivery in rural communities across the state. I want to again express my appreciation to lawmakers in both chambers and Gov. Cooper for recognizing the extraordinary challenges facing rural health care and designing solutions that benefit the citizens of North Carolina, including making Medicaid expansion a reality. ECU Health will continue to strongly advocate for rural health care in North Carolina and remain at the forefront of creating a national academic model for rural health delivery.”
Greenville, N.C. – ECU Health and the Brody School of Medicine at East Carolina University’s Lora Joyner was recently selected as the National Bleeding Disorders Foundation (NBDF) Physical Therapist of the Year. Each year, NBDF honors those who have made significant contributions to the inheritable blood and bleeding disorders community at its annual Awards of Excellence program.
“It is an honor to be recognized for my life’s work as a physical therapist in the bleeding disorder community by fellow therapists, health care professionals, patients, families, and HTC colleagues,” said Lora Joyner, MS, PT, PCS, physical therapist and clinic manager at ECU Health Hemophilia Treatment Center (HTC). “I am grateful that my name will be associated with Donna Boone and previous award winners and recognized as a role model and mentor for current and future health care professionals in the bleeding disorder community.”

Physical Therapist of the Year, given in honor of Donna Boone, PT, honors an individual who has demonstrated service to the inheritable blood and bleeding disorders community above and beyond their daily responsibilities in an HTC PT role. This person serves as a role model for others in the physical therapy field and has a minimum of two years’ experience working with individuals with blood or bleeding disorders at an HTC. Donna Boone was a pioneer in physical therapy and bleeding disorders and served as a mentor for many professionals.
“We are proud of Lora for all of the hard work, dedication, and leadership she has put into this clinic and into our patients,” said Dr. Beng Fuh, director of pediatric hematology and oncology, “Bleeding disorders, sickle cell disease and cancer are life-changing diagnoses for patients and their families. Lora is an invaluable asset and works hard to ensure patients can live their best lives as possible after diagnosis. Lora’s passion for her patients is reflected by this well-earned achievement.”
Joyner has worked at ECU Health HTC for 32 years as a physical therapist and as the clinic manager for seven years. As HTC manager, Joyner is responsible for selecting patients for clinical trials and research, supporting transition needs of the clinic, quality improvement and writing grants and reports. As a physical therapist, Joyner is responsible for treating any muscular skeletal complications, most commonly joint or muscle bleeds. If left untreated long enough, joint/muscle bleeds can cause chronic pain, long-term joint problems and limited mobility. Joyner also facilitates safe participation in sports and physical activity of patients, including medication management, which allows patients to live an active and fulfilling life. Additionally, Lora has held leadership roles in multiple regional and national organizations. She is the currently the national chair of the physical therapy committee of the NBDF.
“When you see the joy on the face of a little one when you say ‘yes you can play baseball’ after their diagnosis, after they’ve thought they wouldn’t be able to do normal activities, that’s one of my favorite parts of my day,” Joyner said. “All parents dream that their children are able to do normal things, and I’m able to help children do that.”
ECU Health HTC is a nationally recognized comprehensive lifespan clinic with both adult and pediatric specialty services that is one of only three in North Carolina and is part of a national network of over 140 Comprehensive Hemophilia Diagnostic and Treatment Centers, which provide comprehensive specialty care to people with rare inherited bleeding disorders and their families.

