The Maynard Children’s Hospital at ECU Health Medical Center is celebrating its 10th year of offering high-quality, compassionate care in a soothing environment for patients and families in eastern North Carolina.
Dr. Matthew Ledoux, pediatrician in chief at Maynard Children’s Hospital, said the children’s hospital has immensely benefited the youngest patients in the East and made for more seamless care.
“The children’s hospital itself has given us the opportunity to grow services – we started an ECMO program, we’ve started and developed a dedicated Children’s Transport Team that flies all over the region and picks up kids and brings them back here,” Dr. Ledoux said. “The fact that we have all the subspecialty care, we have all the surgical care and generalized pediatric care here makes all the difference. It’s really a shining light in the East.”

Over the past 10 years, countless improvements have been made that have positively impacted the lives of many children and their families in eastern North Carolina. Other key expansions included the Pediatric Day Medical Unit, Pediatric Radiology Unit, and Pediatric Pharmacy among several other additions.
 Kim Crickmore, PhD, RN, senior vice president for Women’s and Children’s Hospital and Community Health Programs, said the Maynard Children’s Hospital is an integral part of health care in eastern North Carolina today. Over the last 10 years, the children’s hospital has delivered more than 37,000 babies, with more 61,000 inpatient admissions, 216,000 emergency cases, 223,000 outpatient cases and an additional 700,000 pediatric outpatient visits through the ECU pediatric outpatient center.
Kim Crickmore, PhD, RN, senior vice president for Women’s and Children’s Hospital and Community Health Programs, said the Maynard Children’s Hospital is an integral part of health care in eastern North Carolina today. Over the last 10 years, the children’s hospital has delivered more than 37,000 babies, with more 61,000 inpatient admissions, 216,000 emergency cases, 223,000 outpatient cases and an additional 700,000 pediatric outpatient visits through the ECU pediatric outpatient center.
“When we consider the impact to the region over the last 10 years, it’s really unbelievable,” Crickmore said. “It means so much to us here at the hospital that we’ve been able to provide care, primarily under one roof and unite all the services and to be the destination in eastern North Carolina for children who are sick or injured and need the specialty care we provide.”
Crickmore and Dr. Ledoux both said one of the services they are most proud of is the Children’s Transport team. The team consists of intensive-care trained nurses and respiratory therapists skilled in providing the specialty care many children need from the onset of transport to arrival at Maynard Children’s Hospital. Crickmore said it has been an intentional focus to build the program over the last five years and the program has seen many successes.
The Space
The amenities offered in the under-the-sea-themed Maynard Children’s Hospital are designed with patients and families in mind. Soothing young patients in a health care setting is no small task, but the children’s hospital is uniquely equipped to handle the challenge.
Dr. Ledoux said the community has stepped up time and again to provide resources and make donations that make a real difference for patients and families.
When thinking about his favorite area of the Maynard Children’s Hospital, Dr. Ledoux came back to the light tower, which can be seen when driving past the hospital. He said it’s a reminder of why he, and every children’s hospital team member, shows up to work every morning – to take care of the youngest patients in eastern North Carolina. He said he’s often asked what the colors on the light tower mean when people drive by at night.
“The reason is, we’re generally celebrating a child, we’re celebrating the end of a treatment, they’ve finished chemotherapy, or maybe they’ve been in the NICU for two or three months and they’re getting to go home,” Dr. Ledoux said. “We really try to make sure that the families and children get to pick the color and the time, but any time you see the color change anything different from our usual light blue, we’re celebrating a child and a family so it’s pretty exciting.”

Into the Future
Crickmore and Dr. Ledoux both said the next 10 years are something they’re looking forward to with the Maynard Children’s Hospital. They hope to continue expanding services and looking more to the region to bring specialty care closer to home for patients and families.
Dr. Ledoux said he and other physicians in the system have enjoyed their time spent in the region and the ability to help patients and bring key services closer to home for patients makes it special.
“I think the biggest thing is the distance that people have to travel,” Dr. Ledoux said. “We know that it’s a very underserved population and there’s a lot of poverty. People have challenges paying for gas or even having a car. The closer we can be to them to provide those services, the better.”
Another upcoming project that will impact pediatric patients in the East is the behavioral health hospital, slated to open in Greenville in 2025. ECU Health is partnering with Acadia Healthcare to build the state-of-the-art facility that will feature 24 inpatient beds specifically for children and adolescents with mental health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
Join us in celebrating the Maynard Children’s Hospital and all of its team members for the last 10 years of service to eastern North Carolina.
Four students in the Brody School of Medicine at East Carolina University have been named to the 2023-24 class of the North Carolina Albert Schweitzer Fellowship (NCASF) program and will spend the next year working on projects that address social factors that impact health and health care. Their projects will be completed in part at ECU Health facilities.
They are part of a class of 29 North Carolina graduate students — including two other Brody students and two students in the ECU School of Dental Medicine — representing medicine, dentistry, physical therapy, occupational therapy, public health and law.
“Schweitzer Fellows are not given a project or told to address a specific health need,” said Barbara Heffner, executive director of the N.C. Albert Schweitzer Fellowship. “They follow their passion and the needs of the community to develop innovative approaches which fill gaps in our health care system.”
Schweitzer Fellows develop and implement service projects that address the root causes of health disparities in under-resourced communities, while also fulfilling their academic responsibilities. Each project is implemented in collaboration with a community-based organization. Schweitzer Fellowships include an intensive leadership component, with fellows working closely with community and academic mentors during their fellowship year.
The ECU Schweitzer Fellows working on projects through ECU Health sites are:
Miranda Freeman and Michael Burt, Brody School of Medicine

Miranda Freeman

Michael Burt
A.C. Reid Schweitzer Fellows
Academic Mentor: Dr. Rima Panchal
Site Mentor: Dr. Margaret Clifton
Site: Palliative care unit at ECU Health Medical Center and Service League of Greenville Inpatient Hospice
Freeman and Burt are developing an end-of-life companions volunteer program to provide compassionate end-of-life companionship to palliative care patients who do not have anyone able to visit them. Volunteers will receive basic inpatient and outpatient hospice training, participate in narrative medicine workshops and will become knowledgeable advocates for the role of palliative services in modern patient care.
Freeman, a fourth-year medical student and native of Eagle Springs, said her passion for the project comes from her father’s recent cancer diagnosis.
“I saw how incredibly important it is to have support and care during scary difficult moments in life,” she said. “End of life should not have to be something individuals go through on their own. This program aims at providing more support to those at the final stages of their lives.”
Burt, a fourth-year medical student from Williamston, said the project aims to bridge a gap for a vulnerable population that deserves support.
“One group of individuals who are often not appreciated in conversations about loneliness is those who are in hospice care,” he said. “There are unfortunately many people who find themselves alone as they approach the end of their lives, and we believe they deserve the option of compassionate companionship, outside of their health care team, during this time.”
Vaishnavi Siripurapu and Elisabeth “Ella” Whitfield, Brody School of Medicine

Vaishnavi Siripurapu

Elisabeth “Ella” Whitfield
Academic Mentor: Dr. Lisa Moreno
Site Mentors: Dr. Hannah Florida, Dr. Lauren Sastre
Site: ECU Physical Medicine and Rehabilitation Inpatient Unit
Siripurapu and Whitfield are launching a cardiovascular health intervention for patients at the ECU Physical Medicine and Rehabilitation Unit focused on individualized goal setting, nutrition education, behavioral health and community support.
Siripurapu, a second-year medical student from Mooresville, said her passion for the project comes from watching her father’s diabetes journey.
“After following his journey and realizing the impact that chronic cardiovascular disease has on many people in my rural community,” she said, “I decided to pursue a project in order to address this unmet need that has manifested in my own life.”
Whitfield, a second-year medical student from Durham, said the project will address continuity in support from the hospital to home.
“During their hospital stay, patients are provided with structure, nutritional counseling and convenient healthy meals, therapy such as physical and occupational therapy, and support from hospital staff. However, upon discharge, this support structure is removed, leaving patients feeling isolated and powerless in their circumstances,” Whitfield said. “With the status quo, patients have a difficult time creating lasting change. We hope to ease this transition for CVD patients, and prevent future re-hospitalizations, by providing an abundance of supportive measures during this gap in care. We want to support individuals in a holistic way and help to empower them to feel confident in their ability to take charge of their own health journey.”
The NCASF is funded through the Blue Cross and Blue Shield of North Carolina Foundation, Delta Dental of North Carolina, Duke University School of Medicine, ECU Brody School of Medicine, North Carolina Area Health Education Centers, North Carolina Central University School of Graduate Studies, University of North Carolina School of Medicine, North Carolina Oral Health Collaborative, UNC Office of Interprofessional Education and Practice, ECU Health, Wake Forest University Health Sciences and individual donors.
NCASF began in 1994 as a local chapter of the national nonprofit, the Albert Schweitzer Fellowship, and has trained more than 600 leaders in health care. Nationally, more than 4,000 U.S Schweitzer Fellows have served individuals and communities in need and are continuing to shape health care policy and provide direct service.
Hurricane season is underway in the Atlantic and according to the Eastern Healthcare Preparedness Coalition (EHPC), it’s expected to be an active season.
The EHPC team said that while hurricanes are difficult to predict, we can all do our part to prepare for the best possible outcomes. That includes preparing yourself, your family and your home for potential storms.
“If something goes off unexpectedly and you’re unable to leave your house potentially due to flooding, do you feel like you could provide for yourself and your family, including your pets, for about 72 hours?” Stephanie Seals, disaster services specialist with EHPC, asked. “Historically, we know the rescue services aren’t able to help for about the first 72 hours, so we always recommend having enough food, water and medications at your home to take care of yourself, your family and your pets for that time.”
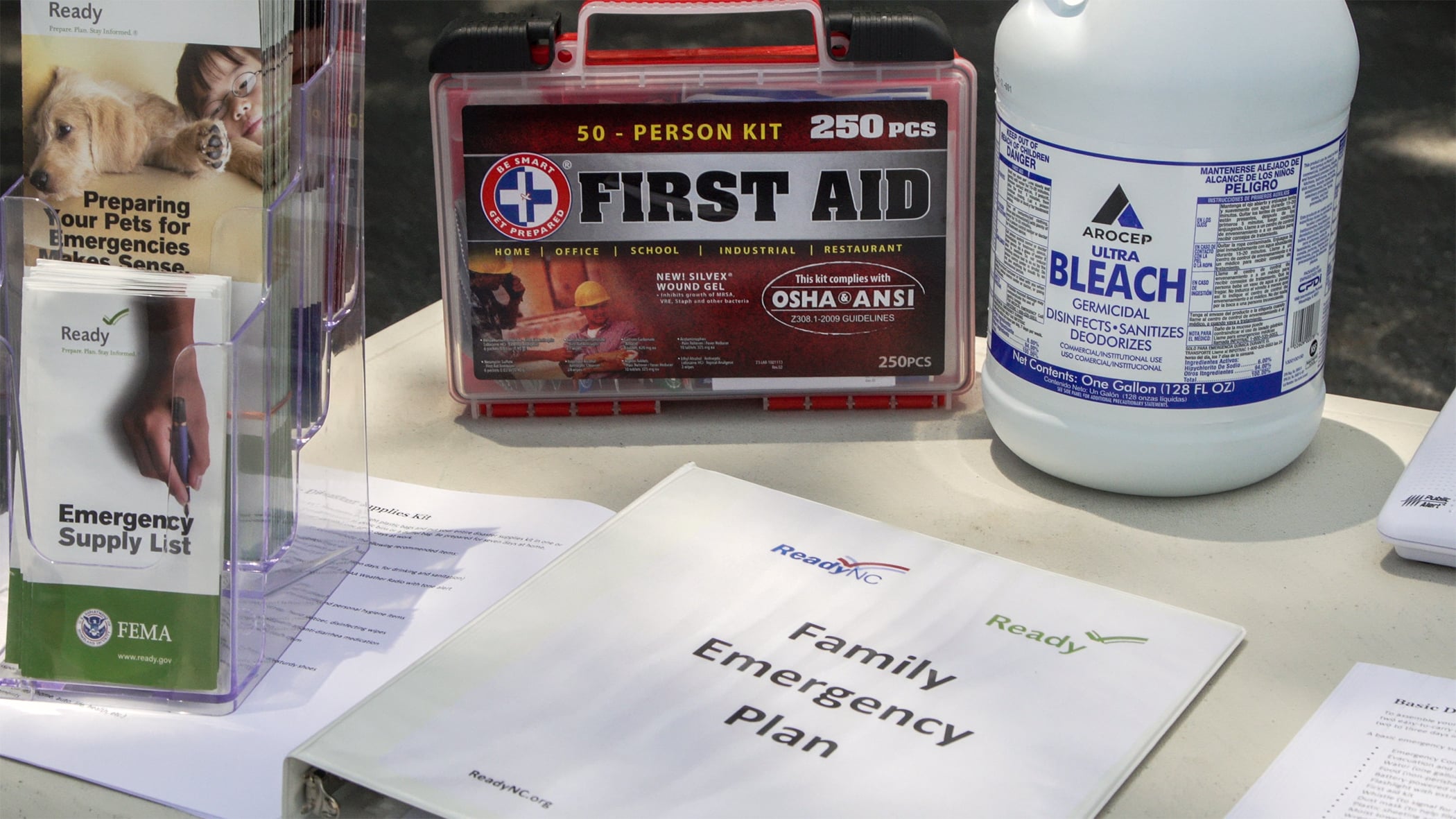
Other key items to keep in mind for your preparedness kits include important phone numbers, documents like birth certificates, marriage certificates and wills, and a first aid kit.
“You don’t necessarily have to go out and buy a brand new first aid kit, you can kind of buy your equipment and piecemeal it together yourself, but it’s important to make sure it’s stocked,” Seals said. “The big things that we see needed after these storms are things such as band aids, ace bandages and gauze to wrap up injuries and your basic antiseptic ointment to clean off those wounds.”
Ready.gov is a federal government website with helpful information about how to properly prepare for a hurricane. This includes guidance on Creating a plan that meets the specific needs of your household and building an emergency kit that contains supplies to help you stay adequately prepared for a natural disaster like a hurricane.
The EHPC team is ECU Health-based while proudly serving all of eastern North Carolina, which enables Seals to pursue her passions on both the personal and professional fronts.
“Getting to help people when they need it the most is incredibly important to me. I think helping people help themselves is one of the coolest things we get to do, too,” Seals said. “We have heard back from people that we get to train and educate and they’ll say, ‘When this happened unexpectedly, we had a house fire or another situation, I was ready because of the things that we put together.’ That just means the world to me.”
Resources
Hurricanes can form quickly. Take the time now, before a hurricane impacts our region, to educate yourself on how to prepare and respond. Below are helpful links for federal and state websites:
“I was really apprehensive about it because I’ve always been at one little hospital,” said Suzanne Foster, a travel nurse with ECU Health, “so it was a little intimidating coming to a larger hospital.”
Suzanne Foster isn’t the only nurse who found herself looking for new and different opportunities in the wake of the COVID-19 pandemic.
“I wanted to try travel, nursing and experience other facilities,” said Foster, “but I have a husband and a son that I dearly love and do not want to be away from. The fact that I can drive home at night is huge.”
She can do both thanks to the ECU Health Travel Staffing program. It’s an innovative approach to recruiting driven by the ever-changing health care industry and the need to meet nurses where they are.
“For an organization of our size to develop its own staffing agency is significant in the innovation of nursing care and staffing hospitals,” said Dennis Campbell, ECU Health Beaufort Hospital, a campus of ECU Health Medical Center interim president. “It’s no secret that there is a nationwide shortage of staff nurses and nurses are more mobile today than they have ever been.”
“I was getting a little bit burnt out in my current role, which frankly after COVID, I think a lot of us needed just a change of scenery,” Foster said.
“The travel staffing program mimics any other staffing agency. The difference is it’s ours,” said Campbell.
Since the start of the program, the system has hired more than 500 clinical team members. Of those, 89% have opted to extend their assignments.
“The team, everybody that you encounter is extremely considerate and thankful to have you on board,” Foster said. “Working at ECU Health has been wonderful.”
To learn more about the ECU Health Travel Staffing Program visit: https://careers.ecuhealth.org/pages/vidant-health-travel-staffing-program.
ECU Health, local organizations, non-profits and other behavioral health and substance use groups came together on May 23 to host the 11th annual Mental Health Expo, which was in person for the first time since 2019.
Nearly 50 exhibitors saw groups and individuals come through as they answered questions and provided information about local mental health and substance use resources.
Glenn Simpson, ECU Health system service line administrator for Behavioral Health, said the opportunity to come back together in person was crucial for the event to connect with community members face-to-face.
“Most of us become accustomed to Zoom meetings and masking and not having that interpersonal relationship. As humans, interpersonal relationships are extremely important,” Simpson said. “Technology helped us with this event the last couple years but to be able to actually see people shake people’s hands, talk to them directly is really exciting.”

The event also included speakers presenting on a few different topics, including: “Mind Over Matter: Using Mindfulness to Assist with Treatment of Depression and Anxiety,” “Lay Responder Naloxone Training: When and How to use NARCAN Nasal Spray” and “Human Trafficking: Building Protective Factors for Prevention and Resiliency.”
Simpson said these “mini workshops” were helpful to give community members more information on topics that may be important to them.
Simpson also shared that this event would not be possible without the support of the community and the many organizations that came together to share information with eastern North Carolinians.
“There is help out there, you just kind of have to figure out how to get it,” Simpson said. “This event brings the exhibitors, agencies and the public together to share all of this information. I’ve already talked to a few people and realized I didn’t even know the agency existed and I’ve been doing this for a long time. It’s a real cool opportunity to learn what’s out there and I know the communities we collectively serve really benefit from that.”
The Walter B. Jones Center, located in Greenville, was one of nearly 50 exhibitors on hand for the Mental Health Expo. Team members from the center said the partnership with ECU Health is crucial and the opportunity to connect with community members in person is invaluable.
“It’s great to get the word out and to let people know what we do and let folks know how to get into treatment and get help when they need it,” Jade Butler, counseling supervisor at Walter B. Jones Center, said. “I think we have the same vision and goal in mind as ECU Health, to help as many people as we can with mental health and substance use issues. Having ECU Health Medical Center right here and us just down the road, I think we’re able to collaborate and be able to serve as many people as we can.”
Simpson said the event was also a great opportunity to help promote the 988 Suicide & Crisis Lifeline as well, which offers 24/7 access to trained crisis counselors who can help people experiencing mental health-related distress.

The lifeline is available nationwide and connects callers with a trained professional in the state from which they are calling. North Carolina residents contacting the 988 services are connected to a team in Greenville. The lifeline offers free and confidential support and can also help callers connect with nearby services.
Access to care was a frequent topic during the Mental Health Expo and Simpson shared that Medicaid expansion is an exciting development for those seeking behavioral health care. He added that the upcoming behavioral health hospital, slated to open in Greenville in spring 2025, is a major step in improving access for eastern North Carolina.
“We’re very excited to partner with Acadia,” Simpson said. “It’s going to be a state-of-the-art behavioral health hospital that will serve all ages. That’s all on top of what we’re already able to do today so it will be from children to senior citizens that need that level of care.”
ECU Health team members were on hand to share information on family services and important topics, like setting up a Psychiatric Advance Directive. The ECU Health team also shared information on MyChart and ECU HealthNow.
At ECU Health, the support team members provide to each other makes a difference – not only to those team members but also to the patients we serve across eastern North Carolina.
Recently, three ECU Health nurses were inducted into the East Carolina University (ECU) College of Nursing Hall of Fame while another earned a scholarship as she pursues her doctorate in nursing. These four ECU Health nurses each said the support of fellow nurses has uplifted them throughout their careers and the scholarship and inductions into the Hall of Fame is a reflection of that support.
Learn more about the honorees below.
Amy Campbell
Amy Campbell, quality nurse specialist at ECU Health, has been with the system for about 18 years over two separate stops.

 Campbell started at ECU Health Medical Center as an associate degree nurse in pediatrics and said she was quickly encouraged and supported by fellow nurses and leaders to join the HomeGrown program, which helps team members go back to school and balance their work and school responsibilities, and she received her bachelor’s degree from ECU in 2001. Campbell left ECU Health to teach at Pitt Community College and ultimately returned to the health system with a master’s degree. During her second stop at ECU Health, she said she was once again supported to further her education and pursue a doctorate degree, which she completed in 2020.
Campbell started at ECU Health Medical Center as an associate degree nurse in pediatrics and said she was quickly encouraged and supported by fellow nurses and leaders to join the HomeGrown program, which helps team members go back to school and balance their work and school responsibilities, and she received her bachelor’s degree from ECU in 2001. Campbell left ECU Health to teach at Pitt Community College and ultimately returned to the health system with a master’s degree. During her second stop at ECU Health, she said she was once again supported to further her education and pursue a doctorate degree, which she completed in 2020.
“A lot of executives were so encouraging for me to get my Ph.D. and I was HomeGrown and I was able to do my research here so they really were supportive all along,” Campbell said. “I also went through the Ph.D. program with a lot of my colleagues here so that was really great, too. I couldn’t have done it if people hadn’t given me time to do my research and to go to school.”
Campbell is a Williamston native and she said the rural aspect of the care ECU Health provides for the region is close to her heart.
The close-knit communities of eastern North Carolina transfer over to the hospital setting where Campbell said it’s a family atmosphere for team members and the patients they serve.
“I believe that at ECU Health we really do rise by lifting others and people really try to make sure others get time in the spotlight, even though, if you ask any of the four of us, we really don’t like this spotlight,” Campbell said. “But for me, I’m able to embrace it because I want all those people who supported me to have their moment with me. I’m a single mom, I’ve been a single mom for 19 years, but I’ve had a wonderful family here. Everyone has always been so good and supportive of school or whatever I was going through to help me be successful.”
Angela Still
 Angela Still, senior administrator of Women’s Services at ECU Health Medical Center, said she was humbled to join her colleagues who have been inducted into the ECU College of Nursing Hall of Fame as part of the Class of 2023.
Angela Still, senior administrator of Women’s Services at ECU Health Medical Center, said she was humbled to join her colleagues who have been inducted into the ECU College of Nursing Hall of Fame as part of the Class of 2023.
Still has been with the health system for 36 years and is a 1986 graduate of ECU. As a Greenville native, Still said the opportunity to care for and support women in eastern North Carolina is special to her.
“The needs of the patients and families in our region, the disparities, and the social determinants of health are so different from what the rest of the state deals with every day,” Still said. “Our 29 counties are comparable to the size of some states but it’s rural. Access to care, access to healthy food, these are unique needs. At this point in my career I am not impacting the individual patient and family, I’m working to impact the region. It’s a population of mothers and babies that we want to be healthier because they are our future in the region.”
Still said that during her time at ECU Health, she’s been the beneficiary of great leadership and mentors and she’s been happy to give that back to the next generation of nurses as they rise through the system and across the state.
She said it’s crucial to invest time and energy into mentorship as it will make a difference for the individual, those they mentor in the future and the patients they serve.
“The opportunity to mentor people through my career has been just really amazing. I have people across the state I mentored that are not with the system anymore and they still call me to ask questions or just look for guidance,” Still said. “So just being able to make an impact on the people that are going to care for others is very special to me. We’re all eventually going to retire, so being able to mentor and guide folks that are going to be here long after I’ve left and are going to continue to carry that torch and make a difference for our communities, it’s a big deal.”
Georgia Perry
 Georgia Perry is the nurse manager on 2 North Medicine and 2 North Progressive Care at ECU Health Medical Center and was also inducted into the ECU College of Nursing Hall of Fame this year.
Georgia Perry is the nurse manager on 2 North Medicine and 2 North Progressive Care at ECU Health Medical Center and was also inducted into the ECU College of Nursing Hall of Fame this year.
Perry said the night of the induction into the Hall of Fame was special for her as she had a chance to look into the crowd gathered and see mentors, some of whom nominated Perry for the recognition.
Perry earned her bachelor’s degree from ECU in 2010 and began working at ECU Health as part of the very first New Grad Nurse Residency Program class. She started working on 2 South, became an assistant nurse manager, and eventually became the nurse manager on her current unit. She received her master’s degree in 2015 and said the backing of fellow nurses and leaders alike made going back to school a manageable task.
“I tell people all the time, if you can dream it, you can do it here,” Perry said. “I truly feel like the support system is really what makes it easy to go back to school to be able to juggle it all. There’s a wealth of mentors here, you can pick up the phone and call anybody and it doesn’t matter if it’s across service lines.”
Perry is a Newton Grove native and said working in rural medicine is important to her because she grew up in a rural area.
“I think it’s wonderful that we have such great access to really all specialties right down the road,” Perry said. “My family actually will travel and get to ECU Health Duplin Hospital and then have access to the tertiary center, so we live it. I’m really grateful for what we have here at ECU Health and I’m glad to be a piece of the impact we have on this region.”
She added that the team around her keeps her going while the patients they serve inspire her to bring her best each day.
Lauren Nichols
 Inductees into the Hall of Fame help fund a scholarship for ECU College of Nursing students. Lauren Nichols, a staff nurse on the Cardiac Intermediate Unit at ECU Health Medical Center, earned a scholarship from the fund for this year.
Inductees into the Hall of Fame help fund a scholarship for ECU College of Nursing students. Lauren Nichols, a staff nurse on the Cardiac Intermediate Unit at ECU Health Medical Center, earned a scholarship from the fund for this year.
Nichols, who has been working at ECU Health for seven years, is pursuing a doctorate in nursing with a family nurse practitioner specialty at ECU.
Nichols is from Edgecombe County and said she chose to work at ECU Health and continue her education at ECU because of the health system’s commitment to rural health care and eastern North Carolina.
“ECU Health’s mission really resonates with me,” Nichols said. “Growing up in such a rural community makes me want to do my part to help improve the health of the people of eastern North Carolina.”
She said she never doubted her decision to go back to school because of the support she has received, especially from nursing leadership.
Join the Team
ECU Health nurses make an incredible impact every day across eastern North Carolina. Learn more about opportunities to work alongside these amazing nurses and so many others here.

Trish Baise
Since my arrival to the organization in January, I have enjoyed the privilege of getting to get to know the nurses of ECU Health. I’ve visited our acute care environments and interacted with a number of ambulatory care teams. In every visit, I come away inspired by the level of nursing care that is provided on a daily basis in communities across eastern North Carolina.
This week, May 6-12, is National Nurses Week, and it is my distinct honor to recognize and celebrate the incredible contributions of our ECU Health nurses. They demonstrate the mission, vision and values of ECU Health by providing excellent care in our hospitals and clinics. Nurses also serve in other critical roles across our health system focused on improving well-being, quality, safety, outcomes and access.
All nurses, regardless of their role, have a profound connection to purpose. Our purpose might be to provide hope to the hopeless, administer life-saving care that impacts generations of a family, give the support a colleague needs at just the right time, teach the next generation of nurses or be a part of innovation that fundamentally changes health care. If we pay attention, our careers our filled with daily moments of purpose, some small, some life changing. Our nurses are joined in purpose by 4.2 million nurses nationwide. It is the tie that binds us together. Together we will build upon our shared purpose as ECU Health nurses and become a national model for nursing excellence.
During National Nurses Week and beyond, I encourage our community to take the time to celebrate each and every one of the nurses providing care for our family, friends and neighbors. Nursing is the backbone of health care, and achieving the ECU Health mission would be impossible without them.
Thank you, ECU Health nurses, for your compassion, commitment to excellence and all you do for your patients and their families every day. ECU Health, our patients and our communities all benefit because you choose to serve eastern North Carolina.
For more than 25 years, the Pediatric Asthma Program at the Maynard Children’s Hospital at ECU Health Medical Center has worked to help patients and families living with asthma lead healthy lives.
Jeanine Sharpe, social work care manager for the Pediatric Asthma Program, said the goal of the program has always been to decrease emergency department visits, reduce school absences due to asthma, provide education and improve quality of life for patients and families.
“Currently, there are about 5.1 million children under the age of 18 that have asthma in the U.S. and it’s the leading chronic disease for children,” Sharpe said. “Just for our service area last year, we had 1,687 pediatric asthma patient referrals. It’s the number one reason for school absences and the number two reason for hospital admissions for children. But we know that asthma is a controllable disease. What we find is that a lot of times the missing piece is just education.”
Sharpe said the program has touched many families over the years, whether it’s just one interaction or years of working on a family’s case. One family that has seen the impact of the program recently is the Carr family.
Dalton Carr III was diagnosed with asthma three years ago and struggled with wheezing, coughing and attacks in the years since.

Dalton III’s mother, Shanika said she was scared when her son was first diagnosed and she wasn’t sure how to handle certain situations. This past December, Dalton had an incident and was seen in the emergency department for his asthma.
“That’s when I met Ms. Sharpe,” Shanika said. “I was confused at the time, but ever since I met Ms. Sharpe, it’s been easier to learn things. I was confused with the things different doctors were telling me and I really didn’t understand how serious it was.”
Dalton III’s father, Dalton Jr., said it has been a great experience working with Sharpe and the Pediatric Asthma Program team.
He said the education and support offered have helped their son be confident and join in the everyday activities of other children his age. While he used to struggle, today he does not wheeze, cough or have flare ups from his asthma. Dalton Jr. credited the work with the Pediatric Asthma Program for this turnaround.
“She got us in a good routine for him. Ever since we’ve gotten Dalton on a consistent routine, he hasn’t had any problems,” Dalton Jr. said. “It’s even to the point where he can tell us when he needs his pump. He might say, ‘Mom or dad, I need my pump’ or ‘I’m good.’ He plays football and he’s running and tackling and it’s a lot but with Ms. Sharpe being in our lives these last few months, it’s just helped a lot.”
Dalton Jr. encouraged families to reach out for help and to learn what might work best for their child’s asthma.
Malorie Whitaker, respiratory care manager at ECU Health Medical Center, said the program is designed to help patients from one to 18 years of age feel more comfortable while they manage their asthma and participate in normal childhood activities.
She also said the program is set up to meet children where they are and eliminate barriers to care.
“Sometimes they’ll come into our office to do different testing or do some education, but usually we meet them,” Whitaker said. “So we’ll get into the homes, we’ll go into the schools, into the clinic, wherever they are. Some of these kids that we see don’t have transportation or transportation is difficult for them, so that’s why we like to go into the school or into the homes to help them.”
To learn more, or to speak with someone close to you, visit the Pediatric Asthma page or call one of the ECU Health locations offering pediatric asthma services.
- ECU Health Bertie Hospital: 252-833-2861
- ECU Health Chowan Hospital: 252-833-2861
- ECU Health Edgecombe Hospital: 252-641-7382
- ECU Health Medical Center: 252-847-6835
- ECU Health Roanoke-Chowan Hospital: 252-209-3117

Brian Floyd
ECU Health Chief Operating Officer and ECU Health Medical Center President Brian Floyd joined other rural health care leaders from across the state for a virtual town hall hosted by the North Carolina Healthcare Association on Tuesday, April 11.
During “Reimagining Rural Health in North Carolina,” Floyd and the 4 other panelists – Jessie Tucker, president and CEO at UNC Health Wayne, Kathy Bailey, president and CEO at UNC Health Blue Ridge, Lynda Stanley, President and CEO at Dosher Memorial Hospital, and Michelle Fortune, CEO at St. Luke’s Hospital – discussed how they are evolving the future of rural health care in the state.
Like many rural regions, 1.4 million people who call eastern North Carolina home face a number of systemic socioeconomic challenges, which have negative impacts on health outcomes. The panelists discussed the unique challenges rural health care faces, how Medicaid expansion will impact rural health care and communities, workforce development, community partnerships and outreach and innovations. Partnerships and collaboration were a key topic and many rural health systems across the state, including ECU Health, continue to identify solutions to improve access to care in rural communities.
“I was honored to discuss rural health care challenges, successes and innovations alongside fellow rural health leaders across North Carolina at today’s town hall,” said Floyd. “ECU Health and the Brody School of Medicine at East Carolina University are uniquely positioned to help train the next generation of physicians and health care workers. Together, we can address the issues that rural communities face like a lack of access to health care resources and disproportionate chronic illness. From community education, to partnerships that make every social system more vital, to caring for people at their worst and sometimes best day, the work we get to do is so fulfilling.”
Wildwood Park in Greenville served as the perfect setting for “Emergency Medicine Wilderness Day” as ECU Health emergency medicine residents practiced assessing and treating a variety of common outdoor ailments including altitude sickness, lightning strikes, falls from trees and more.
On March 29, approximately 20 emergency medicine residents attended training and worked in small groups to run through simulated injury scenarios with real people. From knowing how to stabilize an injured person, to assessing injuries and helping get them to safety, emergency residents worked together to treat the injuries under the watchful eye of experienced faculty members from the Brody School of Medicine at East Carolina University. Residents received real-time instruction and feedback from faculty as they worked through their training.
Standardized patients from Brody’s Office of Clinical Skills Assessment and Education acted as the patients in each scenario. Standardized patients are trained to mimic real patients so that students can learn. Their role is to help prepare future health care professionals for a variety of patient interfaces.

“There are a number of practical applications for this type of training, especially for our medical residents who get to test their knowledge in the field,” said Dr. Jennifer Bennett, an emergency medicine physician at ECU Health and clinical assistant professor of emergency medicine at Brody. “These scenarios are the types of things that we, as emergency medicine physicians, address somewhat commonly. We can apply the knowledge and skills learned out here to patient care.”
The day was a success, according to Dr. Bennett, who helped create the simulation Emergency Medicine Wilderness Day training event last year alongside Dr. Jennifer Parker-Cote, assistant professor of emergency medicine at Brody. Both doctors helped organize the Wilderness Day, coming up with unique patient scenarios, including the altitude sickness training station which featured a standardized patient acting as a distressed hiker. The residents removed a fake snake from the area, asked the patient questions about their medications and medical history, moved the patient to a lower area and helped get them to further medical care.
“It’s always nice to get outdoors instead of sitting in a lecture hall,” said emergency medicine resident Tyler Ruchti, DO. “When you’re in the hospital, you have all of your tools and all of your equipment and know where it is, and when we come out here and do things like this it’s a change of scenery. You have to think outside the box.”
The training is another example of the valued partnership between ECU Health and Brody. Residents at an academic health system like ECU Health have support and resources for continued education from faculty and the Interprofessional Clinical Simulation Program at Brody, enriching their clinical training experience. Residents are able to participate in trainings like this to prepare for real situations with real patients both behind the walls of the hospital and out in the community.
“This training was partially about simulating complex medical issues that you may encounter in the wilderness as well as providing a little wellness for our residents,” said Dr. Parker-Cote. “This is a fun way to test knowledge and work together as a team. When it comes to education, there are different modalities for teaching. Learning in this type of environment provides us another way of reinforcing the knowledge they have learned throughout their residency, and it prepares them to help their fellow community members no matter the situation.”
Resources