Meet Clive, ECU Health Medical Center‘s resident canine.
“Currently, he’s working two days a week with us,” said recreational therapist and dog handler Kasey Shue. “Some mornings when we go through the hospital doors, he’s just like, on a mission. I have to be like, ‘Clive, wait, hold on, buddy. You’re like, ready to roll this morning’. So I think he knows what he’s here to do.”
It’s an assignment he’s well prepared to tackle.
“A service dog is specifically trained to do certain tasks for somebody with a disability,” said Clive’s owner and outpatient rehab supervisor Tanya Bowen. “So a therapy dog is basically to provide comfort and they have to be very friendly and outgoing because there’s a lot of people that want to pet them and touch them. They have to be calm. They have to like the interaction, the social interaction. So he’s kind of like a little combination of both.”
Clive’s skill set benefits patients in a number of ways, whether that’s assisting with physical needs or providing emotional support.
“We’ll partner up with a physical therapist or an occupational therapist and we’ll work on walking him if they’re working on mobility improvement,” Shue said. “We’ll work on throwing a ball if they need some hand strengthener. We’ll work on them being able to pick up a very small treat and hand it to him if they have fine motor limitations. We really try to incorporate him into whatever functional skills they are trying to learn to make their life easier when they get home. On the other side, many times we have patients that are depressed or anxious. They don’t like being in the hospital and he just provides that comfort.”
And his services are in demand at the bedside and beyond.
“He actually wears a vest that says, I’m friendly, please ask to pet me,” Shue said. “We absolutely encourage that because he is therapy for our patients, but he’s also therapy for the staff, the families.”
Resources
ECU Health Therapy & Rehabilitation
Watch more ECU Health News videos
Leaving a child, senior or pet behind in a car can pose serious danger, even if it’s just for a few minutes.
That was the message of the hot car safety event hosted by Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center, along with the Pitt County Health Department and the Martin-Pitt Partnership for Children.
Walston said it’s dangerous for anyone to be left alone in a vehicle because of how quickly they can heat up, but especially for children.

“Children’s bodies heat three to five times more quickly than adults,” Walston said. “They all have a smaller amount of body surface so they can’t cool themselves very quickly. A small child, like the families we’re serving today, they can’t verbalize when they’re thirsty if they’re under a certain age. You really have to be very careful. The message is never leave a child alone in a car, not even for a minute.”
The team had a demonstration with temperature gauges and s’mores roasting in a vehicle on an 80-degree day, one of the coolest days in recent weeks in eastern North Carolina. Despite the cooler than normal temperatures, the interior of the van rose to 90 degrees within 15 minutes, over 100 degrees after an hour, and approached 120 degrees in an hour and a half.
The s’mores demonstration showed how quickly things can literally cook inside of a car when left alone.
“As you see we have this temperature gauge here and just in the last 15 minutes, it’s already gone up 10 degrees,” Walston said. “This is a white car with light interior, and with a dark car and dark interior it can heat the car more quickly.”
Walston noted that there have already been 10 deaths across the country this year from children left alone in cars. In North Carolina, we have seen one this year and another in neighboring Virginia.
She said more than 50 percent of child deaths from hot cars are from children that have been forgotten in vehicles. She said children can be forgotten when routines are broken and leaving something like keys, your cellphone or a briefcase in the backseat next to the child is a safe way to ensure the child is not left alone.
According to Walston, about 17 percent of hot car fatalities are children that are intentionally left behind. She said no amount of time is safe for a child to be left alone, even with windows cracked.
“Many times folks think that, I’m just going into the store for a few minutes, but anything could happen inside, you could become distracted and forget the child,” Walston said. “There is a misnomer that if you crack a window and that will offer some less heat, but that really is a myth. It doesn’t affect the temperature of the car.”
The North Carolina Coalition of the Year award is based on the coalition’s positive outcomes of the child passenger safety program, medication safety programs and maintaining partnerships.
“It was a huge surprise,” Injury Prevention Program coordinator at ECU Health Medical Center Ellen Walston said. “Lisa Blackmon with Safe Kids NC said our social media really was the catalyst for winning the award. We post multiple times a week on our risk areas in injury prevention, and it’s just really important to use those quick soundbites to get the word out.”
Preventable injuries are the number one cause of death in kids in the United States, according to Safe Kids. That’s why Safe Kids Pitt County works to prevent injuries in children and adults through simple tips and safety checks. The Safe Kids Pitt County team strives every day to keep kids in eastern North Carolina safe and healthy and to meet ECU Health’s mission of improving the health and well-being of eastern North Carolina.

A “hallmark” program
Walston called the child passenger safety program the hallmark of the coalition’s work. The program began in the early 2000s and, along with pop-up opportunities for car seat inspections, Safe Kids Pitt County has a permanent checking station. The permanent station is located at the Winterville Fire Department and is available on the third Friday of each month, 1:30-4:30 p.m.
“To me that parent’s expression of appreciation is priceless,” Walston said. “When they walk in, they just have that look of ‘I don’t know how in the world to put this seat together. Will you please help me?’ Then when they leave, you ask them ‘Are you confident in being able to put this seat in yourself?’ You just see that anxiety just melt away. That to me is the most comfort, knowing that we’ve made a difference.”
More than half of car seats are not used or installed correctly, according to Safe Kids. Correctly used child safety seats can reduce the risk of death by as much as 71 percent.
The child passenger safety program also covers free child safety seat checks when someone has received a violation, citation or ticket. The child and parent will receive one-on-one education to help ensure correct car seat installation, and the program also offers hot car safety information sessions, as well. For more information on this program or general car seat inspections, contact Walston at 252-847-8532.
Medication safety
Medication safety was another key driver for the award, and Operation Medicine Drop is an event that helps the public dispose of expired, unused or unwanted prescription drugs or over-the-counter medications. The event serves to protect children, our community and the environment. Medicines are the leading cause of child poisoning, and proper disposal of medications can largely prevent them from happening. The valuable education sessions offered throughout the community on medication safety help to reduce unintentional poisoning from prescription medications, which is on the rise in North Carolina.
Walston said the opportunity to connect with families and children is vital to the program’s success.
“We have a lot of anecdotal affirmation from children on this kind of education session,” Walston said. “I will see children in the store and they’ll say, ‘Miss Ellen, you came to my school and talked about fire safety’ or ‘You were at the park in Winterville and taught us about medication safety.’ Just making those contacts is so important, we never know when we’re planting that seed. Those children can go home and tell their siblings and tell their families what they’ve learned.”
Key Partnerships
Working with a small internal team makes it crucial to have great partnerships, Walston said. Safe Kids Pitt County primarily partners with Martin-Pitt Partnership for Children, ECU’s TEDI BEAR Children’s Advocacy Center and the Pitt County Health Department. Other partners include Greenville Fire Rescue, Winterville Fire Rescue, Pitt County Sheriff’s Department and Greenville Police Department.
“We’re so blessed with partnerships. I cannot do this work alone,” Walston said. “I just enlist partners, I’ve learned to delegate, I ask for help when I need it. We’re a small team but mighty and we get a lot done.”
Walston also shared appreciation for ECU Health Medical Center, the lead agency for the Safe Kids Pitt County coalition.
“I really want to emphasize a big thanks to ECU Health Medical Center for being here for us since 1995,” Walston said. “They provide all the technical support for me to be in this role – my office, the hours that I designate. We’re really blessed. A lot of hospitals are lead agencies but [other coalitions] don’t get the same support that I’ve received from the hospital.”
Past Recognitions
This is the second time Safe Kids Pitt County has received North Carolina Coalition of the year, first taking home the award in 2010. Other past recognitions include Safe Kids NC Outstanding Outreach Initiative and NC Child Passenger Safety Outreach Program of the Year award in 2016, as well as Walston earning Coordinator of the Year in 2013.
Learn more about Safe Kids Worldwide here.
The 2022 ECU Health Board Quality Leadership Award winners were recognized at the ECU Health Board of Directors meeting on June 28. These winning teams are shining examples of excellent work in driving the quality goal of zero harm, creating exceptional experiences and improving patient outcomes.
Team members were required to submit projects that demonstrated at least two of the following criteria:
- Quantifiable improvement in an organizational quality priority with sustained excellence over time
- Demonstrable empathy and compassion in patient care
- Implementation of innovative solution to patient care problem
- Community outreach that addresses social determinants of health in a meaningful way
Nineteen nominations were reviewed by the committee. Congratulations to the winning teams:

Improving Blood Pressure in Control
Aimed to improve blood pressure control, less than 140/90, in ACO hypertensive patients to 75% within the fiscal year, as measured by Care Evolution.
- David Lewis, MD
- Penny Coltrain, BSBA, MBA
- Wendy VanLandingham, BSN, RN, LSSBB
- Nicole Lewis
- Sharonda Nicholson-Bradley, RN
- Gail Scheller
- Faith Garrett
- Robbie Webber
- Sherry Bowers

Curbing Contamination: Reducing Blood Culture Specimen Rejection
Aimed to improve patient outcomes by achieving and sustaining a hospital-wide blood culture (BCX) specimen contamination rate of ≤ 3%.
- Krista Horne, MSN, RN
- Christine Miller, MBA, RN
- Elizabeth Lanier, MLT
- Sharlene Blizzard, BSCLS, MLS (ASCP)CM
- Ashley Sholar, MBA, BSN, RN

For the Love of the Line – Central Line Associated Bloodstream Infection (CLABSI) Reduction Project
Aimed to decrease CLASBI by 5% by at ECU Health Medical Center by April 2021.
- Erin Pearson, BSN, RN, QNS
- Jamie Hall, BSN, RN, CIC, IP
- Takisha Williams, MSN, RN, NPD-BC
- ECUHMC Nurse Leadership, Physician Leadership
- ECUHMC Supply Chain
- ECUHMC Professional Development Specialist Team
- ECU Health Infection Control
- ECU Health Performance Improvement/ Quality Analytics
Thank you to all the nominees for their hard work and dedication. This is one example of our teams reinforcing our mission to improve the health and well-being of eastern North Carolina and pursue excellence in our values and Quality imperative.
With our continued focus on the imperatives of quality, experience and finance, ECU Health’s transplant program at ECU Health Medical Center has consolidated their treatment and office spaces into the newly renovated 3 South. The area is now known as the 3 South Transplant Clinic.
The transplant program performs an average of 80 to 100 living and deceased donor kidney and pancreas transplants per year. Patients that are seen in the clinic include pre-transplant (patients being evaluated for transplant), living donors and post-transplant. This program and the services offered have continued to grow over time, but have been limited by clinic space. To enhance patient and team member experience, the pre- and post-transplant clinics have now consolidated into one, centrally-designed space on 3 South, as they have been operating in separate clinics at the Cancer Center and ECU Physicians.
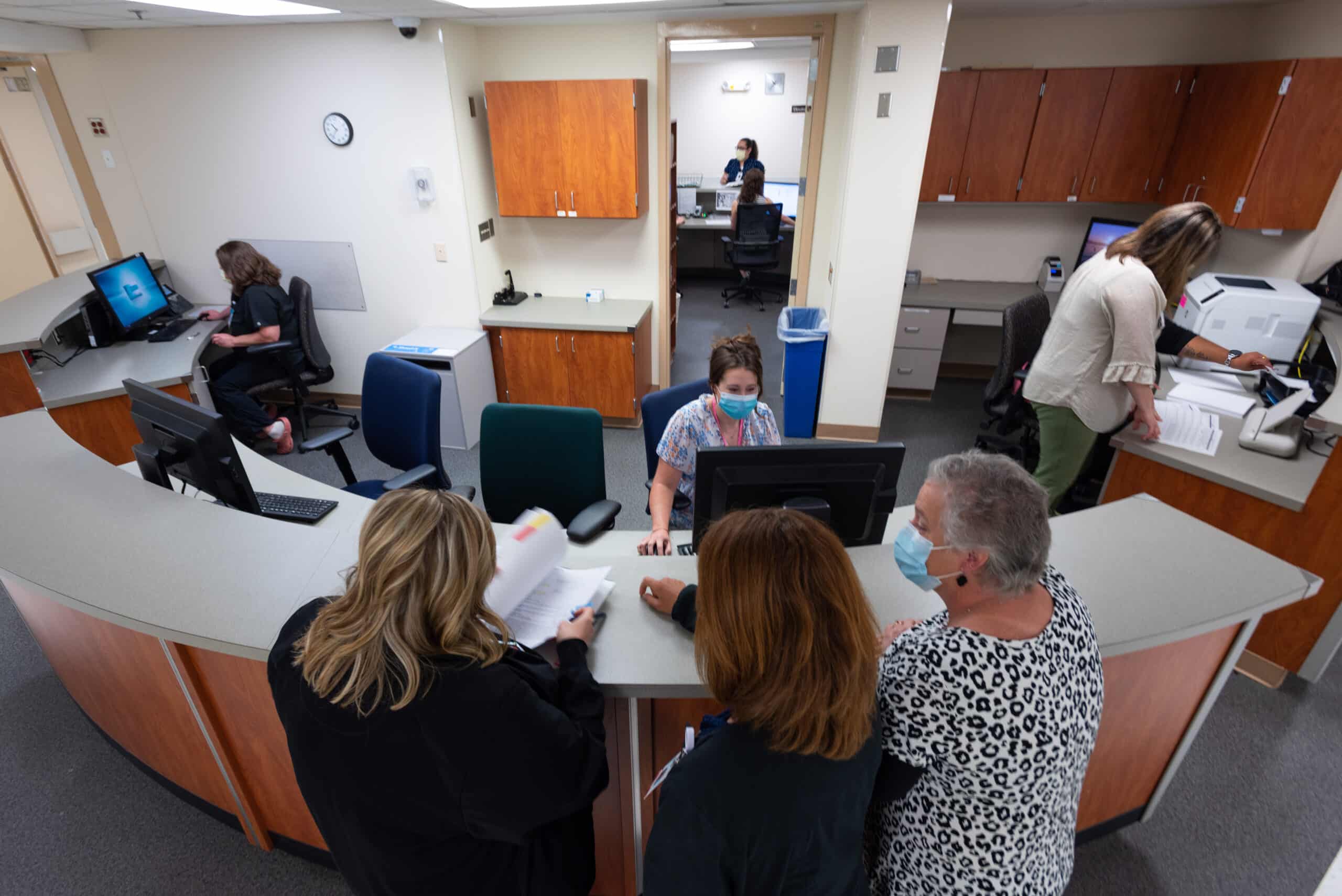
Previously, the transplant team worked in separate clinics, sometimes limited to three rooms. 3 South Transplant offers 18 patient exam rooms, which in addition to consolidating space for patients, will also help to shorten wait times for new referrals and follow up appointments.
Another benefit of 3 South is the accessibility of team members such as dieticians, social workers, pharmacists, nurses and physicians, which provides patients the accessible support of various teams of health care workers critical to patients’ transplant journeys.
Lastly, this consolidation allows for expansion of potential future services such as phlebotomy, expanded pharmacy services, infusion services and vascular access.
In 2022, as we build the future of ECU Health, the exceptional care and services we provide have a positive impact on the communities of eastern North Carolina that we serve through our considerations of patient quality and experience.
For more information on transplant services at ECU Health, visit the transplant section of our website.
Younger people are increasingly suffering from strokes according to medical experts at ECU Heath. While risk of stroke increases with age, health care teams have seen an increase in strokes in young people, partly due to a combination of COVID-19, an increase in consuming processed, sugary and fatty foods as well as smoking and vaping.
“With COVID-19, we have noticed an increase in strokes, especially in younger populations,” said Dr. Shailesh Male, stroke medical director, ECU Health Medical Center. “During the peak of the pandemic, my colleagues and I noticed that young patients who do not have vascular risk factors were having strokes. COVID-19, like other infections, increases the risk of forming blood clots and, in turn, can lead to higher risk of strokes.”
Strokes are considered the heart attack of the brain. A stroke occurs when a blood clot compromises blood flow to the brain. This leads to loss of brain function, manifesting in symptoms including: weakness or numbness on one side of your body, slurred speech or difficulty understanding others, blindness in one or both eyes, dizziness and/or a severe headache.
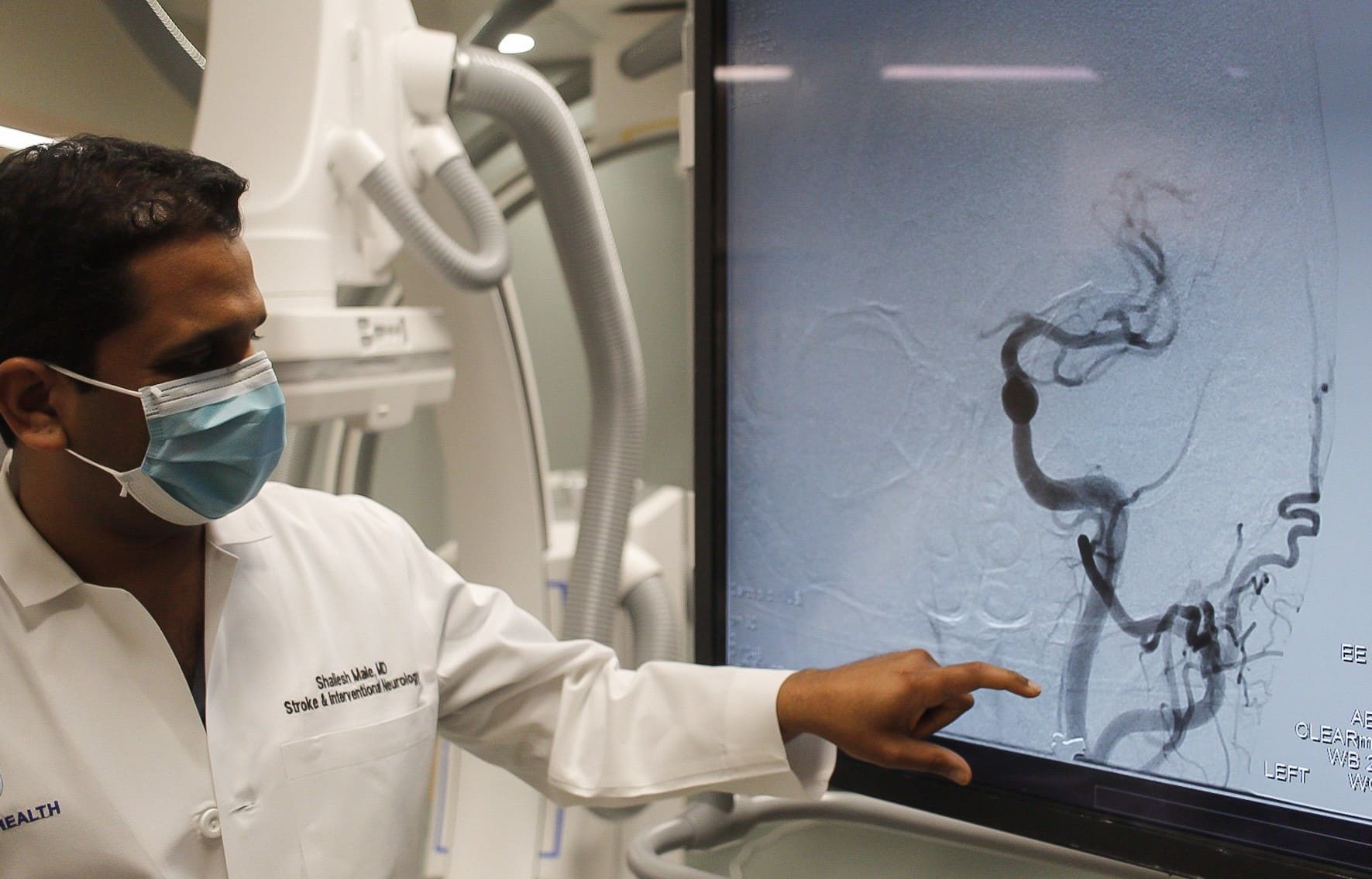
Risk factors for stroke can be broken down into two categories: modifiable and non-modifiable.
“We like to focus on the modifiable risk factors, the ones that you can change,” said Dr. Male. “These include hypertension, cholesterol, diabetes, smoking, physical inactivity and obesity.”
The increase in younger people having strokes are mostly attributed to modifiable risk factors. The rise in popularity of e-cigarettes and vaping has largely been in younger populations. Smoking reduces the amount of oxygen in the blood, makes the heart beat faster and raises blood pressure. Additionally, younger people are generally less healthy than previous generations in terms of diet and exercise.
“Processed, fatty and sugary foods are increasingly becoming a regular part of our diets at a younger age,” said Dr. Male. “This combined with an inactive lifestyle increases almost all risk factors including obesity, diabetes, high blood sugar, hypertension and high cholesterol.”
Non-modifiable risk factors include older age, gender (men face higher risk of stroke), family history, genetics and even race. According to The Office of Minority Health, African Americans are 50 percent more likely to have a stroke than non-Hispanic whites adult counterparts and 70 percent more likely to die from a stroke.
“African Americans have higher incidences of hypertension, diabetes and high cholesterol, which in combination, increases the risk of strokes,” said Dr. Male.
It is important to discuss risk factors with your primary care provider. If you have had a stroke, your doctor may prescribe preventative medications to address risk factors like blood thinners, cholesterol medication or blood pressure medication. Additionally, lifestyle changes such as exercising more and eating healthier foods are proven to lower your risk of stroke.
“With great treatment options now widely available, it is important to remember, time is of the essence,” said Dr. Male. “The sooner we implement treatment, the better the odds that the patient will recover to their baseline. The benefit of early treatment is preventing long-term disability.”
If a stroke is not caught quick enough, long-term disability and health issues are possible. Most commonly, patients may lose strength on one side of their body or have problems speaking.
The acronym B.E. F.A.S.T. can help quickly identify the signs and symptoms that you or a loved one may be experiencing a stroke:
- B – Balance problems
- E – Eye issues like blindness or seeing doubles
- F – Face drooping
- A – Arm weakness
- S – Speech slurring
- T – Time to call 911
In 2000, Millie Shinn developed an ulcer on her right heel. A complication of Shinn’s Type 1 diabetes, the ulcer continued to grow, requiring Shinn to seek treatment and ultimately, a heel reconstruction.
When that did not heal properly, she said she knew amputation was a possibility, though she wasn’t willing to accept it yet. Fast forward to February of 2002 and Shinn was still in bandages from the surgery. After a trip to the Emergency Department, Shinn met with her doctors and they decided it was time to amputate her right leg below the knee.
“My husband was with me and even the nurse that was taking care of me, we were all just bawling before the surgery,” Shinn said of her experience before her first amputation at Vidant Medical Center (VMC). “It was not something that I thought would happen to me … I really wasn’t sure what to expect.”

She said she was motivated after her first surgery to get moving and was lucky to have the opportunity to use an early post-operative prosthesis, or EPOP, which helped her to get out of bed and moving around on a prosthetic limb sooner than she would have without one.
The EPOP was used while she was still healing and about three months after her first surgery, she was fitted with a permanent prosthetic limb. In September of the same year, ulcers began to show up on her left foot. She knew right away how it would end.
She asked what her options were and her providers told her they could continue to clean her ulcers and try to heal her foot for as long as possible. But she told the doctors to move ahead with amputation again.
“I said, ‘I’ve done fine with one fake leg, I’ll be fine with two.’ And that’s what we did,” Shinn said. “It was not circulation issues, it was nerve issues. Circulation was always good I just didn’t have any feeling and had lots of nerve damage.”
Her left leg amputation was also a below-the-knee amputation and she said, like her first amputation, she recovered quickly. Since she knew what to expect the second time around it was not as traumatic an experience—for her. It wasn’t as easy for her son to accept, and at that time, there was not an amputee support group in eastern North Carolina.
Eastern North Carolina Amputee Support Group

Vidant’s amputee support group, officially called Eastern North Carolina Amputee Support Group, came together for the first time in March of 2006 thanks in large part to Shinn and Helen Houston, an occupational therapy clinical specialist at Vidant Medical Center.
Shinn, who lives nearly two hours away from Greenville and made the drive monthly to help lead the support group, said the first meeting had about eight people. The numbers and traditions have grown along the way, and 16 years later the group continues to meet. COVID-19 means they connect virtually on the third Monday of each month from 4:30 to 5:30 p.m.
Shinn said she estimates that nearly 500 people have joined a meeting a one time or another. She has seen the importance of the meetings for her fellow amputees, especially those in the early stages.
“I think it’s very important because they can see us and realize that there is a life afterwards,” Shinn said. “Yes, it has changed my life and yes this is like a death in your family and a death to you because you’ve actually lost a part of yourself. It’s going to be a part of your life, but it doesn’t have to be a controlling part of your life.”
Houston said she has loved her time participating in the group and looks forward to the meeting each month and interacting with people she now considers family. Houston has also helped lead the group since its inception.
She said the conversations each month are inspiring to her and a reminder of why she chose a career in therapy.
“It’s my responsibility, together with recreational therapy, to bring the people that have had recent amputations and are in rehab right now to the group,” Houston said. “We let them see other people that are a little further along than them and let them ask questions. I can answer their questions all day, but I have two legs, so my experience carries limited weight.”
The group frequently has guest speakers including doctors, massage therapists, highway patrol officers, politicians and prosthetists. Shinn said sometimes people will join the group just once to get a few answers to questions that they have and will not return, but she said that as long as people are getting the help they need, the group feels like it is doing its job.
Houston and Shinn both recalled how meaningful it is to include caregivers, family and friends of amputees in the support group sessions. They even shared that in a few cases, after an amputee has passed, spouses and friends continue to attend the sessions to share their insights and past experiences with the group.
“It’s really neat and it’s become like a family,” Houston said. “For me, who is from South Africa, and who doesn’t have family here, to see the same people every month for 16 years, they know me better than I know myself. We’ve been through all kinds of stuff together.”
Occupational Therapy Month
Along with Limb Loss and Limb Difference Awareness Month, April is also Occupational Therapy Month. While occupational therapists play crucial roles in many areas across the health system, supporting amputees is a special responsibility.
Houston said in the acute care setting, occupational therapists are often the first people helping to get amputees out of bed. From there, it’s about teaching patients how to do all the things they are used to doing, but in a different way. This includes bathing, dressing, grooming, transferring to and from a toilet, and to and from a tub.
She said patients typically need three months for their wounds to heal and their residual limb to be shaped, before they get a prosthetic limb. They would initially be at a wheelchair level—or wheelchair and walker level—for some time during their recovery.
“In inpatient rehab, amputees practice self-care tasks, but they also address what we call instrumental activities of daily living,” Houston said. “That is not just self-care but also taking care of the things in your environment. So that would be things like cooking, grocery shopping, money management, medication management, yardwork and starting to access the community, including returning to driving.”
She described the stages after this as getting people back to doing whatever occupied their time before their amputation and educating them on different ways to do so. Houston mentioned a study of healthy adults that showed it takes at least two days to regain strength from each day spent lying in bed.
“That’s for someone who has not had surgery and has not had anything wrong with them,” Houston said. “So here at Vidant we help to get patients up the day after surgery. You’re trying to prevent blood clots, and help them mentally adjust to their new life. The longer you lay there and are fearful of ‘How am I going to get up and how am I going to do this?’ the bigger the mountain seems.”
Houston said her experiences with amputees are often the most inspiring.
“It’s really neat. It’s an honor to be part of their journey,” Houston said. “To be a part of one of the patient’s hardest times in their lives and be able to support them and show them a little further down the road, makes coming to work every day extremely rewarding. To be able to show them that they’re not the only ones in their current situation and to help them to problem solve how they’re able to get back to doing whatever is important to them – that is why I became an occupational therapist.”
Resources
Two Vidant leaders were recognized on Friday, March 18 and inducted into the East Carolina University (ECU) College of Nursing Hall of Fame along with seven other recipients.
Dr. Julie Kennedy Oehlert, chief experience officer at Vidant Health, and Dr. Kamilah Williams, administrator for nursing professional practice, development and clinical education at ECU Health Medical Center (VMC), were each honored last week after being nominated by colleagues and accepted into the ECU College of Nursing Hall of Fame.
Dr. Williams is a 2005 graduate of the ECU College of Nursing and an eastern North Carolina native. She said she is proud to serve the community she calls home and the induction was a great honor.

“I’m so humbled and proud to be a Pirate nurse,” Dr. Williams said. “I’m proud to give back to my community here in eastern North Carolina, where I grew up as a young child. It’s an honor to serve and care for the population that I grew up with. I’m just grateful.”
Dr. Williams is tasked with developing nurses in her role at Vidant. Under her leadership, VMC achieved accreditation for the Nurse Residency Program and has developed an International Nurse Fellowship Program.
She said she loves what she does and is happy to give back to her profession and region through her role.
“When I think about the mission of our organization and being able to improve the health of the people here in eastern North Carolina, it’s exactly why I do what I do,” Dr. Williams said. “As a young child, I always knew I wanted to be a nurse and be able to give back to my community. Now in my role, to be able to help develop future nurses, it’s just a humbling experience.”
Dr. Julie Oehlert has used her experience as a nurse to improve the experience of patients, families and Vidant team members across eastern North Carolina. Dr. Oehlert came to Vidant and eastern North Carolina in 2016 and said the recognition made her feel at home.
“For me, I was so humbled and excited to be recognized with other Pirate Nurses,” Dr. Oehlert said. “I came from outside of Vidant but my heart is with Vidant and ECU. I feel welcomed into this community. I was so overwhelmed when I was nominated and accepted.”
Dr. Oehlert said she is proud to be part of a health system with so many Registered Nurses as leaders in different areas. With nurses in non-traditional roles lending their health care expertise and compassion for patients and families, the nursing heart can be seen in many facets of the health system.
“I don’t get to work directly with nursing but the nursing heart of all the leaders that have RNs behind their name, is pretty darn special at Vidant,” Dr. Oehlert said. “Many of our presidents and executives have that RN heart and that means we are always caring about our communities, we always have a holistic view on care and I love that.”
With the nine inductees for 2022, the ECU College of Nursing Hall of Fame that started in 2011 has grown to 150 members.
One of the past inductees on hand for the event was Dr. Daphne Brewington, senior vice president nurse executive at ECU Health Medical Center.
“It’s just been an amazing night and both Dr. Williams and Dr. Oehlert are so deserving of this award,” Dr. Brewington said. “I’m so proud that they have been inducted into the ECU College of Nursing Hall of Fame. I was inducted in 2018 so it’s just really special and surreal to be able to support colleagues that are on this journey as well.”
Inductees into the Hall of Fame also help fund a scholarship for ECU College of Nursing students, which has raised $170,000 throughout the years to support the next generation of nurses.
Learn more about the ECU College of Nursing Hall of Fame on ECU’s website.
February may be American Heart Month, but it is important to be aware of heart health all year long. During the pandemic, many people may have delayed or postponed heart screenings, which can negatively impact their health. Nearly a quarter of deaths in the United States are caused by heart disease. Although this is a staggering statistic, heart disease is often preventable with lifestyle modifications and medicines.
There are key factors that impact heart health that everyone should be aware of to maintain a healthy cardiovascular system. Risk factors are conditions that heighten your risk of heart attack, stroke and death. Some, like aging and genetics, can’t be controlled, but others can:
- Elevated blood pressure, or hypertension, is sometimes referred to as a silent killer because it doesn’t cause symptoms and accounts for most cardiovascular deaths because of its prevalence.
- Cholesterol levels, especially LDL — the bad cholesterol — can play a key role in buildup of plaque and blockages inside our blood vessels, increasing the risk of stroke and heart attack. About one third of US adults have a high LDL level (>130mg/dl). When it comes to cholesterol and blood pressure, lower is better.
- Diabetes is a major risk factor for heart disease that is heavily influenced by lifestyle. About 12% of adults in the U.S. are diabetic, and an alarming 30% are pre-diabetic. Aggressive control of blood pressure and cholesterol is especially important in diabetics.
- Smoking is a leading preventable cause of disease, disability and death (cardiac and otherwise) in the U.S. Almost one third of coronary deaths are related to smoking and second-hand exposure.

One of the most important ways to prevent heart disease is to control your risk factors and adopt a healthy lifestyle throughout life.
“An ounce of prevention is worth a pound of cure. Being proactive about your heart health is the best way to prevent and manage heart disease,” said Dr. Rony Shammas, interventional cardiologist and hypertension specialist for Vidant Health. “Plaque buildup in the blood vessels starts early on in life, even in our teens, so it is important to address your risk factors and adopt a healthy lifestyle as soon as you can.”
Positive changes in lifestyle that make an impact on heart health include:
- Diet: Eating a well-balanced diet that is rich in fruits, vegetables, nuts, legumes and whole-grains, and low in salt, saturated and trans fats, red meat and sweets and sugar-sweetened beverages promotes good heart health.
- Exercise (Physical Activity): The American Heart Association recommends at least 150 minutes per week of moderate intensity exercise. Almost half of adults do not meet the minimum recommendations for exercise. The American Heart Association recommends at least 150 minutes per week of moderate intensity exercise (i.e., brisk walking).
- Limit alcohol: If you don’t drink, don’t start. Otherwise, keep it to a minimum and don’t exceed one drink a day if you are a woman and two drinks a day for men ( 1 drink= 12oz beer, 5oz wine or 1.5 oz liquor)
- Managing stress: Some stress is good, but excessive stress can be damaging to the body. Breathing techniques, meditation, owning a pet and practicing yoga can help deal with stress.
Depending on your particular risk profile, your health care provider will decide if there is a need for medication to treat blood pressure, cholesterol and diabetes alongside lifestyle changes. If your doctor recommends medication, make sure you take it as prescribed.
Dr. Shammas advises that if you or a loved one suspect you may be having a heart attack or stroke, call 911. Immediate intervention can save your life and reduce your risk of disability. On the other hand, If you are having less acute but concerning symptoms seek medical attention early. After listening to your story and performing an exam, your doctor may order one of several diagnostic tests to decide if your symptoms are related to heart disease.
“Everybody wants to stay off my operating table, and these tips are key for heart disease prevention and helping minimize harmful conditions,” said Dr. Michael Bates, chief and clinical professor of cardiothoracic surgery at the Brody School of Medicine at East Carolina University and ECU Health Medical Center.
When someone is experiencing concerning symptoms, it is key to seek medical attention early. Patients are offered several diagnostic tests when they report symptoms like severe chest pains.
Noninvasive tests can be performed early in a patient’s heart history to look for signs of heart issues. Some of these include a stress test, an exercise stress test performed on a treadmill, which shows how your heart works during physical activity. During this time, your heart rate, blood pressure and the heart’s electrical signals will be monitored. Other noninvasive tests include an echocardiogram, which checks how the heart chambers and valves are pumping blood through your heart.
If heart surgery is needed, today’s advancement in surgical treatments have resulted in less invasive procedures and much faster recovery time than even ten years ago. Some surgeries can be performed through smaller incisions in the body with cameras. Robotic surgery also helps to make less invasive surgeries possible.
There are several less invasive surgeries for the heart. Bypasses can now be performed with assistance from robotic surgery through a smaller incision in the body. Cardiac catheterizations are used to repair the heart valves without making an incision in the chest cavity; instead, the procedure can be performed through arteries and veins.
“Bringing Vidant Health and the Brody School of Medicine together as Vidant Health will continue to extend our mission as a leader in rural health care,” Dr. Bates said. “This collaboration of excellence and combined resources will create even more advancements in our work in cardiac and vascular care.”
Dr. Shammas believes eastern North Carolina’s future is bright because of the outlook for Vidant Health.
“Ultimately, our hope is to make hearts healthier throughout the region and moving forward as Vidant Health strengthens our commitment and mission to bring the best in research and care to the communities we call home,” he said.
One of the most important things you can do for your heart health is to see your provider for screenings and check-ups, which are key to preventing problems before they arise. For more information about cardiovascular resources at Vidant Health, including treatments and technologies, visit www.ecuhealth.org and the Heart & Vascular Care section of the website.

