Greenville, NC – Sept. 3, 2021 – Moderately or severely immunocompromised community members can now schedule a third dose COVID-19 vaccine appointment through Vidant Health by calling 252-847-8000 or by visiting VidantHealth.com/Vaccinate. A third dose may prevent serious and possibly life-threatening COVID-19 in immunocompromised people who may not have responded to their initial vaccine series.
Vidant Health is closely following Centers for Disease Control (CDC) guidance to provide third doses to eligible community members. Appointments can be scheduled at Vidant Health clinics and oncology practices throughout the region for immunocompromised, eligible community members who meet the below criteria:
- You’ve had an organ or stem cell transplant
- You’re receiving chemotherapy, other treatment for cancer or tumors, taking biologic agents (Humira, Enbrel, Remicade, etc.), taking high doses of prednisone, or taking similar drugs. Many of these drugs are used for treatment of cancer, Crohn’s disease, rheumatoid arthritis, or psoriasis.
- You have a disease that weakens your immune system (like HIV or a primary immune system disease)
- Your doctor told you that you’re immunosuppressed
The third dose is recommended for immunocompromised individuals at least 28 days after their second dose of the Pfizer or Moderna vaccine and is not recommended for those who received Johnson & Johnson’s Janssen COVID-19 vaccine.
Vidant Health is following CDC guidance and is not currently offering additional doses or booster shots for any other population at this time. Please continue checking back to VidantHealth.com/Vaccinate for the latest information on Vidant’s vaccine efforts.
Local data
We continue to see a similarly troubling trend in our region, with COVID-positive hospitalizations in the Vidant Health system rising from 43 on July 17 to 169 on Aug. 30.
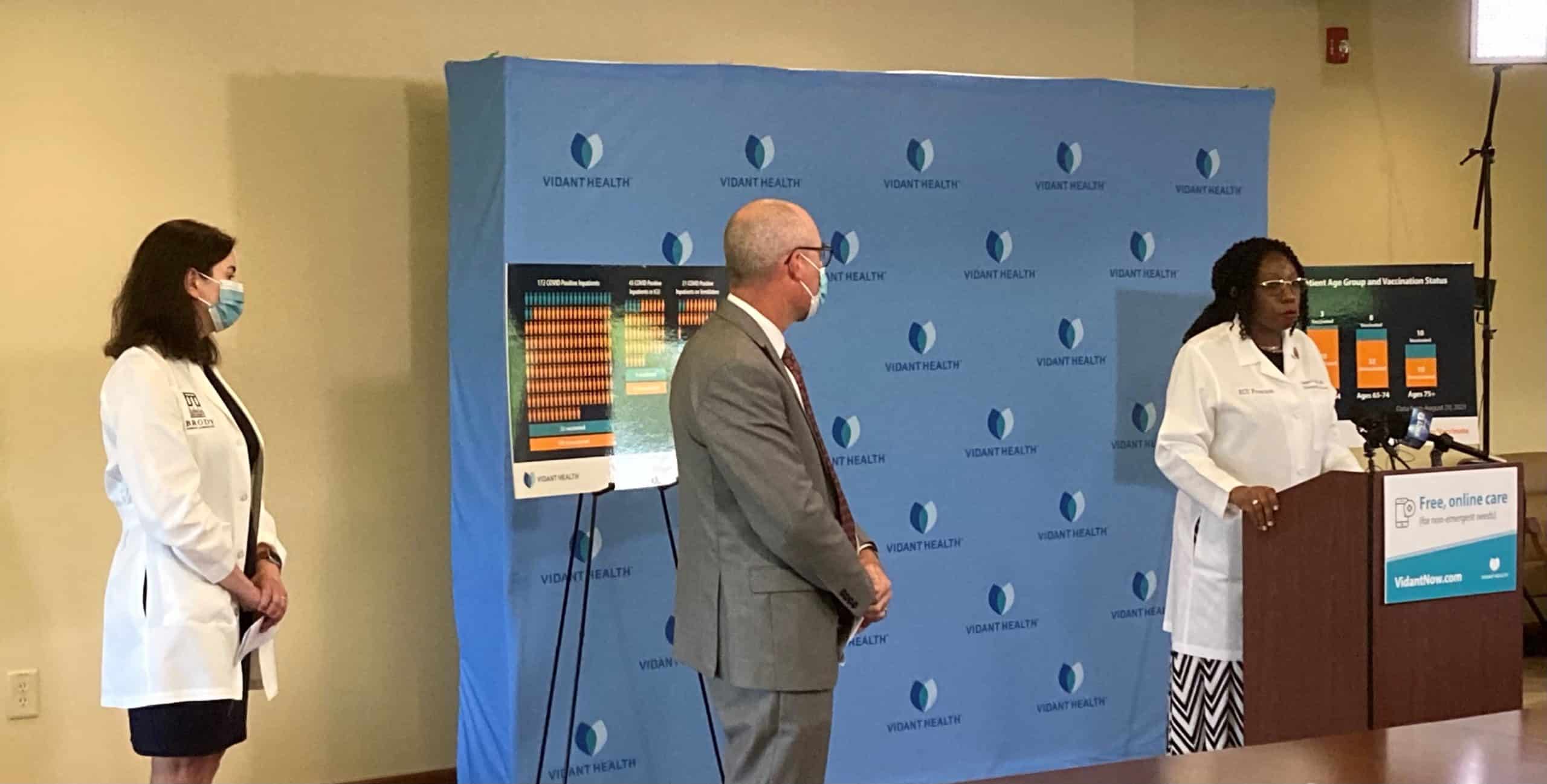
Dr. Leigh Patterson, an emergency medicine physician at ECU Health Medical Center (VMC) and ECU’s Brody School of Medicine, spoke to the media on Aug. 30 to address the recent spike in COVID-19 cases.
“We are currently seeing record numbers of patients presenting to the emergency department seeking care,” Dr. Patterson said. “We are seeing record numbers of children, more children than we have seen at any point in the pandemic up until now.”
Dr. Ogugua Obi, a critical care physician at VMC and Brody School of Medicine, said the burden of care on hospital team members is immense in the current state of COVID-19 but hospital staff continues to show up and care for a region.
“We have an excellent team of physicians and nurses – our teams are excellent, they’re first-class,” Dr. Obi said. “They’re doing all that they can to take care of our critically ill patients, but we are exhausted. We are seeing more death and suffering in our ICUs than we have ever seen before.”
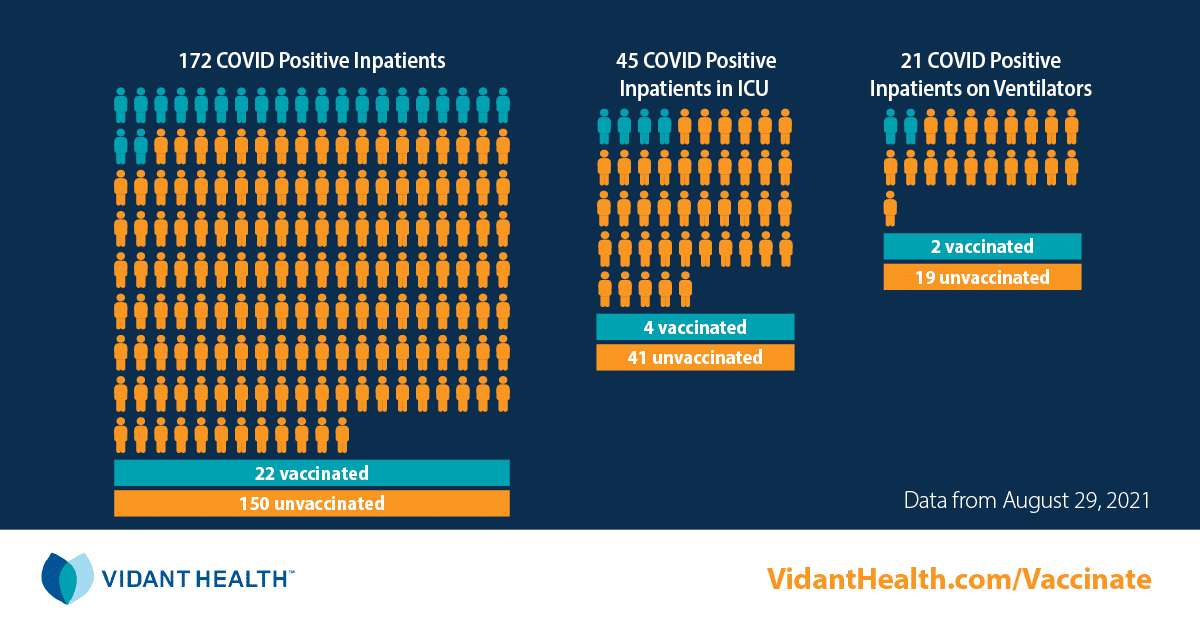
The data continues to show that the vaccines are effective at lessening the severity and impact of this virus.
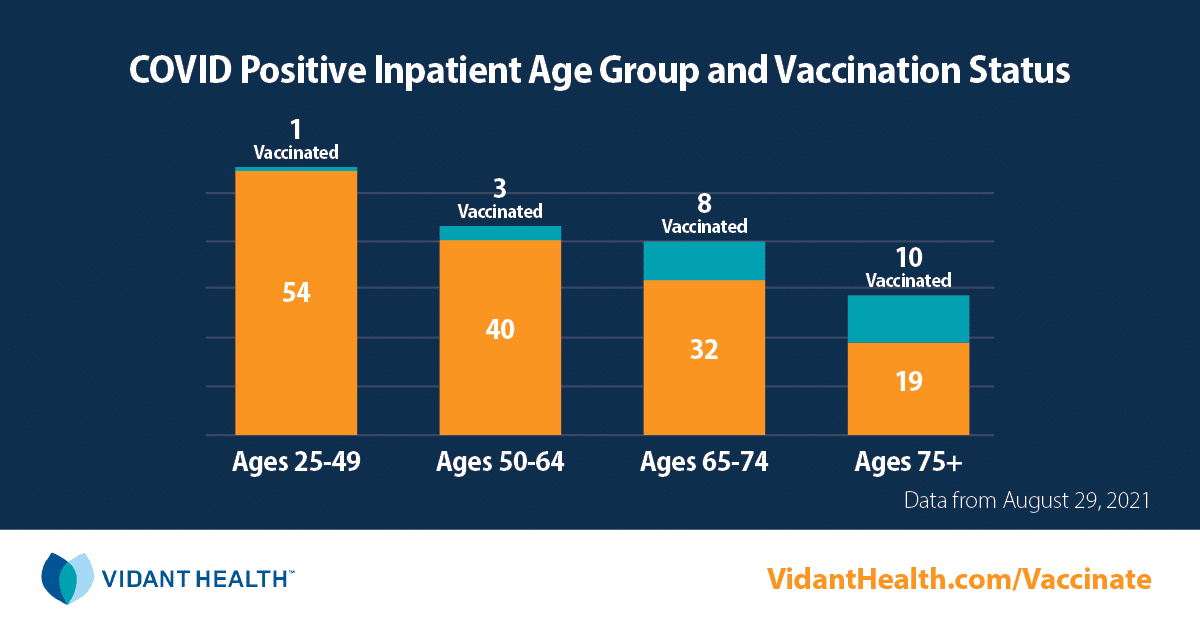
On Aug. 29, 87 percent of those hospitalized in a Vidant hospital were not vaccinated. Of those in the Vidant system on Aug. 29, 45 COVID-positive patients were in the ICU with 21 on ventilators. Only two of those patients on ventilators were fully vaccinated. Vidant has had no patients hospitalized due to reactions from the vaccine. The vaccine is available to everyone age 12 and older and appointments can be found at VidantHealth.com/Vaccinate.
According to the North Carolina Department of Health and Human Safety, as of Aug. 30, 65 percent of North Carolinians 18 or older have received at least one dose of a COVID-19 vaccine and 60 percent are fully vaccinated.
Get vaccinated today
Dr. Obi asked that everyone do their part to help slow this pandemic and take a COVID-19 vaccine if you are able.
“We know the vaccines are safe, we know the vaccines are effective and the vaccines are very readily available here in eastern North Carolina,” Dr. Obi said. “Please take the vaccine. Take the vaccine to protect yourself, take the vaccine to protect your family, take the vaccine to protect your loved ones, take the vaccine to protect our staff, take the vaccine to protect our nurses, take the vaccine to protect our physicians. Help us take care of all of eastern North Carolina.”
Dr. Matthew Ledoux, a pediatrician at VMC and Brody School of Medicine, reiterated messages that have been important to slowing the spread of COVID-19 since the very beginning of community spread:
- Wear a mask when in public
- Get tested for COVID-19
- Get your COVID-19 vaccine
Watch a recap of Monday’s press conference:
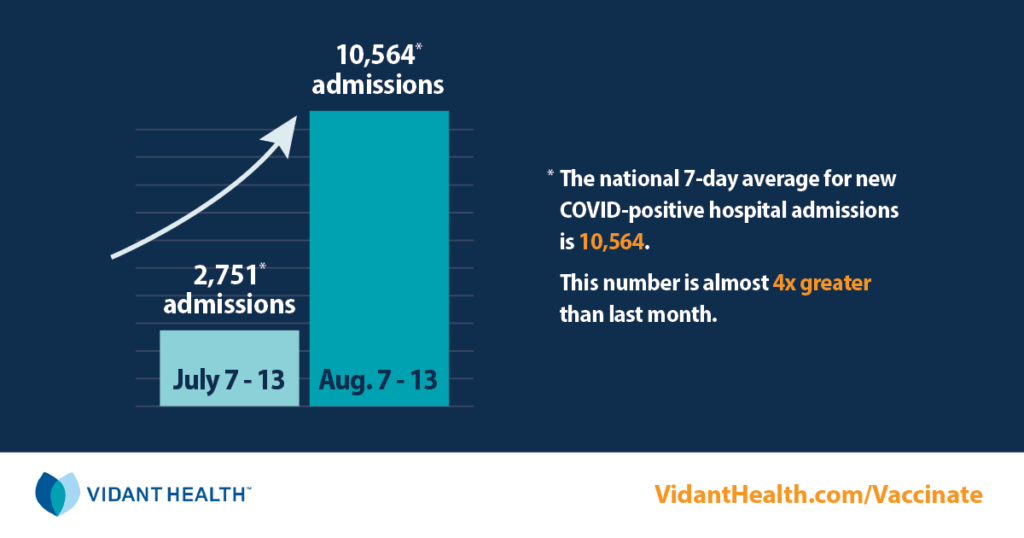
As of Aug. 18, there were 2,930 COVID-positive hospitalizations in North Carolina. This is up from 623 just one month ago—a 370 percent increase. In addition, Aug. 17 had the highest COVID-related ED visits across the state since the pandemic started in early 2020.
Local data
We continue to see a similarly-troubling trend in our region, with hospitalizations in the Vidant Health system rising from 34 on July 17 to more than 123 on Aug. 17. The 29 counties Vidant serves are currently the highest in the state for the seven-day moving average for COVID-19 hospitalizations.
“We were in a pretty good place,” Vidant Chief Medical Officer Dr. Niti Armistead said. “The transmission had slowed down, more and more people were getting vaccinated and protected, hospitalization days started to really come down, number of cases started to come down and many of us thought we were just in the last leg of this marathon. What changed was the vaccination rates just hit a wall.”
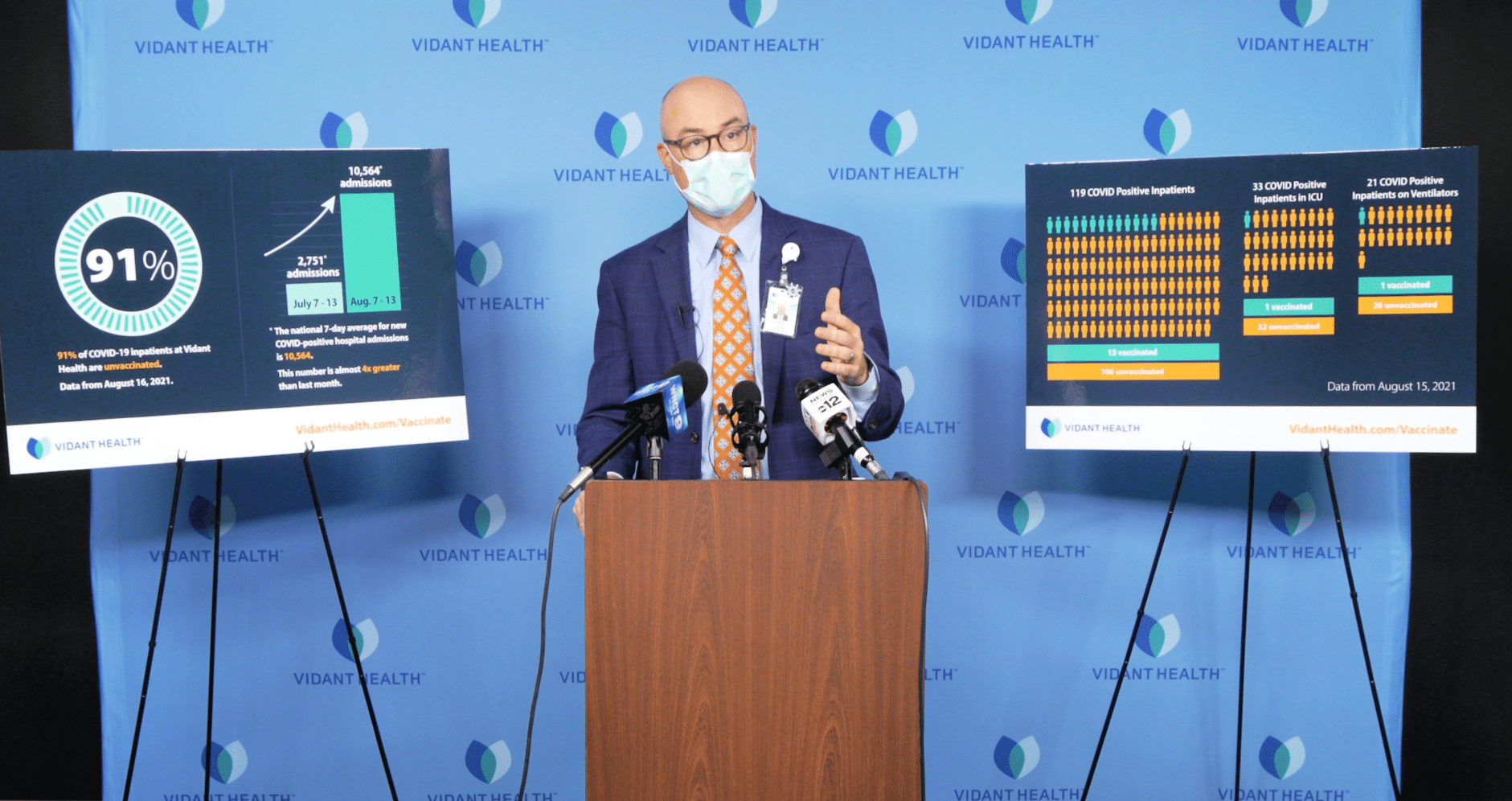
The data continues to show that the vaccines are effective at lessening the severity and impact of this virus.
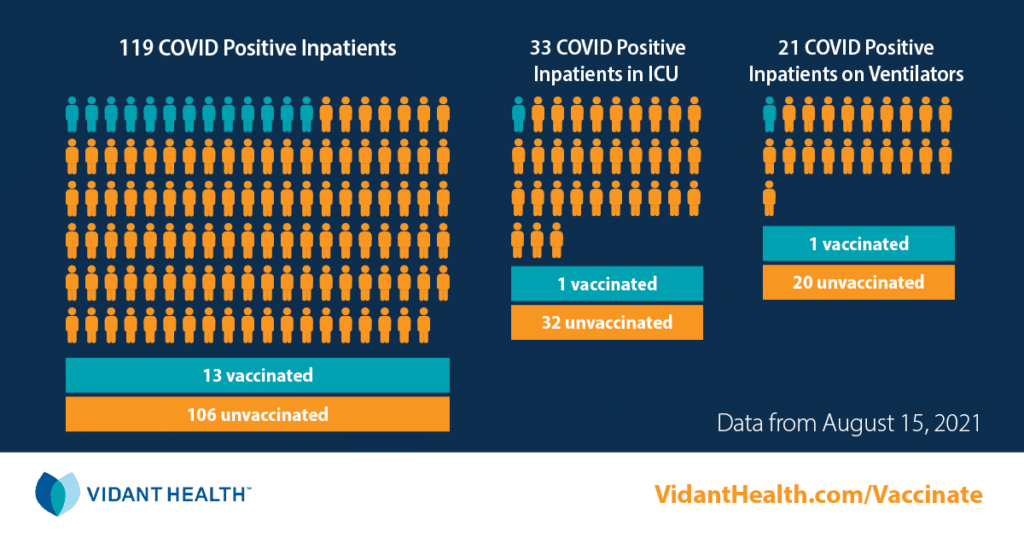
On Aug. 16, 91 percent of those hospitalized in a Vidant hospital were not vaccinated. Of those in the Vidant system on Aug. 15, 36 COVID-positive patients were in the ICU with 22 on ventilators. Only one of those patients was fully vaccinated. Vidant has had no patients hospitalized due to reactions from the vaccine. The vaccine is available to everyone age 12 and older and appointments can be found at VidantHealth.com/Vaccinate.
According to the North Carolina Department of Health and Human Safety, as of Aug. 20, 64 percent of North Carolinians 18 or older have received at least one dose of a COVID-19 vaccine and 59 percent are fully vaccinated. For eastern North Carolina, those numbers drop to 56 percent with at least one dose and 51 percent fully vaccinated.
Get vaccinated today
Chief of Adult Medical Services at ECU Health Medical Center (VMC) Dr. Paul Bolin said the demographics of those coming to the hospital with COVID-19 are skewing younger than at any other time during the pandemic. Bolin, who also serves as the chair of the department of medicine at Brody School of Medicine, compared getting the vaccine to wearing a seatbelt in a car and said your chances of surviving COVID with the vaccine are 25 fold better than without.
“I think the most important thing to understand is this,” Dr. Bolin said. “There have been a very small number of complications from the vaccine. That is a one-time event that occurs after the vaccination. Your risk of dying from COVID if you’re not vaccinated continues day after day after day after day until this pandemic is over.”
VMC President and Vidant COO Brian Floyd hosted a press conference recently to discuss the importance of receiving the COVID-19 vaccine, especially as we experience another surge in cases and hospitalizations.
“Take care of your loved ones, take care of your community and help us take care of this team that’s been here for the public for the last year and a half looking out for their interests,” Floyd said. “It’s a personal choice we make on a mask or vaccine or whatever, but it is a public impact. You are making that choice on behalf of more than you – you’re making it on behalf of people.”
Floyd reiterated messages that have been important to slowing the spread of COVID-19 since the very beginning of community spread:
- Wear a mask when in public
- Get tested for COVID-19
- Get your COVID-19 vaccine
Learn more about Vidant’s COVID-19 efforts in recent interviews with Public Radio East and WNCT.
Vidant Health’s mission to improve the health and well-being of eastern North Carolina stretches beyond the walls of our hospitals and clinics here in the East.
With recent Community Health events across the 29 counties we serve, Vidant is delivering health care in unique ways. Recently, Vidant partnered with local leaders and community groups to host these events in Grantsboro in Pamlico County and Farmville in Pitt County.
Community members had the opportunity to get health screenings, receive health coaching, learn about providers and health care options near them, and even receive a COVID-19 vaccine.

Cheryl Willoughby, project coordinator for Systems & Procedures at Vidant, plays a key role in organizing these events. She said it is crucial to bring health care to the people of eastern North Carolina because of Vidant’s unique rural positioning.
“Access to health care is a huge issue for a lot of the people that we serve,” Willoughby said. “So when we do these community events, that barrier is easily broken when we meet people where they are. That’s the exciting piece for me.”
Pamlico County Health Event
 Vidant hosted a Pamlico County Community Health event on July 27 at Pamlico County Community College with great support from many local leaders and organizations. Pamlico County government, the Pamlico County Health Department and Pamlico County Community College all played a vital role in making the event possible.
Vidant hosted a Pamlico County Community Health event on July 27 at Pamlico County Community College with great support from many local leaders and organizations. Pamlico County government, the Pamlico County Health Department and Pamlico County Community College all played a vital role in making the event possible.
Vidant Beaufort Hospital, a campus of Vidant Medical Center, team members came out to the event to administer health screenings to community members, including body mass index measurements, blood pressure readings and blood sugar checks. Team members were also on hand to educate the community on colorectal cancer, diabetes and stroke.
Jennifer Lewis, community health improvement coordinator for Vidant Beaufort, said screenings and wellness checks events like these are crucial to making sure community members are staying on top of their health. She said that people will often go through everyday life feeling completely healthy while chronic illnesses like hypertension and diabetes go unchecked.
“We want to help identify some of those risk factors and maybe here we can share something with an individual that will get their attention,” Lewis said. “Hopefully we can get them in to see a physician and maybe make some changes in their diet, in their physical activity and if they need to get medication, that too.”
Dr. John Callahan from Vidant Family Medicine – Aurora was on hand to discuss any concerns with community members and to discuss COVID-19 vaccines with those interested. About 20 COVID-19 first doses were distributed to community members at the event.
The EastCare team also showed support for the Pamlico County event by showcasing a helicopter on the main road leading to the event and the Eastern Carolina Health Care Preparedness Coalition had a medical emergency bus and mobile field hospital out on display for the event as well.
Farmville Community Health Event
 The following weekend, Vidant team members and community groups showed up again to bring health care directly to the communities we serve at the Farmville Public Library. Many of the same screenings and opportunities available at the Pamlico County event were brought to Farmville as well.
The following weekend, Vidant team members and community groups showed up again to bring health care directly to the communities we serve at the Farmville Public Library. Many of the same screenings and opportunities available at the Pamlico County event were brought to Farmville as well.
KaSheta Jackson, nurse executive fellow at Vidant, said the community partnerships Vidant has built and are working to strengthen are key to creating trust with the whole community. She said having those trusting relationships with community groups trickles down to individuals within communities and ultimately leads to better health for everyone.
“We are making sure that we are connecting with the community,” Jackson said. “We are here with CAREE, which is a community group. They’re doing our vaccines with the Pitt County Health Department. The local library, they’ve offered up the space. Cheryl (Willoughby) worked with a lot of local agencies here so that they would support it. We work with a lot of communities here because we don’t want to just come in, we want to be a part of how we improve health care in these comminutes.”
Along with health screenings and awareness campaigns at the event, behavioral health team members were on hand to provide support and share information. Vidant’s Talent Acquisition team also joined each of the events to make connections with community members seeking employment with the health system.
Jackson said the Community Health events are important to bringing health care to people and hopes that positive responses and results continue to come out of these opportunities.
“We are following the model of doing health care on the outside to make health care better on the inside,” Jackson said. “We’re working to address the social determinants of health, offering employment, trying to take care of the need for vaccines, taking health care into communities versus having people come to us – we’re taking services to those that need them.”
Where will we be next?
Vidant’s next Community Health event will be on Aug. 21 in Bethel at the Field of Dreams – additional information can be found on the Events page of VidantHealth.com.
With easing COVID-19 restrictions, we are on the move again, especially children and teens in sports. With that comes the potential for injury and Vidant Orthopedics and Sports Medicine is here to help.
Vidant Orthopedic surgeon Dr. Robert Palmer appeared on WITN to discuss common sports injuries and how to prevent them.

He said the most common sports-related injuries he sees are broken wrists and clavicle fractures. The most important things you can do for yourself or your child to prevent sports injuries is to maintain a typical healthy lifestyle and get plenty of Vitamin D.
Dr. Palmer said a unique risk this year is young people returning to sports after a year away.
“I’ve seen quite a number of children in my clinic who have gone back, and just participating in a field day event at school and they’ve actually gotten stress-related fractures from what we would consider everyday events,” Dr. Palmer said. “That is probably just because their bodies aren’t used to the load from sports. I think taking it slow and easing back into things and making sure they have a good healthy diet is a good start to prevent injuries.”
He also discussed the importance of the implementation of rules to limit overuse injuries. An example of this is rules set by youth baseball organizations in conjunction with Major League Baseball to keep children safe. Dr. Palmer encouraged coaches and parents to educate themselves on these rules and stay on top of them to keep children healthy.
While many sports-related injuries in children just require typical treatment like rest and ice, some are more serious. It can be challenging to know when it’s time to consult a physician but Dr. Palmer gave some tips on what to look for.
“When we see a patient, if they have limited range of motion, inability to weight bear, swelling about a joint, reduced motion about that joint,” Dr. Palmer said, “certainly if there’s a bone sticking out of the skin or there’s bleeding, those are more urgent things that we should address and potentially may need surgery. Other sports-related injuries are ACL tears or ligament tears and shoulder instability that we think about.”
Visit the Orthopedics and Sports Medicine section of VidantHealth.com to learn more about services Vidant offers.
Greenville, NC – Aug. 12, 2021 – As Vidant Health continues to respond to the evolving COVID-19 pandemic across North Carolina, we are taking steps to ensure the safety of all. Vidant remains vigilant with its screening process for all visitors, entry requirements and visitor restrictions by department.

In response to increased community spread and the heightened risk of hospitalization posed by the Delta variant, all Vidant Health hospitals are adjusting visitation policy in the Emergency Department. To ensure the safety of patients, families and team members, effective 7 a.m. Friday, Aug. 13, visitors will not be allowed in the ED lobby or waiting areas at hospitals across Vidant’s system. ED patients can have one healthy adult visitor screened and masked at all times once the patient has been placed into a room, as long as the patient is not COVID positive.
It remains vitally important that community members continue to practice safety measures such as washing hands, wearing a mask and avoiding large gatherings.
Learn more about visitation at VidantHealth.com/VisitingVidant.
Greenville, NC – Aug. 11, 2021 – As Vidant Health continues to respond to the evolving COVID-19 pandemic across North Carolina, we are taking steps to ensure the safety of all. Vidant remains vigilant with its screening process for all visitors, entry requirements and visitor restrictions by department.

In response to increased community spread and the heightened risk of hospitalization posed by the Delta variant, ECU Health Medical Center is adjusting its visitation policy in the Emergency Department. To ensure the safety of patients, families and team members, effective 7 a.m. Thursday, Aug. 12, visitors will not be allowed in the ED lobby or waiting areas. ED patients can have one healthy adult visitor screened and masked at all times once the patient has been placed into a room, as long as the patient is not COVID positive.
It remains vitally important that community members continue to practice safety measures such as washing hands, wearing a mask and avoiding large gatherings.
See the full list of visitation restrictions at ECU Health Medical Center here and learn more at VidantHealth.com/VisitingVidant
These topics included psychiatric disorders, stress management, resiliency and substance use. This series came at a crucial time, as COVID-19 kept many people indoors and away from their typical routines. That isolation and facing many unknowns in our world brought out mental health challenges.
Data trends show a steady increase in adults suffering from anxiety, stress, and depression over the past year.
Glenn Simpson, system service line administrator for Behavioral Health at Vidant, joined WITN to discuss the series.
“Some studies are indicating that four out of 10 of us in the last year have experienced depression or anxiety in a clinical range,” Simpson said. “If you went back two years, that would have been one out of 10, so we are very concerned about people’s mental health. Often times we will take care of our physical health before our mental health. We’re hoping by this series to help folks reach out for the help they need.”
Simpson said the series was exciting and brought forward experts in the field to talk to the general public about mental health and well-being.
Video recordings from the series can be found in the Behavioral Health section of VidantHealth.com.
Anxiety in adults exasperated over the pandemic
A new study from GlobalWebIndex has shown that many adults are worried about the lasting effects the pandemic will have on mental health.
According to the study, 28% of Millennials, and 29% of Gen X adults believe the pandemic will have long-term impacts on their mental health. Additionally, the study found that anxiety, stress and insomnia had all risen across all age groups in the study.
Dr. Nathan Harper, medical director for inpatient psychiatry at ECU Health Medical Center and ECU, said he there has been an increase in patients for mental health needs and services, not only in adults but for children as well. Dr. Harper said he believes isolation from quarantine made some of these issues more prevalent.
Dr. Harper discussed the study and his experience during a recent interview with WNCT.
Vidant has resources and information available on the Programs & Support page.
COVID-19 continues to evolve and expand its grip across the country and here in eastern North Carolina.
“This is one of the most diabolical viruses I’ve ever seen,” said Dr. Paul Bolin, chief of Adult Medical Services at ECU Health Medical Center, and the chair of the Department of Medicine at Brody School of Medicine at East Carolina University.
“We were in a good place. Transmission had slowed down, more and more people were getting vaccinated and protected, hospitalization days started to really come down, number of cases started to come down – and many of us thought we were in the last leg of this marathon,” said Dr. Niti Armistead, chief medical officer for Vidant Health. “What changed was the vaccination rates just hit a wall.”
“In North Carolina, in the past three to four weeks, we have seen a tripling in the number of cases, and in the number of hospitalizations,” said Dr. Bolin. “We’re seeing the same things as we did last fall and winter, but it’s in a much younger and much healthier population.”
Another difference now – we have a vaccine.
“It’s like wearing your seatbelt – your chances of being in an automobile accident are very low, but your chances of surviving that with a seatbelt are much greater,” said Dr. Bolin. “Your chance of surviving COVID are 25 fold better with the vaccine than without it.”
Even still – roughly half of the country remains unvaccinated, enabling the virus to mutate and variants to cause an increase in infections and complications.
“The virus didn’t slow down just because our vaccination rates dropped,” said Dr. Armistead.
Experts say most concerns about the vaccine don’t outweigh the risk of being unprotected.
“I think the most important thing to understand is this: there have been some very small number of complications from the vaccine. And that is a one-time event that occurs after the vaccination,” said Dr. Bolin. “Your risk of dying from COVID if you’re not vaccinated continues day after day after day after day, until this pandemic is over with.”
Vidant Health has appointments available for anyone eligible to receive the vaccine. Visit www.VidantHealth.com/vaccinate and schedule yours today.
 The arrival of the COVID-19 vaccines brought great hope in the battle against the deadly pandemic that has affected our way of life for nearly a year and a half. Now, more than 7 months into the largest vaccination effort in history, the data and science is clear: the vaccines are effective, but only if people get their “dose of hope”.
The arrival of the COVID-19 vaccines brought great hope in the battle against the deadly pandemic that has affected our way of life for nearly a year and a half. Now, more than 7 months into the largest vaccination effort in history, the data and science is clear: the vaccines are effective, but only if people get their “dose of hope”.
The continued spread of the virus and the arrival of new variants is an urgent reminder that this pandemic is not over yet, and that we still have to assure vaccination for everyone to protect our communities. Right now, the Delta variant is quickly becoming the dominant virus variant. We know that this variant is easily spread and has many of the same devastating health impacts as previous variants. We also know that the vaccines are highly effective at both preventing the spread of the virus and drastically reducing the impact on those it infects.
It was not long ago that some hospitals around the country celebrated having zero COVID-19 patients in their Intensive Care Units. Doctors, nurses and other staff rejoiced at this welcomed respite. Here at Vidant, we never quite got to zero, but our numbers hit a new low in the spring. Now, hospitalizations are back on the rise and nearly all hospitalized COVID-19 patients – many of whom are battling for their lives – are unvaccinated.
As we have continued to learn more and more about this virus over the past year and a half, we can confidently say that ending up hospitalized with serious complications from COVID-19 is mostly avoidable now. The vaccines are safe, effective and widely available at local hospitals, clinics, health departments, pharmacies and more.
We can still see the light at the end of the tunnel but the Delta variant is dimming our view. Help us end this pandemic by receiving your COVID-19 vaccine as soon as possible by visiting VidantHealth.com/Vaccinate or by calling 252-847-8000.