When Tabitha Tripp, perioperative supervisor at ECU Health SurgiCenter, was initially approached to host Project SEARCH students for internship rotations in 2021, she hesitated. Already managing a full workload, she questioned whether would have the time to mentor a student. However, recognizing the significance of providing these students the opportunity to learn valuable job skills, she decided to embrace the opportunity.
“These students are some of the hardest workers I have ever supervised,” said Tripp.
Project SEARCH is a one-year internship program for students with developmental and intellectual disabilities during their last year of high school offered at ECU Health Medical Center in partnership with Pitt County Schools. Students complete internship rotations across departments like hospital cafeterias, endoscopy, ECHO Lab, Environmental Services and more, where they learn real-world job skills like cleaning, stocking supplies and changing linens.

“Many of our graduates have gained competitive employment in our community upon graduating from the program,” said Katie Houmard, Project SEARCH instructor. “The main goal of the program is to prepare students with the competitive and marketable skills needed to transition into the workforce.”
Three years after deciding to work with Project SEARCH students, Tripp continues to get excited every time she has a student from Project SEARCH at the SurgiCenter.
“These students have become like family to us,” Tripp said. “I cannot begin to explain how rewarding it is to see how much the students grow. I am honored to take part in the growth, maturity, independence and confidence they gain during the Project SEARCH program.”
“There’s lots of different opportunities and advantages to bringing Project SEARCH into the community,” said Lisa Lassiter, director of Workforce Development, ECU Health. “We are showing the value students with different abilities bring to the workplace, fostering growth within the students and our team members. The community is also engaging with our students so they have the opportunity to see the gifts and skills they possess.”
Cindy Ferry, whose daughter Caitlyn just graduated from the program, has noticed a huge difference in her daughter after completing the program.
“The growth in Caitlyn this last year has been amazing,” Ferry said. “Caitlyn spent four years of high school learning the same things over and over and was, of course, bored. But when she started at Project SEARCH, she would jump off the bus at the end of the day and run up to tell us everything she did. She couldn’t wait to tell us what she did, what department she was in and how she got to learn new skills like making a bed or putting gloves on or creating packets for patients.”
According to Matt Fornes, program manager and job coach at Project SEARCH, both the students and hospital team members benefit from the program.

“There’s a good relationship where the students are learning the skills, and the department is learning from them as well, so they grow mutually,” said Fornes.
For Ferry, that growth can be seen in her daughter every day.
“Her growth at home is absolutely, positively astounding,” said Ferry. “The things she’s doing now that she couldn’t do before such as helping set the table and cleaning up the table at the end of the day, helping in the kitchen. She wants to help now, and a lot of times she’ll now say, ‘Mom, I can do that by myself now.’”
Caitlyn is one of nine Project SEARCH graduates from the program this year and is part of its ninth graduating class.
“This program is really amazing, and so are all of the people who run the program,” said Ferry. “They really have the kids’ best interests at heart.”
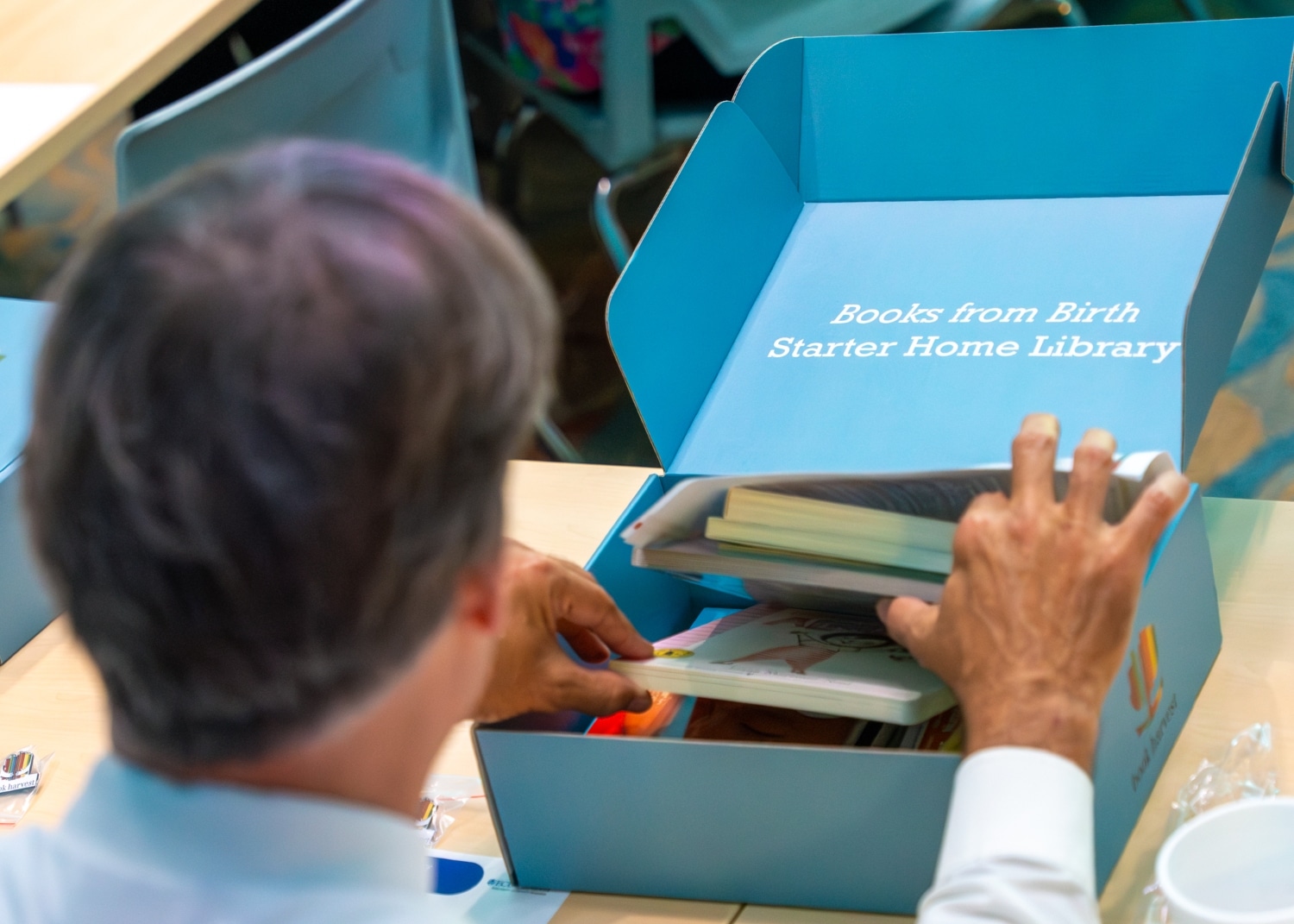
Books from Birth, a Book Harvest program, will begin providing children’s books to families of babies born in Maynard Children’s Hospital at ECU Health Medical Center starting in summer 2024. The books will help families foster early language and reading routines from a baby’s first days.
In preparation for the upcoming go-live, ECU Health hosted an event to educate team members at Maynard Children’s Hospital on Friday, June 14. Team members learned about Books from Birth, how these books can help families bond and improve early childhood education.
Book Harvest is an organization based in Durham that provides ongoing literacy support and an abundance of children’s books to families.
By partnering with Maynard Children’s Hospital, this collaboration will provide families and children in the East with the support and books they need to foster early language and reading routines at home from a baby’s very first days.
“The Books from Birth program is really designed to bridge early education and health,” said Book Harvest Chief Operating Officer Jeff Quinn. “Early literacy lays a foundation for life-long learning and healthy development. This program is meant to give children the opportunity to be what they want to be in life. We could not be more proud to help serve Pitt County and eastern North Carolina through this collaboration.”
N.C. House Rep. Tim Reeder, MD, District 9, secured funding of $500,000 for the project in the North Carolina State Budget. Rep. Reeder thanked Book Harvest and ECU Health for their willingness to partner on this important initiative. With his medical background in-mind, Rep. Reeder detailed the importance that early literacy has on the development of children as they grow, as well as the importance of improving access to education in eastern North Carolina.
“As a practicing physician, I see first-hand the benefits of early childhood literacy in terms of creating success in the classroom and in children’s behavior,” Rep. Reeder said. “Per data released from the state, about 50% of the children in Pitt County are not reading at grade-level. Early intervention and early reading is critically important to setting our children up for success. These books will help set families on a path to literacy that we know is really important to long-term development. I was proud to advocate for this funding and I am excited to see the impact this partnership will have.”
The Books from Birth program will provide a box of 10 board books, helpful reading education materials and a onesie for families who deliver babies in the Maynard Children’s Hospital.
“The benefit of giving these books at birth is that they help form loving and bonding relationships between babies and their caregivers,” said Dr. Matthew Ledoux, pediatrician in chief, ECU Health, chair of pediatrics, Brody School of Medicine at East Carolina University. “As a rural academic medical center serving a third of the state, it is incredibly valuable to get these books in the hands of families throughout eastern North Carolina. For that, we are very grateful.”
According to Tara Stroud, vice president, Women’s and Children’s Services, Maynard Children’s Hospital, the program will provide around 4,300 boxes of books to patients and families.
“This is our chance as a health system to change what it looks like for literacy in eastern North Carolina starting from the beginning,” said Stroud. “Our goal is that we demonstrate for our families the importance of books as a way to connect and bond with their child and improve their development.”

For Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center and Safe Kids Pitt County, the message she wants to get out is simple: “Never leave a child, senior or pet alone in a car, even for a minute.”
Walston’s message was amplified at a Hot Car Safety event in June hosted by ECU Health in partnership with the Pitt County Sheriff’s Office, Pitt County Health Department and the Martin-Pitt Partnership for Children, to demonstrate how quickly cars heat up.
The event included a demonstration with temperature gauges and s’mores roasting in a vehicle on hot, summer day. During an overcast, 88-degree day, the interior of the van rose to 113 degrees within 15 minutes.
The s’mores demonstration showed how quickly things can, quite literally, cook inside of a car when left alone. Volunteers handed out the s’mores to shoppers to explain the demonstration in a fun, interactive away.

“We host these types of events to raise awareness so parents are realizing how hot cars can become,” said Walston. “A car can heat 20 degrees in as quickly in 10 minutes. In our display today, it is already 113 degrees, and it’s only 86 degrees outside.”
According to Walston, about 17 percent of hot car fatalities occur in children intentionally left in the car. During this time, parents or caregivers are often running into the store or running an errand for a few minutes, thinking that will be fine.
“A lot of times, people think ‘I’m just going into the store for a few minutes,’ but anything could happen inside, from losing track of time to becoming distracted and forget the child,” Walston said. “There is a misnomer that if you crack a window and that will offer some less heat, but that really is a myth. It doesn’t affect the temperature of the car or cool the temperature down.”
Walston said it’s dangerous for anyone to be left alone in a vehicle because of how quickly they can heat up, but especially for children.
“Children’s bodies heat three to five times more quickly than adults,” Walston said. “They all have a smaller amount of body surface so they can’t cool themselves very quickly. A small child, like the families we’re serving today, they can’t verbalize when they’re thirsty if they’re under a certain age.”
More than 50 percent of child deaths from hot cars are children forgotten in vehicles, according to Walston. She said children can be forgotten when routines are broken, and leaving something like keys, a cellphone or a briefcase in the backseat next to the child or setting an alarm on your phone are extra safety measures one can take to ensure the child is not left in the car.
Walston encouraged attendees to call 911 if they ever see a child, senior or pet alone in a call.
“This is something parents really need to take seriously,” said North Carolina Insurance Commissioner Mike Causey. “It’s year-round, not necessarily just during the hottest months of the summer. We have had children die in November and other months outside of June, July and August.”

Keeping patients safe while they receive high-quality compassionate care is at the heart of what ECU Health does for eastern North Carolina. This is especially important to Dr. Teresa Anderson, ECU Health’s senior vice president for Quality, who recently celebrated her induction into the East Carolina University (ECU) College of Nursing Hall of Fame.
She joins a number of colleagues, mentors, friends and former classmates in the Hall of Fame, which recognizes the accomplishments of ECU’s exemplary nursing graduates and faculty members.
When Dr. Anderson enrolled at ECU, nursing school was not the path she thought she’d take. She started out in education but after a semester of tutoring, she realized it was not her passion. She started on her nursing course work and never turned back.
“I always had a heart of service,” she said. “Then I got into nursing school and on we went. I actually started at [ECU Health] Medical Center in 1996 as a nursing assistant while I was in nursing school. I hit 28 years of service this May.”

Over those 28 years, Dr. Anderson has worn many different hats. From the nursing assistant role to a bedside nurse and working in various medical roles before taking on management and administration, she believes her varied experiences have helped her be successful in her current role in Quality.
Along with the variety of her work and the mentors she has learned from, Dr. Anderson said it’s the patients and ECU Health’s commitment to improving the health and well-being of eastern North Carolina that keeps her coming back each day.
“Our mission and the population that we serve are special and important to me,” Dr. Anderson said. “We serve a very complex population. I know that we’re doing so much good for our patients and our community, and there’s so much more we can do now alongside the Brody School of Medicine. There’s just going to be so much more that we can do with population health and making sure that people get all the services and access to care that they need.”
Dr. Anderson is a three-time ECU graduate with her bachelor’s, master’s and doctorate degrees from the university. She’s also been recognized as a Great 100 nurse in 2016 and received a Leadership DAISY Award in February of 2021.
Dr. Amy Campbell, a quality nurse specialist at ECU Health and an ECU College of Nursing Hall of Fame inductee last year, submitted the nomination for Dr. Anderson to be admitted to the Hall of Fame. In the nomination, Campbell noted that Dr. Anderson is an outstanding role model and mentor who influences positive change while recognizing her team’s accomplishments.
“Over the years, she has served in many leadership and administrative roles that have led to improvements in patient outcomes. In addition, she has served on numerous community boards and enhanced the lives of Pitt County Residents,” Campbell wrote in her nomination. “On a personal note, Teresa has been a mentor to me personally and professionally over the last 14 years. She encouraged me to go back to school of my Ph.D. and was an active member of my dissertation committee. She has walked with me through tough times and give me priceless feedback to help me grow. I cannot think of anyone more deserving of this award.”
Dr. Anderson said she was humbled and grateful to have been nominated and accepted into the Hall of Fame. Hall of Fame members, new and former winners along with family and friends, attended a ceremony and had their nomination letters read before they were presented with a plaque to honor their induction.
Members of the Hall of Fame help fund a scholarship for the next generation of nurses and Dr. Anderson said this was one of the most special parts of the recognition for her.
“They showed a video from one of the recipients of the scholarship money at the event,” Dr. Anderson said. “She talked about how much it meant to her and it was very nice to know that the money collected goes to a great cause and to fund students in need. She talked about making ends meet and paying rent and all of her work in school. I remember those days, so it feels great to give back to future nurses.”
Resources
To be a health care provider is to answer a calling. For some, the journey to health care is a straight line; for others, the road is winding. This series features stories from ECU Health team members who took the winding road, but found the destination to be worth the effort.
Virginia native Suzanne Foster moved to New Bern in 2007 because of her husband’s work; at the time, she served as an operations manager in sales and marketing for a small internet company. “We primarily did financing for military and government employees,” Foster said. When her father became terminally ill, she found herself as his primary caregiver when he transitioned to hospice.
“Taking care of him through hospice was very eye opening,” she said. “It made me realize that my job didn’t really matter. What mattered was taking care of him.”
It was then Foster realized she wanted to become a nurse. Her brother, who had just been accepted to medical school, also supported her shift in priorities. “He said, ‘This is what you need to do,’ and it turns out he was right.”
Suzanne attended Craven Community College, and now she’s been a nurse for nearly eight years. Recently, she found herself drawn to work as a travel nurse, which is what brought her to ECU Health*. “I wanted to try travel nursing and experience other facilities, but I have a husband and a son I dearly love and don’t want to be away from,” Foster said. That’s what made a travel position at ECU Health Medical Center a perfect fit, even if it was something she was initially apprehensive about.
“I had always been at one little hospital,” Foster said. “It was intimidating coming to a larger hospital like the medical center.” But one of Foster’s friends assured her she’d love it. “And she was right, the staff on the Medical ICU where I work is incredible.”
The Medical ICU was the right fit, Foster said, “because it’s kind of a hodgepodge or catch-all. You get to do the MacGyver stuff because we catch everything that requires intensive care and not just strokes or heart attacks.”
She also enjoyed that the medical center was a teaching hospital, something she had not previously experienced.
“Where I worked before, we had four or five regular intensivists, and I could pretty much anticipate a plan of care from that rotating group,” she explained. “Now I get to experience a teaching hospital, which has been eye opening. I get to take care of patients with residents – medical students – and it’s fun because they want to learn. The difference between working in a small hospital and a teaching hospital has taken a little adjustment, but it’s been a lot of fun and exciting.”
Foster had nothing but great things to say about her transition to nursing and her travel nursing experience at ECU Health.
“I absolutely recommend it,” she said. “Whenever friends say they’re really thinking about nursing, I tell them the medical center is a wonderful facility. You get to be at the bedside and have fun, and you work with awesome nurses with impressive skill sets.”
Ultimately, her transition to nursing has allowed her to do what she feels is important: take care of people.
*Suzanne Foster worked as a travel nurse at ECU Health Medical Center from October 24, 2022 to October 21, 2023.
Greenville, N.C. – ECU Health is partnering with Food Lion Feeds, Sodexo and the ECU Health Foundation to provide free meals for kids, teens and people with disabilities as part of the Summer Meal Program. Meals will be available in Greenville, Bethel and Ahoskie. The selected sites this year were chosen based on the need in each county, existing partnerships and the social vulnerability index at each location.
During the school year, many kids and teens receive free or reduced-price meals. When schools close for the summer, those meals disappear, leaving families to choose between putting the next meal on the table or paying for other necessities like utilities or medical care. While over 57% of students in North Carolina receive free or reduced lunch, 66% of Pitt County students and over 90% of Hertford County students receive free or reduced lunch.
Meals will be available until food runs out each day at the following locations:

- Greenville: English Chapel Free Will Baptist Church – 11:30 a.m. to 1 p.m., Monday-Friday from June 10 to Aug. 23. The location will be closed July 22-26.
- Ahoskie: Calvary Missionary Baptist Church – 11:30 a.m. to 1 p.m., Monday-Friday from June 10 to Aug. 23. The location will be closed June 19 and July 4-5.
- Bethel: Bethel Youth Activity Center – 11:30 a.m. to 1 p.m., Monday-Thursday from June 17-July 17. The location will be closed July 3-7.
ECU Health has offered the Summer Meal Program since 2021, providing nearly 12,000 free meals to kids and teens during the summer months. In 2023, 51 ECU Health team members served more than 2,800 meals to kids in need.
No registration is required. For more information about the ECU Health Summer Meal Program, please email [email protected].
Greenville, N.C. – Project SEARCH, an educational program offered at ECU Health Medical Center, is proud to announce nine students recently graduated from the program: Camarion Allred, Jordan Bell, Kevin Caudle, Caitlyn Ferry, Region Jenkins, Nicholas Tripp, Xavier Vaughan-Holliday, Eric Williams and Maxwell Wilson. Project SEARCH is a one-year internship program for students with developmental and intellectual disabilities during their last year of high school with the goal of providing real-world practical skills and increasing the chances of competitive employment.
“ECU Health is very proud to host Project SEARCH to bring educational opportunities to everyone in the East,” said Doris Hill, Project SEARCH coordinator at ECU Health. “This program gives students the opportunity to learn job skills that can be applied after graduation and brings diversity to our organization and the local workforce. We are proud of the tremendous growth of our nine graduates throughout the program, and we are all very proud of their accomplishments.”

The Project SEARCH program at ECU Health Medical Center began in 2015 through partnerships with Pitt County Schools, RHA Health Services and the North Carolina Division of Vocational Rehabilitation Services. Students complete internships in various departments at the hospital, including the ECHO Lab, Endoscopy Center, Environmental Services, SurgiCenter, hospital cafeterias, Hospitality and the Neuroscience Intermediate Unit.
“Project SEARCH gives our students support to transition into the workforce through skills development and a customized job search in the second half of the program,” said Katie Houmard, Project SEARCH instructor. “This program grows confidence and independence in all our students, and many of our graduates have gained competitive employment in our community. I am so proud of all our students and am excited to see them continue to grow and become employed.”
The employment rate for youth with disabilities is about 60 to 70 percent less than youth without disabilities, according to the Office of Disability Employment Policy. Project SEARCH has proven results with a 65 percent employment and 90 percent retention rate nationally.
Students who participate in the program are enrolled at various Pitt County high schools including J.H. Rose, D.H. Conley, South Central, Farmville Central, North Pitt and Ayden-Grifton. This is the ninth graduating class.
The Project SEARCH program began in 1996 at Cincinnati Children’s Hospital Medical Center (CCHMC) and was developed as a means to meet entry-level employment needs at CCHMC, support their diversity initiative and partner with schools and community services agencies. Project SEARCH is now an international program with over 716 program sites in 48 states and 11 countries.
After graduating from East Carolina University with a Master of Social Work (MSW), Breanna Culler moved away from her hometown of Stokes, North Carolina, to live and work in Poughkeepsie, New York. Then one day she received a call from Sue Anne Pilgreen, manager of the Eastern Carolina Injury Prevention Program (ECIPP) and the Pediatric Asthma Program at ECU Health.
“She’d gotten a grant for a Suicide Prevention Coordinator for ECIPP and needed to find someone to fill that position,” Culler said. “My previous internship field supervisor and a professional colleague gave her my name and she called me up.”
Culler ended up getting the job and moved back to North Carolina. Just a year after starting her new role, Culler was approached about serving as a social work field instructor for a graduate student. This year, Culler was awarded the East Carolina University School of Social Work Outstanding Field Instructor award in recognition of the work she’s done with social work graduate students.

Culler’s work primarily centers on firearm safety, safe storage of firearms and suicide prevention, specifically for veterans and LGBTQ+ individuals.
“I struggle to describe my job because our team does so much, but we provide resources and education through formal trainings such as Counseling on Access to Lethal Means (CALM) and less formal settings such as community events,” Culler said. “I am a co-lead with the Pitt County Firearm Safety Coalition, which includes law enforcement, medical providers and others from across Pitt County, and I work closely with Veteran’s Affairs and the Dr. Jesse R. Peel LGBTQ Center at ECU, along with other agencies across eastern North Carolina. If we’re not out providing education, we’re in the office preparing a program or connecting with new agencies.”
Culler said a challenge to developing these programs is how to customize the content based on location.
“Greenville is very different from other communities,” she explained. “Figuring out how to connect to rural populations and make this information and education relevant to folks living on the outskirts of town — that’s very important to me both on a professional and personal level. You have to think about those things to make any program sustainable and impactful.”
ECIPP does this by finding innovative approaches to the challenges associated with firearm safety and suicide prevention.
“For example, there are many health systems that partner with law enforcement agencies regarding firearm safety,” Culler said. “But we realized a lot of people get their guns from pawn shops, so we have initiated relationships with pawn shops around eastern North Carolina as a creative avenue to spread suicide prevention education and firearm safety resources.”
Along with her firearm safety work, Culler also partnered with the Safe Communities Coalition and Pitt County Students Against Destructive Decisions (SADD) to launch the You Belong Here campaign which aims to reduce suicide among LGBTQ+ youth.
“This is our other major project, as it encompasses a documentary, resource library, allyship education, parent support group and a therapy fund,” Culler said. “We started the therapy fund as a part of You Belong Here and created a partnership with mental health providers, linking those people with providers and giving financial coverage for that care. We’ve been able to share it both nationally and across the state, which is pretty cool.”
As a result of that creativity and hard work, Culler was approached early-on about taking a MSW student from ECU.
“I was only 24 and was nervous,” Culler said. She had great field instructors when she was a student, and that influenced her own interactions with her interns. “The thing I’ve enjoyed the most is seeing how the students see a new side to social work.”
Students may expect to work in child welfare or social services, but with Culler, they get to see a more community-based, out-of-the-clinical-box advocacy and education.
“Breanna is very intentional in allowing her students to play an integral part of the program development, implementation and evaluation of whatever they are doing,” said Pilgreen.
That’s why Pilgreen was not surprised when she learned that Culler had won the ECU School of Social Work Outstanding Field Instructor award. Culler, however, didn’t even realize she’d been nominated for the award until she found out she’d won.
“My intern nominated me, but I didn’t know, so it was very much a surprise,” she said. “I was excited to win the award in general, but that my intern nominated me made it much more special.”
The award recognizes student supervisors for their commitment to providing a rich learning environment and their dedication to educating the next generation of social workers while also exemplifying professional social work qualities.
“Breanna’s most recent intern played a huge role in the North Carolina Youth Suicide Prevention Symposium we hosted in March,” Pilgreen said. “The intern has a special interest in research and data collection, and she’s now working toward submitting conference presentation abstracts and a manuscript with Breanna’s guidance.”
In addition to her work, Culler now plans to become a North Carolina Licensed Clinical Social Worker. Doing so will allow her to practice independently or clinically.
“I have the degree, so I just need to go through with getting the clinical training hours to get become licensed,” she said. “Then I can become a provider serving the same communities where I work now.”
The grant funding Culler’s position was set to run out on Aug. 31, 2024, but Pilgreen recently received an unexpected call from NCDHHS asking if they could extend Culler’s position and programmatic funding for another year.
“This is unheard of,” Pilgreen said. “It only happened because of the amazing work that Breanna has not only done as a social work field instructor, but also as an avid advocate in the field of suicide prevention and firearm safety.”
Culler said she loves the work she does and was surprised to find out she had an additional year of funding.
“I love working in community health and with the prevention team,” she said. “I love the team I work with – they’re like a family. I appreciate being a part of a system that’s invested in my home.”
ECU Health emergency medicine residents took time away from their regular Wednesday morning classroom sessions and dove into an Emergency Medicine Wilderness Day exercise at Wildwood Park in Greenville.
On May 29, about 20 emergency medicine residents spent their morning in small groups, walking around the park and encountering “patients” with different ailments. From poisoning to animal attacks and drowning scenarios to firework accidents, the experience helped residents prepare for real-world scenarios and eventual board exams. Residents received real-time instruction and feedback from the Brody School of Medicine at East Carolina University faculty as they worked through their training.
The patients for this exercise were standardized patients from Brody’s Office of Clinical Skills Assessment and Education. Standardized patients are trained to mimic real patients so that students can learn. Their role is to help prepare future health care professionals for a variety of patient interfaces.

Dr. Sarah Thead is a second-year emergency medicine resident at ECU Health and said she’s attended the training the last two years and has benefited from the experience.
“It’s a great educational experience every time we do this,” Dr. Thead said. “It’s scenario-based and our faculty try to set up the scenarios similar to how they’ll be set up on our oral board exams, so it’s a fun experience but also really important from an educational perspective as well.”
She said the scenarios change from year to year which helps her and her co-residents as they try to work together and think quickly to help patients experiencing a medical emergency.
Dr. Jennifer M. Bennett, an emergency medicine physician at ECU Health, clinical assistant professor of emergency medicine and medical director of the Simulation Center at Brody, said this kind of exercise is important for a number of reasons.
“It’s a great opportunity to demonstrate how we can all work together, even outside of the emergency department. It’s important to work on these skills in a different environment,” Dr. Bennett said. “It’s also a good opportunity to have some team bonding for the residents. Just getting them out for a day and letting them do something a little bit different, getting them out in the sun, that’s a positive as well.”
Dr. Bennett said having Wildwood Park available to run this exercise has helped this program thrive over the last three years.
Along with Dr. Bennett, Dr. Jennifer Parker-Cote, assistant professor of emergency medicine at Brody, helped to create the simulation and organize the event.
In Dr. Parker-Cote’s simulation, residents had to assess a camper who had ingested a toxic mushroom in the woods. Residents assessed the standardized patient, asked about the patient’s medical history and made recommendations on next steps for care.
“These scenarios allow residents to apply the knowledge they’ve gained through their residency and apply it to real world situations and permits them to improvise in wilderness medicine, which you have to do a lot of times,” Dr. Parker-Cote said. “It’s important to put them through these simulations and have them think critically while working together and trying to move quickly to help our standardized patients.”

The training is another example of the valued partnership between ECU Health and Brody. Residents at an academic health system like ECU Health have support and resources for continued education from faculty and the Interprofessional Clinical Simulation Program at Brody, enriching their clinical training experience. Residents participate in trainings like this to prepare for real situations with real patients both behind the walls of the hospital and out in the community.
Resources
Updated June 19, 2024
A beam adorned with signatures from ECU Health team members, behavioral health care teams, leadership and the Thomas Construction team was raised into place at the site of the upcoming behavioral health hospital in Greenville.
The beam raising served as a backdrop for an event showcasing the construction progress of the new 144-bed behavioral health hospital, a partnership between ECU Health and Acadia Healthcare, slated to open in summer 2025. ECU Health and Thomas Construction team members paused their important work to witness the historic milestone.
Glenn Simpson, service line administrator for behavioral health at ECU Health, said this event was another historic step, celebrating about 15 years of work to bring a behavioral health hospital into the ECU Health system to serve eastern North Carolina.

“Today is only the beginning of so much excitement around this facility,” Simpson said. “We couldn’t be more excited to be partnered with Acadia Healthcare and working with Thomas Construction to build this facility. This is all allowing us to offer outpatient services, specialty services that we cannot provide today and we’ll be able to treat a population of children and adolescents who used to have to drive over 70 miles for inpatient treatment.”
Mary Branch-Ellis, a registered nurse with the behavioral health team at ECU Health Medical Center, has been with the system for 41 years. She said she was working at the former Pitt County Memorial Hospital years ago when the behavioral health unit first opened in the 1980s.
She said seeing the facility come together is something she will never forget and she’s glad eastern North Carolinians in need of the services will have everything under one roof.
“It’s just wonderful to be a part of this as someone who is invested in this work in eastern North Carolina,” Branch-Ellis said. “I’ve worked so many years in mental health and been an advocate for patients and now we’re seeing this state-of-the-art facility being built and it’s a wonderful experience to see these beds – which we need – opening up. I’m excited to see it coming to Greenville and I’m proud to be a part of it.”
ECU Health team members sign beam slated for upcoming behavioral health hospital
Recently, ECU Health team members had the opportunity to leave their mark on the upcoming state-of-the-art, 144-bed behavioral health hospital in Greenville, slated to open in 2025.
The Thomas Construction team brought a beam, which is slated to be installed in the hospital’s gymnasium, to ECU Health Medical Center for team members to sign. More than 100 team members signed the beam and many signatures will be visible in the gymnasium even after construction is complete.
Amy Albritton, a recreational therapy assistant in Behavioral Health Services, has been with the system for more than 25 years. She said it’s special for her to see the plans for the new hospital come together after her years on the unit.
“I think being able to see the beam and sign it helps make it a little more real,” Albritton said. “It’s been talked about for a while now but having this here that we can touch, it’s a really exciting time. I’m just glad to be a part of it.”

Glenn Simpson, service line administrator for behavioral health at ECU Health, said engaging team members in the lead up to the hospital opening is a great opportunity for education and building excitement.
“With building a brand-new hospital, it’s special to give our team members the opportunity to be part of the history of that by signing one of the beams,” Simpson said. “When they’re finished with the gymnasium part of the structure, they’ll be hoisting the beam into the framework. This is great for team members to sign the beam and know that their name will forever be a part of that hospital.”
Renderings of the upcoming hospital were also on display during the beam signing to allow team members to see the plans again. The beam was in the hospital for about a week before being returned to the construction site.
To learn more about new behavioral health hospital, please visit: ENCBehavioralHealth.org
