Greenville, N.C. – East Carolina University’s College of Nursing and ECU Health are launching an Adult Gerontology Acute Care Nurse Practitioner program, a new graduate-level certificate program that will prepare more specialized nurse practitioners in acute care settings across the state.
“We have a lot of nurse practitioners in North Carolina who are doing amazing work to care for patients in ICUs and other very demanding care sites, we also want to expand the knowledge, skills and abilities of current practitioners because the need is so high and the shortage of providers is so great,” said Dr. Julie Linder, chair of the Advanced Nursing Practice and Education department. “This new program will provide the didactic and clinical experiences necessary to meet the needs of our patient populations.”
According to the American Association of Nurse Practitioners, only 6.1% of nurse practitioners specialize in adult gerontology acute care.

The aging population is growing nationally, along with an ongoing shortage of health care workers. The collaboration between the College of Nursing and ECU Health bolsters the health care workforce in eastern North Carolina, enhances health outcomes and increases access to specialized care for older adults in these communities.
“ECU Health values its strong partnership with ECU and the College of Nursing, especially in addressing the national health care workforce shortage,” said Pam Rudisill, vice president of nursing excellence at ECU Health. “Our success as an academic health system relies on bridging clinical and academic excellence to provide high-quality care to eastern North Carolina. Eastern North Carolina depends on collaborative solutions from institutions like ECU Health and ECU to meet the needs and improve the health and well-being of our region.”
ECU Health’s Chief Nursing Office will support their employees by offering tuition reimbursement as a commitment to support the certificate program and help employees advance their education and skills.
The first cohort of ECU’s Adult Gerontology Acute Care Nurse Practitioner certificate program will begin classes in Spring 2025. Students who complete course requirements on the recommended plan of study should graduate in May 2026. Upon graduation, these students will be eligible to take a specialty exam to become certified as Adult Gerontology Acute Care Nurse Practitioners.
The application deadline for that first cohort is Dec. 15, 2024, and applicants can find application requirements and procedures, along with required courses in the curriculum, here.
The certificate program is a post-master’s program, which means applicants must already be recognized as an advance practice nurse. The education students will receive will provide them with the skills to work in acute care settings. ECU offers pre-requisite courses if prospective students have not already completed them.
“We invite prospective students to contact us in the event they need pre-requisite courses prior to beginning their core class work,” Linder said.
ECU’s College of Nursing and ECU Health previously developed pathways for the development of the future of nursing care in eastern North Carolina with the establishment of an academic-practice partnership, seeded by a $1.5 million investment from ECU Health over five years. This investment has provided the ECU College of Nursing with the opportunity to hire faculty, staff, and purchase resources to support students in the Adult Gerontology Acute Care Nurse Practitioner certificate program.
The first cohort will comprise approximately 12 students, with a minimum of six seats dedicated to ECU Health employees and other slots open to applicants interested in advancing their career in critical care.
ECU will join three other nursing programs in North Carolina to offer the AGACNP certification.
Greenville, N.C. – After six years with ECU Health, including serving as president of ECU Health North Hospital since August 2020, Jason Harrell has announced his retirement effective Aug. 8, 2024. ECU Health has begun a national search for the next president of ECU Health North Hospital. Dennis Campbell II, DHA, RN, NEA-BC, will serve as interim president of ECU Health North Hospital in addition to his current role as president of ECU Health Beaufort Hospital.

Jason Harrell
“On behalf of ECU Health, I would like to thank Jason for his service and dedication to advancing our mission over the years,” said Van Smith, president, ECU Health Community Hospitals. “Jason has had a distinguished 40-year career in health care, and we are grateful for his service to ECU Health. During his time at ECU Health North, Jason’s leadership, collaboration and focus on the priorities of access, quality, experience and safety have been unwavering. ECU Health North Hospital team members, patients and the community have benefitted from Jason’s leadership accomplishments.”
Campbell, II will serve at ECU Health North on an interim basis until the national search is completed. He has been with the health system for four years, previously serving as ECU Health Beaufort’s vice president of Patient Care Services before taking on the role of president in September 2023.

Dennis Campbell II
During his time at ECU Health Beaufort, Campbell, II has prioritized developing relationships with important stakeholders and partners in the area including Beaufort Community College and ECU, exemplifying his dedication to investing in the future of academic health care in eastern North Carolina.
“Dennis’s leadership skills and deep understating of the needs of our team members and the communities we serve in eastern North Carolina will be invaluable assets to ensure the stability and ongoing success of ECU Health North Hospital during this time of transition,” Smith said. “I appreciate Dennis’s willingness to serve the system in this capacity.”
As an academic health system, ECU Health serves as both a rural care delivery organization and a training ground for health care providers and support services team members.
While resident physicians and nurses come to mind as the most obvious roles that blend the clinical and academic environments, a new resident track is helping bridge an important need for patients across eastern North Carolina who are Deaf or Hard of Hearing: the ECU Health American Sign Language (ASL) Residency program.
Launched in April, the ASL Interpreter Residency program was born from the demand for more skilled ASL medical interpreters. The program is designed to help increase the number of ASL interpreters available to patients across ECU Health’s system, in both hospitals and clinics, as well as train the next generation of interpreters for a career in the medical field.
More than 500,000 people throughout the United States use ASL to communicate as their native language, making ASL the third most common language in the United States, after English and Spanish, according to the Commission on the Deaf and Hard of Hearing.

“There is a massive need for ASL interpreters in health care both nationally and locally,” said ECU Health ASL coordinator Reid Barnes, who designed the program. “When we looked at this need in the lens of our role as an academic health system, it made sense to model something similar to the physician resident experience.”
Residents in the program join with a two-year commitment where they focus on skill development and clinical interpreting during their first year, with close supervision in the clinical setting. The second year of the program incorporates both hospital and clinical work while also assisting with ongoing educational efforts.
Barnes, ECU Health’s only full-time ASL interpreter, works with up to 6 or 7 patients on any given day, often times spread across the health system’s 29 county service area, so the demand is obvious. What is less obvious, however, is the process behind becoming a skilled medical ASL interpreter.
A licensed or certified ASL interpreter does not receive a specialized certificate in medicine. ASL interpreters undergo rigorous testing to ensure they have generalized competencies for a multitude of interpreting settings. However, the decision to specialize in any setting is left to the individual interpreter. Specialization often involves an extensive combination of targeted workshops and firsthand experience. As a result, it is often difficult for newer interpreters to safely gain firsthand experience.
All of these factors, Barnes said, inspired the creation of the ECU Health ASL Interpreter Residency program.
“Health care should always be provided in a patient’s native language,” said Barnes. “Imagine what your health care experience would feel like if you couldn’t communicate with your doctors and nurses in your primary language? For the Deaf and Hard of Hearing community, that is a very real reality. We can now expand our services, improve patient experiences and be a true training ground for skilled medical ASL interpreters.”
Jordan Satchell is the first ever resident in the ECU Health ASL Interpreter Residency program. Having served as an experience coordinator in ECU Health Medical Center’s emergency department, she has a close understanding of the important role ECU Health serves as the flagship health system in eastern North Carolina.
“Returning to ECU Health as the first ASL Interpreter Resident has been a rewarding experience in many different ways,” said Satchell. “You never truly ‘arrive’ when it comes to interpreting, so this program has allowed me to build my skills and improve my knowledge about health care. The patients I work with have already helped me become a better interpreter, and I can only hope to continue serving them, learning their needs, breaking down communication barriers, while also being a resource to the next incoming resident.”
Barnes said Satchell will help chart the future of the program, as the two work together to closely examine the needs of the patient population while tailoring the program’s design to ensure it provides the best resident experience possible.

OUTER BANKS, N.C., July 24, 2024 — Outer Banks Health and Dare County Department of Health & Human Services have joined forces with Blue Zones, the global leader in longevity research and community well-being transformation, to launch Blue Zones Ignite™ Outer Banks.
Blue Zones uses an evidence-based, environmental approach to making healthy choices easier where they live and spend most of their time. Blue Zones will work with Outer Banks Health, the County, and other community leaders to conduct an in-depth feasibility assessment to determine how to make it a healthier place to live, work, and thrive. Together with the community, the Blue Zones team will assess readiness and build a plan for change.
The launch of Blue Zones Ignite is a dream come true for Christina Bowen, MD, Outer Banks Health Center for Healthy Living Medical Director, and ECU Health Chief Well-being Officer.

“We know that 20% of health and longevity is tied to genetics; while 80% is tied to where and how we live. Blue Zones Ignite Outer Banks is going to inspire us to celebrate and promote our strong sense of community while we find ways to make it even easier to eat healthy foods, move naturally and connect with our purpose – just a few of the ways we’ll continue to enhance our well-being and make this an even better place to live and work,” shared Dr. Bowen.
The Blue Zones Approach
Blue Zones employs a proven solution in collaboration with communities to help people live better and longer lives. The company’s work is based on research and principles developed by National Geographic Fellow and New York Times bestselling author Dan Buettner, who identified the cultures of the world – or blue zones regions – with the healthiest, longest-living populations.
The Blue Zones approach focuses on the single largest determinant of health: the place we live. Instead of focusing solely on individual behavior change, Blue Zones helps communities make permanent and semi-permanent changes to policies, systems, streets, surroundings, and social networks so it’s easier for residents to eat wisely, move naturally, and connect more with others as they move throughout their day. By improving the Life Radius®—the area close to home where most Americans spend 90% of their lives—Blue Zones transformations have been able to move the needle dramatically in improving overall population health and well-being. Communities that have participated in the Blue Zone’s Ignite project have seen double-digit drops in obesity and smoking rates, economic investment in downtown corridors, grant funding awards to support policies and programs to improve health equity, and measurable savings in healthcare costs.
“Together, Outer Banks Health and Dare County Health and Human Services are steadfast in our shared mission to enhance the health and well-being of all residents, so that they can live a happy, healthy and long life,” said Dr. Sheila Davies, Director Health & Human Services.
Ben Leedle, CEO of Blue Zones and Co-founder of Blue Zones Project, said: “We are excited to partner with forward-thinking leaders in the joint effort of improving well-being in the Outer Banks. That improvement, at the community level, leads to healthier and happier residents, better and more productive workforces and student bodies, and a more vibrant economy. We are excited to collaborate to create a transformation plan that can generate lasting positive change and ignite a community-wide movement towards sustained well-being.”
The Blue Zones expert team will connect with Outer Banks leaders and organizations to begin immediate work assessing the strengths, needs, and challenges that residents are facing today. Blue Zones will then create a policy-focused transformation plan that, once implemented, can drive widespread improvements in well-being, reductions in healthcare costs, and improve economic vitality in the region.
Greenville, NC — Andy Zukowski, ECU Health chief financial officer, was recently honored by Becker’s Hospital Review as one of 36 Rural Hospital CFOs to Know. Zukowski has served as CFO since 2022 and oversees the financial operations at both ECU Health and the Brody School of Medicine at East Carolina University.

Andy Zukowski, ECU Health chief financial officer
“It’s an honor to be nationally recognized for the work we do here at ECU Health,” said Zukowski. “Our goal at ECU Health is to build the national model for high-quality rural academic health care and being good stewards with our resources is a key component of that. I am proud to work alongside mission-driven individuals who commit their time, expertise and energy to serving the people of rural eastern North Carolina.”
Rural hospitals are an essential component of today’s health care environment, dedicated to serving populations that often encounter obstacles to convenient, quality and affordable care. These institutions play a critical role in ensuring healthcare access for underserved communities. The CFOs highlighted on the list are instrumental in ensuring the financial health of their organizations. Applying their expertise in financial planning, these executives help bring cost effective, innovative, up-to-date and accessible healthcare to their communities.
“Andy’s passion for serving others and mission-focused mindset align with ECU Health’s mission to improve the health and well-being of eastern North Carolina,” said Dr. Michael Waldrum, CEO of ECU Health and Dean of the Brody School of Medicine. “As the largest health care provider, employer and medical educator in the region, ECU Health has a unique role to play in the communities we serve – and Andy recognizes that this depends on the organization’s sustainability. ECU Health is proud to help lead the way in creating jobs and encouraging economic growth to help improve the rural communities we serve, many of which experience socioeconomic distress and health disparities.”
Becker’s is delighted to feature these accomplished leaders, who are critical to the successes of their respective organizations. The Becker’s Hospital Review editorial team accepted nominations for this list and curated it to highlight the fantastic accomplishments of rural hospital CFOs.
When it comes to skin cancer, it is no secret that early detection can save lives. Increased exposure in the sun’s ultraviolet rays greatly increases the risk for skin cancer, especially among those who work outdoors. That is why Eve Stroud, community health improvement coordinator at ECU Health Duplin Hospital, has been spending her summer in hardware stores around Duplin County providing cancer awareness information and free health screenings as part of the Hardware Store Tour.
Designed to help bring resources to people who may be at elevated risk for skin cancer – particularly those who work outside – the Hardware Store Tour initiative was first launched in 2023. Stroud and her team pair skin cancer education with free wellness screenings for important things like body mass index, blood pressure and glucose/cholesterol checks. In its first year alone, the team completed 37 health screenings and provided skin cancer education to 115 people in just three hardware store visits.
“It is always rewarding to spend time in the community providing helpful health resources to those we serve,” Stroud said. “When it comes to caring for your own health and well-being, information and education can make all the difference. Through initiatives like the Hardware Store Tour, we’re hoping to help people understand their risk factors so they can better manage their health.”
Now in its second year, Stroud and her team are continuing to focus on meeting people where they are in the local community by providing these important resources. The Hardware Store Tour is just one of the many ways ECU Health team members work toward the mission of improving the health and well-being of eastern North Carolina.

On June 14, 2024, Dr. Brian Brodish, an otolaryngologist with Eastern Carolina ENT, in collaboration with ECU Health, performed his 100th Inspire procedure at ECU Health Medical Center. Inspire is an FDA-approved obstructive sleep apnea (OSA) treatment option for people who cannot use Continuous Positive Airway Pressure (CPAP) therapy.
“We have a high incidence of sleep apnea in eastern North Carolina, but a lot of patients can’t tolerate a CPAP,” said Dr. Brodish. “There’s a significant morbidity to not treating sleep apnea, and up until now, I had nothing to offer. This is one of the first successful surgical alternatives for our patients with sleep apnea.”
OSA affects 22 million Americans. When left untreated, it doesn’t just affect one person, but also those around them. OSA can cause vehicle and workplace accidents, worsening mood and memory, stroke, heart attack and other serious issues.
CPAP is the main treatment for OSA, but unfortunately a large percentage of people don’t see benefit from or can’t tolerate CPAP. Dr. Brodish is proud to offer Inspire as another treatment option for this population.
“Patients were feeling miserable and had nowhere to turn,” Dr. Brodish said. “I finally have a tool I can offer these patients and we’re seeing fantastic results. It’s a low-risk procedure and patients recover in a few weeks.”

Inspire works inside the body with a patient’s natural breathing process to treat sleep apnea. Mild stimulation opens the airway during sleep, allowing oxygen to flow naturally. The patient uses a small handheld remote to turn Inspire on before bed and off when they wake up.
“We want the patient to use the device for at least four hours a night or more, and we are looking for their apnea-hypopnea index (AHI), which is the number of times per hour a patient stops breathing, to be below 15,” Dr. Brodish explained. “Some of our patients stop breathing more than 50 times a night before treatment, but 80 percent of our patients have achieved our goal of 15 episodes or less. Some have even achieved zero.”
The Inspire system is implanted during a short, outpatient procedure. The system is placed under the skin of the neck and chest through two small incisions. Most patients return home the same day and take over-the-counter pain medications to manage pain as needed.
“We are excited to have completed the 100th Inspire procedure at ECU Health Medical Center,” said Dr. Brodish. “This option is a part of ECU Health’s goal to provide state-of-the-art, high-quality care for eastern North Carolina, and we’re seeing patients benefit from this technology.”
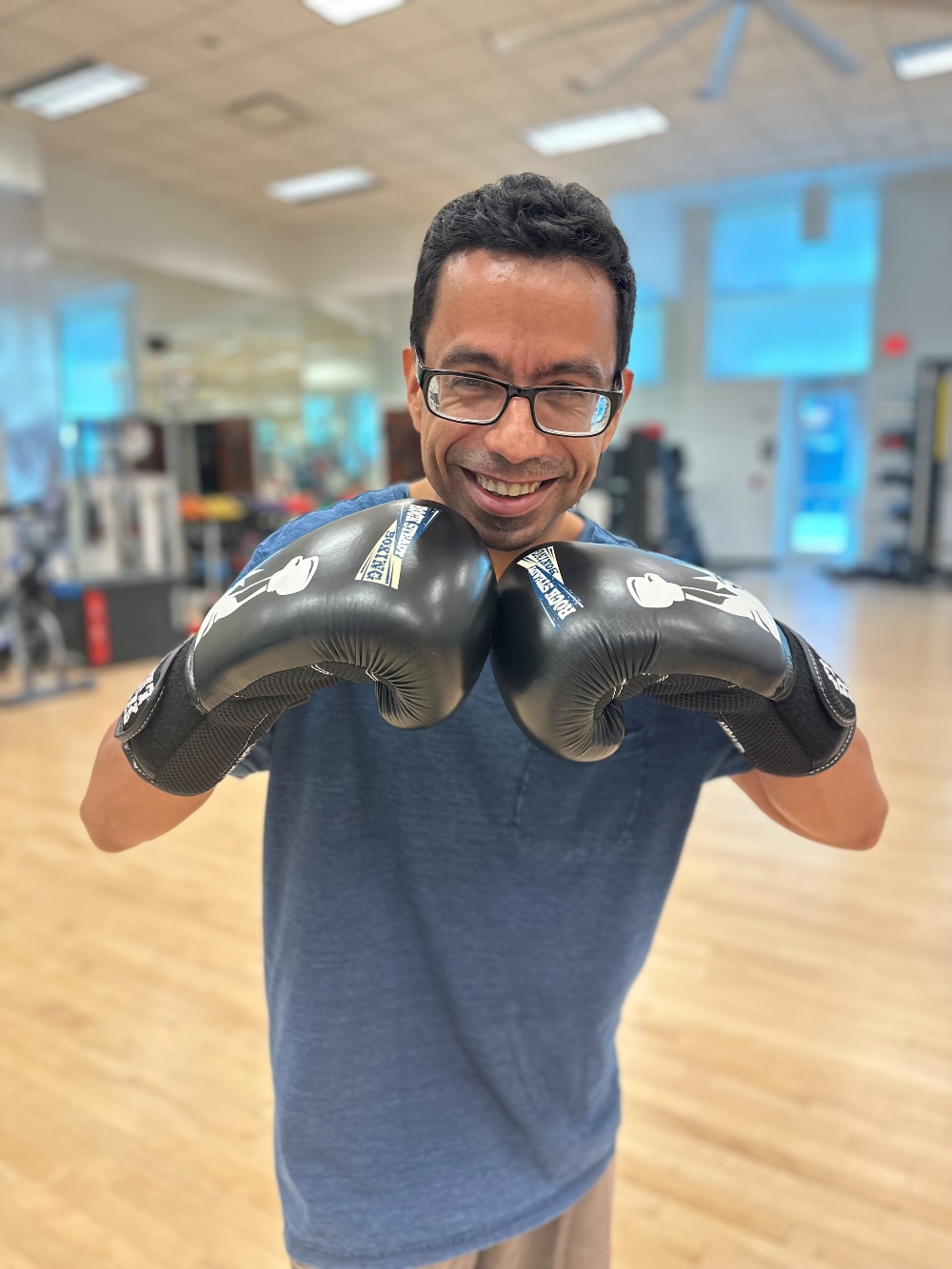
Chris Smith, the vice president of finance and operations for the ECU Health Foundation, was working out at the ECU Health Wellness Center when the director pulled him aside and told him about the Rock Steady Boxing program – a non-contact, boxing-inspired fitness routine specifically created for patients with Parkinson’s disease and similar movement disorders.
“They were looking for help with starting up the program – equipment, training for a few coaches, that sort of thing,” Smith said. “I told him we’d take a look at how the Foundation could help, and as it turned out, we were able to provide them the funds they needed to get the program started.”
Parkinson’s disease is a neurological disorder that causes unintended or uncontrollable movements, such as shaking, stiffness and difficulty with balance and coordination. Symptoms worsen over time, causing difficulty with walking, talking or other daily activities. While there is no cure, physical activity can improve many symptoms of Parkinson’s disease, slow the progression of the disease process and improve patients’ quality of life.

First created in Indianapolis in 2006, Rock Steady Boxing is now an international nonprofit program with more than 840 certified affiliates. Now, ECU Health’s Wellness Center counts itself among those numbers because of the Foundation’s support.
Smith said it was gratifying to know that money given by donors was used in such a meaningful way.
“This demonstrates the impact of what our donors do for their friends and families in the region. It showed the tangible impact philanthropy has on the lives of people in eastern North Carolina.” Smith also had a personal connection to the program; his father had Parkinson’s. “He passed away right before the pandemic. He was doing rehab, but he could never get back on his feet.”
With those donor-provided funds, which covered the cost of coach training in Indianapolis and the necessary equipment, the ECU Health Wellness Center was able to establish a Rock Steady Boxing program in 2023. Two of the coaches trained for the program were Kiara Robins, the lead exercise specialist, and Cas Costa, an exercise physiologist II. More than 36,000 people live with Parkinson’s disease in North and South Carolina, and Costa highlighted the value of having this program in the area.
“I didn’t realize at first the impact it would have, and I didn’t know how few locations offered the class.” That’s true; the ECU Health Wellness Center is currently only one of three locations to offer the program in eastern North Carolina. As a result, Robins said that their class has grown quickly: “We started with just three or four members but now we’re up to ten or twelve. We have people come from Rocky Mount, Kinston, Grimesland, Snow Hill and Ayden looking to do the program. We’re steadily growing, and we’re seeing great results.”
Those results are measured through balance and gait tests, such as the Berg Balance test and the Get up and Go test. “Our first four participants have gone from high fall risks to medium or low risks,” Robins said. “Some couldn’t even complete components of the tests, but they now can.”
Justin Mendoza, one of the participants in the class and its youngest member, attested to the program’s positive effects. “They [the coaches] really put their heart into thinking of exercises. You have someone who has studied this and knows what you’re going through. I’ve improved in my strength and walking, and I don’t fall as often,” he said.
While some clients, like Mendoza, heard about the Greenville class when theirs shut down, others received referrals from their physical therapists or physicians. Dr. Temitope Lawal, an ECU Health movement disorder neurologist, is one of those doctors to refer patients to the program.
“Exercise slows the progression of Parkinson’s,” he said. “It’s an extrapolation of the saying, ‘if you don’t use it, you lose it.’ This program makes you accountable and asks you to move your muscles as much as you can.” Dr. Lawal also noted the social value of the program. “It’s an avenue for interaction with others who have Parkinson’s, so it’s like an informal support group.” Costa agreed: “The biggest benefit is the sense of community. It’s hard to go to a regular gym and know what to do. But here, everyone has Parkinson’s so there’s a level of comfort with the activities.”
That accessibility to specialized exercise programs is just one of the things that sets apart the ECU Health Wellness Center.
“The Wellness Center is more than a gym,” Robins said. “You have trained staff here, all with a degree in exercise and certified in one or more areas to better serve the population.” Costa also emphasized the value of specialty-trained staff. “We’re a wellness center, which is different from a gym. In a gym you can’t see a dietician or a lifestyle coach or go next door for a physical therapy appointment. We have a full-circle of wellness with staff trained to help patients with Parkinson’s, arthritis, orthopedic needs, cancer and other diagnoses.”
Both coaches acknowledged that collaboration is required to make Rock Steady Boxing and other programs successful.
“I’m working towards a Ph.D. in kinesiology, and in school we’re learning about the relationship between physicians and exercise physiologists,” said Costa. “Rock Steady Boxing is an example of that collaboration. ECU Health supporting this program helps us build relationships with the doctors and specialists in the network.”
This partnership provides access to valuable resources and complements the medications patients with Parkinson’s must take to combat the symptoms.
Membership is not required to participate in Rock Steady Boxing. “90 percent of our participants are non-members,” Robins said. Participants pay for eight sessions per month, but there’s also a drop-in rate for those who have less predictable schedules. Those who are unsure if they want to join can observe a class for free, and they can participate in the class on a month-to-month basis with no obligation.
Robins said the program has plans to continue its growth so it can better serve the region, and both she and Costa shared their appreciation to the Foundation for supporting the program.
“We’re grateful to have this program here in Greenville,” Robins said. “We’re still in the beginning stages, but we want to expand as much as we can and get more members. We want to encourage everyone with Parkinson’s to participate and to let them know we’re here to help as much as we can.” Mendoza championed the program and the coaches for their hard work: “I love the class. We have fun, and the coaches know what they’re doing. You don’t feel intimidated or self-conscious, and it gives you a sense of pride.”
Cheryl Hooks, a family nurse practitioner (FNP), is a Rose Hill native who started her career cutting hair. “For a very long time, about 20 years, I worked as a cosmetologist and I owned my own beauty salon,” Cheryl said.
Things changed for her and her close-knit family when they learned her oldest niece, nine years old at the time, had juvenile, or Type 1, diabetes.
“She got sick and had to go to the hospital, and that’s how they found out she was diabetic,” Cheryl said. “It was very scary because no one really knew what to do or how to help her.”
Cheryl wanted to learn all she could about the illness, including about medications and diet, so she could better support her niece; but in the process, she realized she wanted to advocate for all individuals with health problems. That’s when she decided to become a nurse.
Making the shift to nursing wasn’t easy. “I was older and trying to manage my time. You go from a point where you are your own boss to not having that freedom because you’re in school,” she said.
Still, her desire to take care of people inspired her to keep going. After graduating with her RN from Wake Technical Community College in Raleigh, Hooks worked at ECU Health Duplin Hospital while pursuing her BSN from the University of North Carolina (UNC) at Wilmington. She started her health care career in behavioral health, and later worked in the emergency department, where she realized the need in her community for primary care services. As a result, she went back to school to pursue her doctor of nursing practice degree in family medicine from UNC Chapel Hill, from which she graduated in 2022.
While she sometimes misses her work as a cosmetologist, Cheryl said many of the skills she used in her salon inform the way she works with her patients today.
“Owning a business gave me confidence. I was introverted, but taking care of my clients gave me self-assurance,” Cheryl said. “I treasure the trust between me and my patients, and the skills I used behind the chair trickled down to patient care.”
Cheryl now practices at ECU Health Family Medicine – Kenansville, a multi-specialty family medicine clinic, and she loves her team.
“I am thankful for the people I work with and for the opportunity to work in a rural setting,” she said. “A lot of people have the misconception that in rural areas you don’t get to see as much as in other places, but we do. We get to see many things nurses don’t often get to experience – we have family medicine, orthopedics and cardiology all in the same place. We learn so much because the resources aren’t as vast.” Cheryl also enjoys working near her hometown. “I am not a city girl, and I knew I wanted to work closer to home. Now I get to take care of people in my own community,” she said. “I still get to take care of the ladies who sat in my salon chair; now I make sure they’re healthy.”
For those considering a career change to health care, Cheryl has a few words of wisdom. “I say go for it. If you’re not on the path that’s fulfilling you, take that first step. It’s never too late to do what you are meant to do; there’s no expiration date on your dreams.”
*Since this story’s production, Cheryl Hooks has left the health system.
It is no secret that ECU Health’s mission to improve the health and well-being of the region is directly tied to the success of recruiting the best providers, nurses and care teams. The ongoing labor shortage makes it more important than ever to have a compelling reputation that attracts a talented workforce committed to eastern North Carolina.

Trish Baise, ECU Health Chief Nursing Executive
During my first year at ECU Health as chief nursing executive, my team and I set out to gain a deep understanding of ECU Health nursing. The goal was to highlight and leverage the incredible strengths while also identifying the work needed to create and sustain a culture of nursing excellence. Our commitment is to ensure the organization fosters an environment where nurses can flourish, grow professionally and have a meaningful nursing experience while providing safe and highly reliable human-centered care.
This challenging work has already resulted in important achievements that affirm our standing as a world-class nursing organization. Most recently, ECU Health Medical Center achieved Magnet recognition – the highest national honor for exemplary nursing practice – for the third consecutive time, highlighting our commitment to creating a nursing ecosystem that embodies excellence. Less than 10% of hospitals in the United States have Magnet designation and ECU Health Medical Center is one of only eleven in North Carolina.
This achievement is the celebration of our collaborative work, but it is not the destination. We are just beginning our efforts to propel nursing at ECU Health to unprecedented heights, making it adaptable to the ever-changing health care industry.
The Path Forward for ECU Health Nursing
We are taking bold steps forward. At ECU Health, we are not just reacting to the future of nursing, we are defining it. We are co-designing an empowering environment for our nurses to innovate and excel, enhancing patient care, and setting a new standard for nursing excellence in rural health and beyond.
At the core of this work is an inclusive approach to re-imagining and elevating nursing at ECU Health we have named Advancing Nursing Practice and Excellence (APEX). It began as a broad research project, capturing the voices of our nurses across the entire health system to ensure we had a deep understanding and appreciation for our environment. We are using the information gained during this research to inform our nursing strategic plan and design the work ahead, ensuring our nurses are a part of it every step of the way.
APEX will be the model for nursing excellence, innovation, research and education in rural health and beyond. Unifying leadership, technology and evidence-based practices, APEX exemplifies the future of human-centered care.
Investing in Future Nurses
In addition to our APEX work, we are committed to strong partnerships and innovative collaborations alongside our academic partners in the region including East Carolina University and local community colleges to offer training programs for the next generation of health care professionals. Our nationally accredited Nurse Residency Program empowers graduate nurses to select from various clinical areas, aligning with their professional aspirations. Our structured, evidence-based program pairs new nurses with experienced mentors, fostering skill refinement and growth. Upon completion, participants gain practical experience, enhance critical thinking, and transition confidently into their nursing careers.
What This Means for Our Communities
Through our APEX work, ECU Health is cultivating a thriving nursing environment empowered and engaged to lead innovations that support improved quality of patient care and enhanced patient experience for those across our region. Together, with our nurses, we will be publishing our work – sharing the unprecedented work taking place in eastern North Carolina as we create the national model for rural health nursing excellence.
Our Magnet recognition is a reminder of ECU Health’s long-standing legacy of nursing excellence, and we are proud to propel that legacy into the future with these continued efforts. Additionally, our nurse residency program will play a vital role in training the next generation of nurses. By contributing to a healthier, more resilient community with improved health outcomes, we embody the state motto of North Carolina,“Esse quam videri,” which means “To be, rather than to seem.” This marks only the beginning of an incredible journey of continuous improvement and innovation for ECU Health. I take immense pride in our new strategic direction for nursing and feel privileged to collaborate with the best nurses in the country.





